Best of the 2015 AUA Annual Meeting
Highlights From the 2015 American Urological Association Annual Meeting, May 15-19, 2015, New Orleans, LA
[ Rev Urol. 2015;17(3):179-189 doi:10.3909/riu0681]
© 2015 MedReviews®, LLC
Best of the 2015 AUA Annual Meeting
Highlights From the 2015 American Urological Association Annual Meeting, May 15-19, 2015, New Orleans, LA
[ Rev Urol. 2015;17(3):179-189 doi:10.3909/riu0681]
© 2015 MedReviews®, LLC
Best of the 2015 AUA Annual Meeting
Highlights From the 2015 American Urological Association Annual Meeting, May 15-19, 2015, New Orleans, LA
[ Rev Urol. 2015;17(3):179-189 doi:10.3909/riu0681]
© 2015 MedReviews®, LLC
Key words
Patient phenotyping • Chronic pelvic pain syndrome • EXO106 test • MRI/US fusion biopsy • Oxalobacter formigenes • Ureteroscopic stone removal • 4Kscore • Prolaris • Decipher assay • Stress urinary incontinence • Radiation cystitis • Active surveillance • Occult tethered cord syndrome • Hypospadias • MRI-guided biopsy
Key words
Patient phenotyping • Chronic pelvic pain syndrome • EXO106 test • MRI/US fusion biopsy • Oxalobacter formigenes • Ureteroscopic stone removal • 4Kscore • Prolaris • Decipher assay • Stress urinary incontinence • Radiation cystitis • Active surveillance • Occult tethered cord syndrome • Hypospadias • MRI-guided biopsy
Reviewed by J. Curtis Nickel, MD, FRCSC, Queen’s University, Kingston, Ontario, Canada; Michael A. Gorin, MD, and Alan W. Partin, MD, PhD, Johns Hopkins Medical Institutions, Baltimore, MD; Dean Assimos, MD, University of Alabama at Birmingham School of Medicine, Birmingham, AL; Michael Brawer, MD, URIDEA, Seattle, WA; Heinz Nicolai, Escuela de Medicina, Universidad de Chile, Santiago, Chile; Michael B. Chancellor, MD, William Beaumont Hospital, Royal Oak, MI; Áine Goggins, School of Medicine, Queen’s University, Belfast, and Guy’s & St. Thomas’ NHS Foundation Trust, London, United Kingdom; Stacy Loeb, MD, New York University and the Manhattan Veterans Affairs Medical Center, New York, NY; Ellen Shapiro, MD, FACS, FAAP, New York University School of Medicine, New York, NY.
… chronic pelvic pain may be associated with an altered fecal microbiome in patients with IC.
… in-bore biopsy options offer an exciting alternative to MRI/US fusion and may aid in the evaluation of men with a negative first biopsy result.
Ultrasonic propulsion of stones has been previously demonstrated to be a promising technology in in-vitro studies and in animal models.
… the cell-cycle progression test allows improved and more precise prognostic characterization of patients for appropriate treatment selection.
… liposomal tacrolimus may be a promising new intravesical therapy for the rare, serious condition of radiation cystitis.
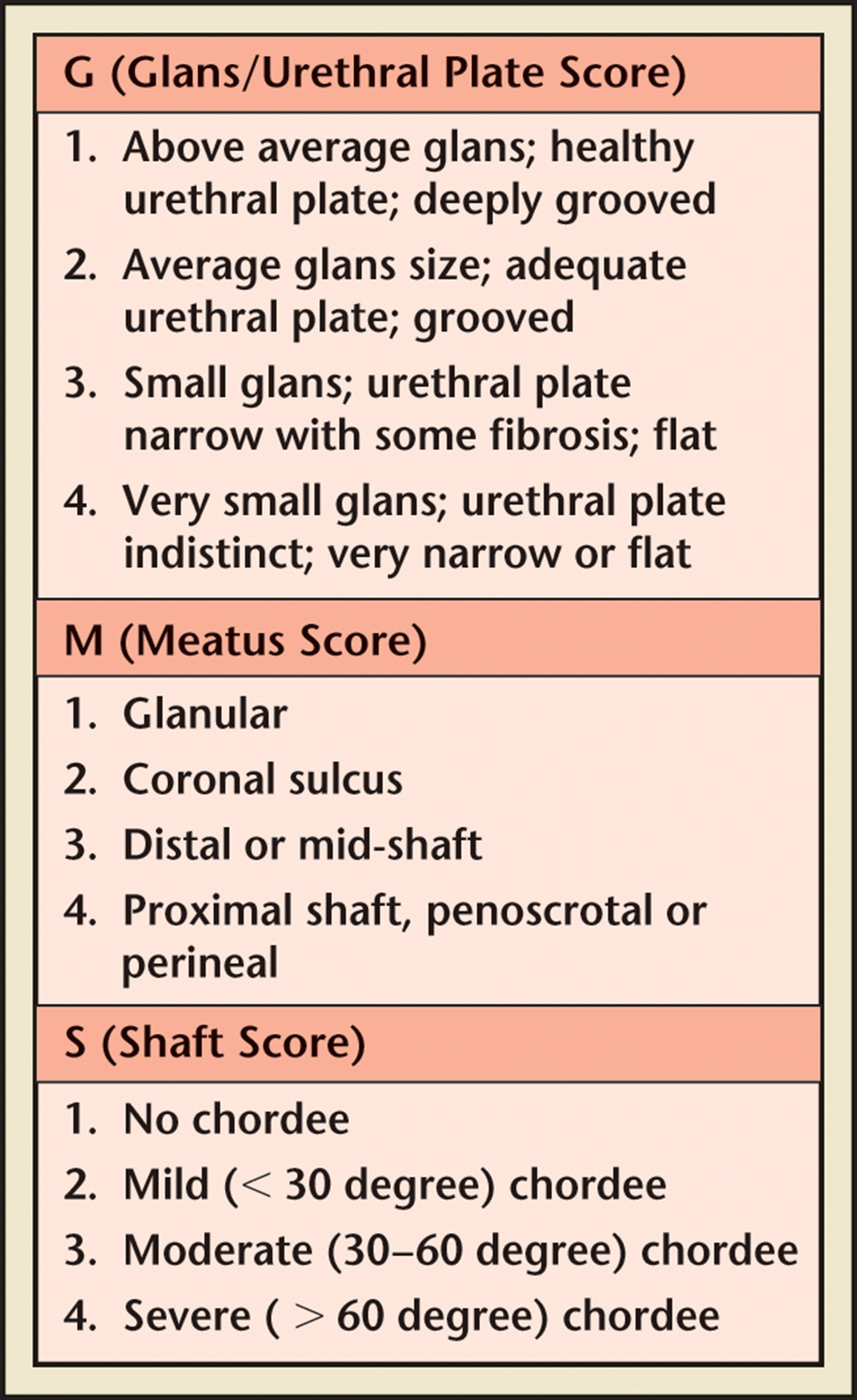
Figure 1. Glans-Urethral Meatus-Shaft score on a Likert scale of 1 to 4. Reprinted with permission from Arlen AM et al.44
At the 2015 American Urological Association (AUA) Annual Meeting, held in New Orleans, Louisiana, from May 15 to 19, 2015, more than 2000 posters, abstracts, and videos were presented. The editors of Reviews in Urology have culled an enormous volume of information from this premier source and present those findings that are most relevant to the practicing urologist.
Urologic Chronic Pelvic Pain Syndrome (Chronic Prostatitis and Interstitial Cystitis/Bladder Pain Syndrome)
One of the principal themes noted during the 2015 AUA meeting was the repeated illustration of the importance of clinically phenotyping patients to assist in development of individualized treatment strategies. Nickel and colleagues,1 by pooling the results of three small, underpowered treatment studies, examining tanezumab, a humanized monoclonal antibody that combines nerve growth factor and inhibits nerve growth factor signaling, showed that women with interstitial cystitis/bladder pain syndrome (IC/BPS) were significantly more responsive to tanezumab than male patients with urologic chronic pelvic pain (primarily chronic prostatitis/chronic pelvic pain syndrome). The analysis further showed an increased treatment effect in patients with less severe symptoms, less depression, and associations with systemic chronic pain conditions. These findings further validate the ongoing research and clinical directions toward improving patient outcomes by individualizing specific treatment strategies based on each patient’s unique clinical phenotypes. It further validates the observation by the National Institutes of Health Multidisciplinary Approach to Pelvic Pain (NIH MAPP) group that a clinical differentiation between patients with pelvic pain only and pelvic pain with other complications is clinically important.
Kleinhans and colleagues2 suggested that altered brain function detectable by functional magnetic resonance imaging (MRI) may further help differentiate patient phenotyping by determining the presence of central nervous system alterations. This unique study recruited 10 female twin pairs who were discordant for urologic chronic pelvic pain syndrome-like symptoms and determined specific differences in the processing of urinary sensation in specific areas of the central nervous system.
Two studies3,4 showed that both transurethral fulguration and endoscopic injection of triamcinolone, respectively, led to significant amelioration of symptoms in patients with this difficult condition. These two papers further confirmed that phenotyping patients, in this case into two clinically distinct categories—those with Hunner’s lesion disease and those without—can lead to improved outcomes in patients with IC/BPS.
This theme of patient differentiation into clinical phenotypes was further described during a plenary session on the topic of urologic chronic pelvic pain in men.5 The take-home message from this panel discussion was that urologists do not need to be afraid to see these patients. With a simple algorithmic approach differentiating the patients by a simple U-POINT (urinary, psychosocial, organ specific, infection, neurologic/systemic, tenderness of skeletal muscles) classification system and directing best evidence treatment toward individual patient phenotypes, most patients will do well. However, a cure may not be possible and the urologist must set realistic goals for both the physician and the patient. These should include not necessarily cure but amelioration of symptoms, increase in activities, and improvement in quality of life.
The other major theme with respect to urologic chronic pelvic pain syndromes was the influence and impact of the microbiome (bowel, vaginal, and bladder) on the symptoms of urologic chronic pelvic pain. Klumpp and associates6 identified statistically significant features in the microbiome detected in stool and vaginal swabs that discriminated patients with IC from control subjects. The authors suggested that chronic pelvic pain may be associated with an altered fecal microbiome in patients with IC. The theme of microbiome and its impact on chronic pelvic pain was this year’s topic at the Society for Infection and Inflammation in Urology, which met on Sunday afternoon under the chairmanship of Dr. Dean Tripp. Dr. Daniel Shoskes presented early work from his patients at the Cleveland Clinic (Cleveland, OH) that again suggested an alteration in the colon microbiota in men with chronic pelvic pain syndrome compared with asymptomatic men. Dr. Michael Freeman presented an interesting and provocative talk entitled “Urinary Tract Microbiome: What We Think We Know.” His major concern was that the increase in megadata will require complex statistical solutions to determine roles and causality. Dr. Jennifer Anger discussed “The Urinary Tract Microbiome: What We Are Learning From Next Generation Technologies,” in which she developed the thesis that the microbiome may be important in the initiation and propagation of IC/BPS and chronic prostatitis/chronic pelvic pain syndrome. She presented the initial exciting findings from the Microbiome Research Group at Cedars-Sinai (Los Angeles, CA) that pointed to differences detected in catheterized urine specimens from patients with IC/BPS compared with control subjects. She also described the initial findings from the NIH MAPP infectious etiology study, which further showed subtle differences between the microbiota of patients with urologic chronic pelvic pain, in both men and women and asymptomatic control subjects. She went on to describe the upcoming microbiome project of the NIH MAPP-2 Symptom Patterns Study. Stay tuned for future developments in this exciting field. There is no doubt that the two major themes from this year’s AUA, patient phenotyping (either clinically or preferably with biomarkers) and continued study on the relationship of our human microbiome and urologic chronic pelvic pain syndromes, will be the topics of future AUA meetings. ![]()
[J. Curtis Nickel, MD, FRCSC]
Clinically Localized Prostate Cancer
Hot topics in the world of prostate cancer included the use of MRI to improve the accuracy of prostate biopsy, molecular diagnostics to help guide patient management, and the use of novel antiandrogens and other systemic therapies in men with castrate-resistant prostate cancer. Specifically within the field of clinically localized prostate cancer, one topic that received considerable attention was how to best manage men with a negative biopsy who continue to be at risk for occult prostate cancer.
Defining the scope of the problem, Telang and associates7 presented data from the Michigan Urological Surgery Improvement Collaborative (MUSIC) demonstrating that, among 6812 men who underwent a first-time prostate biopsy, 47% had no evidence of cancer, yet 6% of this group went on to have a repeat biopsy. Remarkably, 38% of patients who had a second biopsy were ultimately diagnosed with prostate cancer. These data highlight the fact that a significant number of men who have a negative initial biopsy result will have concerning clinical features prompting a repeat biopsy. Additionally, a noninsignificant number of men in this group will harbor occult prostate cancer missed on initial biopsy. How to decide which patients need a repeat biopsy remains a considerable clinical challenge and was the subject of a number of other abstracts at the meeting.
Underscoring the difficulty of using existing clinical parameters to determine which patients need a repeat biopsy, Hadjipavlou and colleagues8 evaluated the role of digital rectal examination (DRE) for predicting the likelihood of prostate cancer on subsequent biopsy. The authors found that an abnormal DRE result was not predictive of a future diagnosis of Gleason score ≤ 7 prostate cancer, but was associated with the risk of Gleason score ≥ 8 disease (23.1% vs 5.4%). Although highly specific for high-grade prostate cancer (90.8%), the sensitivity was quite low (16.9%), limiting the clinical utility of this clinical parameter.
Further demonstrating the inadequacy of clinical data for helping to determine which patients are in need of a repeat biopsy, Sterling and coworkers9 reported that although total prostate-specific antigen (PSA) level, PSA velocity, and race were predictive of finding cancer on first biopsy, these parameters had no predictive role on repeat biopsy.
Moving beyond readily available clinical parameters, Partin and collaborators10 examined the utility of incorporating the methylation profile of three genes, GSTP1, APC, and RASSF1 (MDxHealth, Irvine, CA), into a model for predicting clinically significant prostate cancer (defined as Gleason score ≥ 7 cancer) in men with a previously negative prostate biopsy result. In total, 803 patients formed the study cohort. Of these patients, 179 (22.3%) went on to have a repeat positive biopsy result, 67 (37.4%) of whom had Gleason score ≥ 7 in their biopsy specimen. A model that included the epigenetic profile, patient age, PSA level, and the presence of atypical cells resulted in an area under the curve of 0.80. Compared with current clinically used variables, the methylation profile alone resulted in an increased positive predictive value for the detection of clinically significant cancer.
In another study evaluating molecular markers of prostate cancer, McKiernan and collaborators11 evaluated the utility of the EXO106 test (Exosome Diagnostics, Cambridge, MA), a urine-based assay that utilizes real-time reverse transcription polymerase chain reaction to measure the expression of three genes (ERG, PCA3, and SPDEF) for detecting Gleason score ≥ 7 cancer at the time of prostate biopsy. Of note, all patients in this study had PSA values of 2 to 10 ng/mL—values commonly found in men with a negative first biopsy result. The authors found that the EXO106 test, when used in combination with commonly used clinical variables, including PSA, age, race, and family history, resulted in a significantly improved area under the curve (AUC, 0.72; 95% confidence interval [CI], 0.68-0.77) as compared with clinical variables alone (0.63; 95% CI, 0.58-0.68; P < .00004). Use of this gene signature had excellent performance for predicating Gleason score > 7 cancer, including a negative predictive value of 91%, and a positive predictive value of 36%.
In addition to abstracts evaluating novel molecular tests, a considerable number focused on the use of MRI-ultrasound (US) fusion biopsy to improve the accuracy of standard transrectal US (TRUS)-guided biopsy. In a podium presentation, George and colleagues,12 from the National Cancer Institute, utilized a Bayesian analysis to model the likelihood of harboring clinically significant prostate cancer (defined as Gleason score ≥ 4 + 3 = 7) following a 12-core and/or MRI/US fusion biopsy revealing low-grade or no cancer. The authors reported a modeled likelihood of 46% for harboring clinically significant prostate cancer following standard 12-core biopsy that revealed no, or clinically insignificant, cancer. In contrast, if a targeted biopsy was performed with MRI/US fusion, this risk dropped to 24%. Remarkably, if a targeted biopsy was performed in addition to a 12-core biopsy, the risk decreased to only 11%. In agreement with these findings, Mendhiratta and associates13 reported that the cancer detection rate on repeat biopsy for men with ≥ 1 negative prior biopsy result was 23.7% with MRI/US fusion as compared with 17.3% with standard biopsy alone (P = .09). Additionally, the authors found significantly less Gleason score ≥ 7 cancer was missed with the use of fusion biopsy (0% vs 47%; P < .001). Based on these combined data, the use of MRI/US fusion target biopsy appears to significantly increase the negative predictive value for clinically significant cancer if a first biopsy demonstrates low-grade or no cancer.
As an alternative to MRI/US fusion, Felker and coworkers14 evaluated the efficacy of in-bore MRI-guided biopsy. In this study the authors performed biopsies using an MRI-compatible needle guide known as DynaTRIM (Invivo, Gainesville, FL) following lesion identification with multiparametric MRI. The authors presented data on 511 patients who underwent biopsy at three different centers. Patients underwent a biopsy for a number of different indications, including an elevated PSA level (75%), active surveillance (AS) for an existing diagnosis of prostate cancer (16%), or for a suspected recurrence (9%). Notably, 238 (46.6%) of patients in the study had a prior negative biopsy result. DynaTRIM-guided biopsy resulted in a positive biopsy result in 51% of patients, with 83% of biopsies detecting clinically significant cancer (defined as Gleason score ≥ 3+4). Moreover, 33% of men with a prior negative TRUS-guided biopsy result had a positive result on MRI-guided biopsy. A fully automated version of an MRI-compatible biopsy system was also presented by Ball and coworkers15 at the Engineering and Urology Society section of the meeting. Combined, these two in-bore biopsy options offer an exciting alternative to MRI/US fusion and may aid in the evaluation of men with a negative first biopsy result. ![]()
[Michael A. Gorin, MD, Alan W. Partin, MD, PhD]
Kidney Stones
Several excellent presentations on the subject of kidney stones addressed basic and translational science and clinical research studies.
There is an ongoing epidemic of obesity in the United States and other parts of the world. A number of patients with morbid obesity are subjected to Roux-en-Y gastric bypass for weight reduction. Although this procedure has been demonstrated to improve survival in this cohort, patients are subject to the development of kidney stones and even renal failure due to excessive excretion of urinary oxalate. Canales and Hatch16 undertook a study in which this procedure was performed in rats; they compared sham-operated animals, bypassed animals colonized (intestinal) with the oxalate degrading organism Oxalobacter formigenes, and noncolonized bypassed rats. Oxalate excretion was lowest in the sham-treated animals. The bypassed, colonized animals had substantially lower oxalate excretion as compared with the noncolonized group. A substantial number of bypassed patients are not colonized with this organism. This study suggests that O formigenes colonization of this cohort may prove to be beneficial.
Patients with sterile urine who are subjected to percutaneous nephrolithotomy (PCNL) are still at risk for sepsis. This is attributed to stones laden with unsuspected bacteria, which has been reported to be present in 25% of these cases. Prior studies have demonstrated that the administration of a 1-week course of either ciprofloxacin or nitrofurantoin in those with sterile urine substantially decreases the risk of sepsis/systemic inflammatory response syndrome (SIRS). Larson and colleagues17 performed a retrospective study of 140 patients with sterile urine subjected to PCNL who were considered high risk (prior urinary tract infection, hydronephrosis, or stone burden > 2 cm). They performed univariate and multivariate regression modeling and found that the occurrence of SIRS was similar in those receiving a 7-day course of preoperative antibiotic therapy, 2 days of treatment, or just antibiotics administered on the day of the procedure. This demonstrates that further studies are needed to determine the actual benefit of preoperative antibiotic therapy in this cohort.
Ureteroscopic stone removal is now the most commonly employed approach for stone removal in North America and other areas of the world. Improvements in technology have permitted effective removal of moderate- to large-sized renal stones. Some surgeons endorse laser fragmentation to small particles without extraction (dusting), and others prefer active fragment removal. Chew and colleagues18 performed a multicenter study in which patients with 2- to 20-mm renal stones underwent either “dusting” or active fragment removal. All subjects receive an α-blocker for 30 days after the procedure, and stents were placed at the end of every procedure. Procedural length was longer in the active extraction cohort but the stone-free rate was substantially higher (89.9% vs 60.9%). There were no differences in readmission or reintervention among the groups; however, I predict that with longer follow-up periods those harboring residual stones will have subsequent stone events, some requiring a stone-removing procedure. Thus, I currently endorse active fragment removal if feasible.
Medical therapy has been demonstrated to reduce stone activity and stone events. Compliance with this type of therapy has been thought to be important. Dauw and colleagues19 analyzed a group of 8950 patients with kidney stones who were prescribed thiazide diuretics, alkali citrate, or allopurinol for stone prevention, all of whom had a minimum of 2 years of follow-up. They found that 56.6% were compliant, using a formula of proportion of days covered. A multivariate analysis demonstrated that those who were compliant had a 25% lower incidence of emergency room visits, 30% lower incidence of hospitalization, and 13% lower requirement of a subsequent stone-removing procedure. These findings demonstrate the importance of compliance with such medical therapy as this undoubtedly has a positive impact on quality of life and economic health.
Tamsulosin is commonly used for medical expulsive therapy in patients with ureteral stones. It was not approved for this purpose, and thus is an off-label application of the agent. Pregnant patients with ureteral stones can be a challenge to manage; thus, facilitating stone passage is desirable. The Food and Drug Administration considers tamsulosin a category B medication. Its safety has not been demonstrated in pregnant patients. Bailey and associates20 performed a retrospective study of 28 pregnant patients with suspected ureteral stones who were treated with tamsulosin, for a median length of treatment of 3 days (range 1-110 d). A matched cohort analysis demonstrated no significant difference in maternal or fetal outcomes. The mean follow-up after delivery was 20.8 months. Of note, the 2 infants in the tamsulosin group died of sudden infant death syndrome. Although these results suggest that tamsulosin therapy for medical expulsive therapy in pregnant patients may be safe, this has not been adequately validated.
The majority of patients with renal colic are cared for in an emergency room setting. Scales and colleagues21 performed a cross-sectional analysis of patients with suspected kidney stones who received treatment in an emergency room from 2007 to 2010 using the National Hospital Ambulatory Medical Care Survey; this analysis comprised almost 5 million patient visits. They report that proper imaging was done in only 63% of patients, whereas appropriate laboratory testing was done in 40% of cases. In addition, only 17% of patients were prescribed medical expulsive therapy, which is consistent with rates previously reported. This study clearly demonstrates that emergency room care of patients with suspected kidney stones needs to be improved.
Ultrasonic propulsion of stones has been previously demonstrated to be a promising technology in in-vitro studies and in animal models. Harper and associates22 reported its use in 15 adult humans with renal stones 1 to 13 mm in size. All targeted stones were visualized and there was some degree of stone movement in 14 of the patients. It proved especially useful in patients with stone fragments after shock wave lithotripsy. Only two patients noted discomfort during these manipulations. This technology continues to show promise and will be a useful future adjunct for stone management.
Burst wave lithotripsy is a new technology that may prove to be an effective method of extracorporeal stone fragmentation. Maxwell and colleagues23 performed an in vitro study of this technology using artificial kidney stones, in addition to an in vivo experiment with a porcine model. The device that they used was a 330 kHz US transducer with a focal length of 12 cm. The stones were localized with US and US energy bursts were directed at the targeted calculi. Excellent fragmentation was achieved in an in vitro setting. They were able to detect areas of renal injury using B-Mode US that developed in the porcine kidney during therapy. This technology appears promising but more work is needed to define its efficacy and safety.
The studies profiled here are reflective of some of the advancements that are being made in the care of patients with kidney stones. In addition, these presentations point out areas in which care needs to be improved. ![]()
[Dean G. Assimos, MD]
Prostate Markers
Prostate markers were once again a major offering at the 2015 AUA meeting. Several important studies of prognostic markers are highlighted here.
The 4Kscore test (OPKO Lab, Nashville, TN) measures 4 kallikreins and appears to be more specific than measurement of PSA levels alone. Punnen and colleagues,24 in a multi-institution trial, sought to determine if this assay could predict adverse pathology at radical prostatectomy (RP). They studied men with Gleason score 6 cancer on biopsy. The 4Kscore was associated with the number and percent of positive cores, and the length of cancer on the cores (all P < .0002); 51 men underwent immediate RP. The 4Kscore predicted upgrading (median 4Kscore in men without upgrading was 7 vs 15 for those who did upgrade; P = .023). This study indicates that, in addition to being a test that improves on the specificity of PSA for detection, it may be useful in understanding a cancer’s malignant potential. Further study is warranted, especially to assess its ability to identify intermediate- or high-risk cancers that behave less aggressively. Prolaris® (Myriad Genetics Laboratories, Salt Lake City, UT) is a prostate cancer prognostic marker based on cell cycle progression genes. It has been validated in multiple clinical scenarios and is the dominant predictor of biochemical recurrence, metastases, or disease-specific mortality. Cuzick and associates25 established a cutoff combining Cancer of the Prostate Risk Assessment (CAPRA) and the Prolaris score (CCR) for men who are currently considered candidates for AS. A threshold CCR was established in 505 men such that 90% of men with PSA < 10 ng/ mL, stage ≤ T2b, Gleason score ≤ 3+4, and with < 25% of cores positive had a CCR below this. This was validated in two cohorts of men who were initiated on conservative management and followed for > 10 years with disease-specific mortality being the endpoint.
For the combined cohort, the 10-year risk of prostate cancer mortality at the threshold was 3.2%. There were no observed prostate cancer deaths in patients below the threshold. The cutoff was then used to assess the impact on over 4000 men undergoing commercial Prolaris testing; 35% of men had clinicopathologic parameters noted above and were candidates for AS. By using the CCR cutoff of 0.8, 60% of men had cancer of low malignant potential and were suitable candidates for conservative management. For patients considering deferred treatment, the CCR score provides significant prognostic information at disease diagnosis.
Clinical utility (the ability of a prognostic test to change therapy) is now considered by payers to be as important as assay safety and validity. Shore and associates26 investigated Prolaris scores in a utility registry. Clinicians who were experienced with the test were asked how they would manage the patient before and after receiving the report; 1206 men were evaluated.
The test significantly influenced joint decision making toward appropriate personalized treatment. Prolaris testing caused a change in treatment for 48% patients in this study, 72% of whom had decreased treatment burden. Among 417 men initially recommended to receive noninterventional therapy, 24% were changed to intervention as a result of a higher Prolaris score. Conversely, among 789 men initially scheduled for intervention, 14.2% received noninterventional care. This study shows that the cell-cycle progression test allows improved and more precise prognostic characterization of patients for appropriate treatment selection.
Whalen and colleagues27 examined the Oncotype DX® (Genomic Health, Redwood City, CA) test in men being treated at Columbia University (New York, NY). Among 95 men, they observed reclassification of risk group in 44.1%. However, only 5 men (7.6%) moved from low or very low risk to so-called “low intermediate” risk; 11 men in the low intermediate group moved into the low-risk strata (36.6%). Among 50 men undergoing RP, none in whom the test predicted more favorable pathology had stage pT3 or primary Gleason score 4 or 5 cancer. Oncologic endpoints (biochemical recurrence, metastases) were not reported.
Katz and colleagues28 reported on the first 4000 men commercially tested with the Oncotype DX test. Reclassification from National Comprehensive Cancer Network low or very low risk to low intermediate risk (PSA 10-20 ng/mL, stage cT2b-c, Gleason score 3 + 4, ≤ 3 cores positive, and < 50% of cores positive) occurred in 176 of 2609 patients (6.8%); 156 of 1207 men (12.4%) who were at low intermediate risk were reclassified to low or very low risk. The difference between this larger cohort and the study by Whalen and colleagues27 may be a result of selection bias in the latter.
The Decipher® test (GenomeDx, Vancouver, British Columbia) is a molecular prognostic test performed on RP tissue. In a study of men undergoing RP, Ross and coworkers29 reported on 260 intermediate- or high-risk men who were followed without adjuvant or salvage therapy before evidence of metastases. The Decipher score was significantly higher among men who developed metastases (0.47 vs 0.28, respectively; P < .001), and the risk of metastases increased by 48% for every 10% increase in the Decipher score. Despite lack of definitive data suggesting improvement in disease-specific mortality in adjuvant versus salvage therapy, these data suggest utilization of the test in higher-risk men for consideration of adjuvant therapy.
Yamoah and coauthors30 studied the Decipher assay in African American (154) and European American (243) men with prostate cancer. Previous studies have called into question the utility of standard clinicopathologic parameters in African Americans. Importantly, Decipher was validated to predict metastasis within 5 years after bRP in both African American (AUC = 0.78) and European American men AUC = 0.88). The reasons for the differences need further investigation. ![]()
[Michael Brawer, MD]
Dr. Brawer is Vice President of Medical Affairs at Myriad Genetics Laboratories.
Epidemiology of Stress Urinary Incontinence Treatment and the Rising Importance of Radiation Cystitis
The group from the Cleveland Clinic reported an excellent retrospective study to assess the rate of reoperation for stress urinary incontinence (SUI) after revision of a synthetic midurethral sling (MUS) that is causing obstruction. The study by Abraham and colleagues31 evaluated the effect of time from sling placement to sling revision on reoperation rates. The secondary objective was to assess rates of persistent and de novo stress incontinence. Women who underwent revision of synthetic MUS from 2005 to 2013 were reviewed and completed surgical satisfaction questionnaires. Multivariable logistic regression analysis was used to evaluate the association between time to sling revision and reoperation for SUI.
The authors reported inclusion of 107 women and the reoperation rate for SUI was 14% (15/107). The median time was 22 months between initial surgery and sling revision; 49% and 77% reported de novo and persistent SUI, respectively, and 83% of these women reported they were moderately or quite a bit bothered by their SUI.
The authors noted that, on multivariable analysis, women were significantly less likely to have reoperation for SUI when sling revision was performed > 24 months after the initial sling was placed compared with within 3 months. The high degree of bother with the low reoperation rate for SUI suggests women wanted to avoid additional surgery. This nicely presented research may be helpful for clinicians interested in female urology in counseling selective women after surgical repair of SUI.
Liu and associates32 presented on a topic that is rapidly changing and also of high importance for all urologists given the recent establishment of certification in Female Pelvic Medicine and Reconstructive Surgery (FPMRS). The purpose of the study was to assess female urology surgical case volume characteristics before and after FPMRS certification.
Surgical logs for 6 months of certifying urologists between 2003 and 2013 were obtained from the American Board of Urology with focus on five procedure groups: incontinence, prolapse, vesicovaginal fistula (VVF), ureteral reimplant, and revision/removal of vaginal mesh/graft. Among 4802 urologists (442 women and 4360 men) logging at least one female urology case, 43,949 (54% of all cases) incontinence, 30,983 (38%) prolapse, 451 (1%) VVF, 3643 (4%) revision of mesh/graft, and 3497 (4%) ureteral reimplant surgeries were identified. With initiation of the FPMRS certification process, logs between 2011 and 2013, 225 FPMRS candidates (13% of certifying urologists) were identified, compared with 367 (10%) of urologists prior to 2011 who identify themselves as primarily female subspecialists.
Women accounted for only 5% of certifying urologists in 2004. However, by 2013, 13% were women urologists, logging 38% of prolapse repairs and 35% of mesh/graft revisions. The number and proportion of women certifying in female urology subspecialty have increased, shifting from only 2% in 2004 to almost half of certifying female subspecialists (43%) in 2013.
The authors concluded that a growing proportion of female urologic cases are performed by women subspecialists, with a significant increase since 2011 and the start of FPMRS certification. Female surgeons account for a disproportionate volume, despite remaining a minority of certifying urologists and female subspecialists.
Rajaganapathy and colleagues33 presented a new model to induce radiation cystitis and the first pharmacotherapy that may help this rare but severe disease. In collaboration with radiation oncology specialists, a small animal radiation research platform targeted bladder irradiation with computed tomography guidance. The irradiated rats were assessed serially in metabolic cages to determinate micturition pattern and subsequently treated with instillation of a liposomal formulation of tacrolimus.
Hemorrhagic radiation cystitis is a rare and serious disease from pelvic radiation and chemotherapy and has no approved drug treatment. Liposome-encapsulated tacrolimus is a potential immunosuppressant and arteriole constrictor that may increase endocytosis and decrease toxicity, although systemic administration has a high incidence of adverse events.
In the first phase of the study, rats were exposed to dose escalation of radiation to optimize modeling, and in the second phase the selected 40 Gy radiation was used to test drug effect. Irradiated rats were randomly assigned to receive a single instillation of saline or liposomal tacrolimus. The 40 Gy radiation dose induced statistically significant reductions in the intermicturition interval compared with the lower radiation doses. Histologic analysis revealed degenerative epithelial changes and urothelial swelling with evidence of pseudocarcinomatous epithelial hyperplasia. There was no measurable change in total voided urine volume after irradiation, or after liposomal tacrolimus or saline instillation. Liposomal tacrolimus significantly increased the postirradiation intermicturition interval by approximately 30 minutes back to baseline (P < .001).
The radiation cystitis rat model showed a dose-dependent decrease in the intermicturition interval without inducing short-term skin or gastrointestinal damage. This study demonstrates that liposomal tacrolimus may be a promising new intravesical therapy for the rare, serious condition of radiation cystitis. Further studies are needed to analyze the effect of liposomal tacrolimus on hemorrhagic cystitis. ![]()
[Heinz Nicolai, MD, Michael B. Chancellor, MD]
AS for Prostate Cancer
A major highlight of the program was the wealth of data showing an increase in the use of AS in the management of localized prostate cancer. One of the countries with the highest rates of AS is Sweden, where the National Prostate Cancer Register has complete data on 98% of cases nationwide. Loeb and associates34 previously reported that, from 2007 to 2011, AS was selected as primary management for 59% of very low-risk, 41% of low-risk, and 16% of intermediate-risk prostate cancer cases nationwide. At the 2015 AUA meeting they presented updated data through 2013, showing a significant increase in AS use in both the very low-risk and low-risk categories, up to 84% and 66%, respectively.35 In both risk categories, AS use increased across all age groups: those < 60 years, 60 to 70 years, and those > 70 years (P < .05 for all). However, utilization of AS for intermediate-risk cases remained more limited, at 18% in 2013. Finally, among men in Sweden diagnosed with prostate cancer who would meet six published AS selection criteria (Sunnybrook Heath Sciences Centre [Toronto, Ontario], Memorial Sloan Kettering Hospital [New York, NY], Princess Margaret Cancer Centre [Toronto], University of California, San Francisco, Prostate Cancer Research International Active Surveillance [PRIAS], and Johns Hopkins Hospital [Baltimore, MD]), they reported that 64% to 85% of individuals actually received AS.
A retrospective study of eight community-based urology practices by Shelton and colleagues36 from Large Urology Group Practice Associations (LUGPA) identified 1401 patients, 17.3% of whom had very low-36.1% who had low- and 42.7% who had intermediate-risk disease. Overall, 70.2% of very low, 39.2% of low, and 7.7% of intermediate-risk patients received AS. Risk group, age, and urology practice were significant predictors of primary therapeutic choice (all P < .001), whereas race was not (P = .43). The authors suggested that the notable variation in AS utilization between practices could therefore represent an opportunity for educational interventions.
In a prospective study of 539 patients with low-risk prostate cancer, Kim and associates37 observed an increase in the utilization of AS from 6% from 2006 to 2008, to 18% between 2009 and 2011, up to 37% from 2012 to 2014. During a median follow-up of 20 months, 13% of these men went on to receive definitive treatment. Using validated questionnaires, they showed a low frequency of decisional regret but a significant decline in sexual function over time among men on AS.
Cooperberg and associates38 reported an update on practice patterns in 10,924 men from the University of California, San Francisco Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE™) registry, which includes more than 40 clinical practice sites nationwide. They found that 38.9% of low-risk patients received watchful waiting (WW) or AS for primary management from 2010 to 2013, compared with only 9.5% between 2005 and 2009. Predictors of initial treatment by WW/AS were year of diagnosis in 2010 or later versus 1990 to 2009 (odds ratio [OR] 10.9; 95% CI, 7.2-16.4), age (OR 1.2; 95% CI, 1.17-1.22), and CAPRA score (OR 0.54; 95% CI, 0.50-0.58).
The proportion of men undergoing AS may also be affected by differences in patient inclusion criteria. For example, in the Princess Margaret Cancer Centre AS program, inclusion criteria are age ≤ 75 years, PSA ≤ 10 ng/mL, clinical stage ≤ T2, Gleason sum ≤ 6, number of positive cores ≤ 3, and no single core > 50% involved. Of 712 men in the program who met these criteria, Komisarenko and colleagues39 reported that instead applying the more restrictive criteria from Johns Hopkins Hospital, PRIAS, and the University of Michigan Comprehensive Cancer Center (Ann Arbor, MI) would have excluded 13.7%, 11.5%, and 8.8% men from undergoing AS, respectively. However, there was no significant difference in biopsy reclassification rates among men meeting these criteria. This suggests that AS eligibility may be unnecessarily reduced by using very restrictive criteria.
Several other studies reported on outcomes of AS. Another study by Komisarenko and colleagues40 of 568 men with low-risk prostate cancer reported that 32% discontinued AS at 5 years. Among men with biopsy reclassification, those with increases in grade were more likely to opt for treatment than those with increases in volume (78.2% vs 64.7%; P < .001). Interestingly, there was no significant difference in pathologic outcomes in those who left AS early without progression (n = 42) and those who left after progression (n = 143), although the sample sizes were small.
Finally, Tosoian and assosciates41 reported on the extended follow-up of 1298 men with favorable-risk prostate cancer enrolled in the Johns Hopkins Hospital AS program. At a median follow-up of 5 years, 36% had received curative treatment and 0.4% developed metastatic disease or died from prostate cancer. The 10- and 15-year overall survival rates were 93.2% and 68.7%, with cancer-specific survival rates of 99.9% and 99.9%, respectively. Freedom from grade reclassification at the same time points was 70.2% and 62.7%, respectively. The cumulative hazard of death from prostate cancer remained at 0.3% (95% CI, 0.1-1.2) at both 10 and 15 years, whereas the risk of death from any cause increased from 7.0% (95% CI, 4.6-9.6) to 27.2% (95% CI, 15.4-46.9). These results provide additional long-term data confirming the safety and durability of AS for favorable-risk disease. ![]()
[Áine Goggins, Stacy Loeb, MD]
Dr. Loeb receives funding from the Laura and Isaac Perlmutter NYU Cancer Center, the Louis Feil Charitable Lead Trust, and the National Institutes of Health (Award Number K07CA178258). The content is solely the responsibility of the authors and does not represent the official views of the NIH.
Pediatric Urology
The 3-day joint AUA and Society of Pediatric Urology meeting included scientific sessions covering complex urinary incontinence, perinatal urology, bladder exstrophy, hypospadias, pediatric tumor, trauma, renal transplantation, varicocele, disorders of sexual differentiation, urinary tract infection, and vesicoureteral reflux. Panel discussions included hypospadias, bladder exstrophy, and socioeconomics. The focus of this AUA pediatric review is on a plenary session presentation and the clinical research abstracts.
John Duckett Memorial Lecture—Minimally Invasive Surgery in Pediatric Urology: Present and Future
Dr. Chung Kwong Yeung reviewed the history of laparoscopic surgery in pediatric urology. Laparoscopic equipment became available for infants in the 1990s.42 The laparoscopic approach has changed the surgical approach to partial nephrectomy of nonfunctioning moieties in duplications, ureteropelvic junction obstruction, and undescended testes. The laparoscopic approach has clear advantages for approaching a prostatic utricle and determining the location of dysplastic kidneys that require nephrectomy due to their ectopic orifices causing incontinence. Looking forward, advances in optical technology will provide improved magnification. Three-dimensional reconstruction will permit preoperative “rehearsal” of the surgery.
Occult Tethered Cord Syndrome
Children with clinical and abnormal urodynamic features suggestive of a neurogenic bladder who have no significant improvement on standard medical management usually undergo an MRI of the spine as the next step in their evaluation. An abnormality of spinal anatomy is rarely found. This group of patients with normal spine anatomy and refractory symptomatology is referred to as having occult tethered cord syndrome (OTCS). Improvement in bladder function has been reported in several uncontrolled studies following division of the filum terminale, even in the absence of MRI findings. MacNeily and coworkers43 presented the results of a pilot study of 21 children with abnormal urodynamic findings refractory to medical management for at least 1 year who had a normal termination of their conus on MRI. These children were randomized to medical management alone versus surgical division of the filum plus medical management. The outcome measures at 1 year following randomization included a validated dysfunctional elimination score, a standardized urodynamic score, and a validated enuresis-specific quality-of-life scale (Pediatric Enuresis Module on Quality of Life™ [PEMQOL; HealthActCHQ, Boston, MA]). The authors found that dysfunctional elimination score improved in both groups (13% medical and 10% surgical) and standardized urodynamic score worsened slightly in the medical (16%) and surgical (5%) groups, but no differences were statistically significant. The surgical group did show greater improvement on the family impact scale of the PEMQOL.
This study shows no difference between the medical alone versus medical and surgical approaches to treating these children who have refractory dysfunctional voiding and a normal lumbosacral MRI result with normal termination of the conus. It is important to note that the study was severely underpowered to show clinically significant differences. Nevertheless, this study, which was the recipient of the first place award, casts doubt on the utility of dividing the filum for OTCS.
Hypospadias
The Glans-Urethral Meatus-Shaft (GMS) score has been used to characterize hypospadias beyond meatal position. Arlen and colleagues44 examined the utility of the GMS score to predict factors contributing to postoperative complications. G = glans size/urethral plate quality; M = meatal location; and S = degree of shaft curvature were assessed using a Likert scale of 1 to 4 (Figure 1). Of the 262 boys (mean age 12.3 ± 13.7 mo) undergoing surgery for hypospadias, the mean overall GMS score was 7 ± 2.5 (G2.1 ± 0.9, M2.4 ± 1, S2.4 ± 1). Postoperative follow-up was a mean of 29.7 ± 9.3 months. During this time, 45 complications occurred in 37 (14.1%) boys. Using a univariate model, G (OR 2.1; 95% CI, 1.45-3.12; P < .0001), M (OR 2.4; 95% CI, 1.62-3.59; P < .0001), and S (OR 2.63; 95% CI, 1.77-3.91; P < .0001) scores all predicted complications. However, in a multivariable model adjusting for length of follow-up, only chordee was statistically significant. The odds of any complication increased by 2.49 times for each 1 point increase in S score, but the M score was not an independent predictor of complications. Urethrocutaneous fistula occurred in 8.8%. The authors show that only the S score was an independent predictor of fistula formation with every unit increase in S score increasing the risk of fistula by 2.37 times. The authors concluded that the severity of curvature is strongly associated with the development of a fistula, as well as other complications following hypospadias repair.
Cancer and Infertility
Fertility preservation for prepubertal boys with cancer remains a challenge because these boys are unable to produce semen for cryopreservation.45 Although germ cells of the prepubertal testis do not yet contain mature spermatozoa, spermatogonial stem cells are present. Theoretically, pretreatment cryopreservation of testicular tissue from prepubertal boys with cancer should be possible with eventual restoration of spermatozoa production after treatment. The objective of this study was to evaluate parental preferences for testis biopsy and other factors in the decision-making process, even though the long-term utility of these biopsies remains unknown. The study recruited oncology providers, parents, and male teenage cancer survivors from three major pediatric centers in Canada. Interviews and surveys were used to determine preferences for testis biopsy, factors influencing decisions, and for disclosure and nondisclosure issues.
Overwhelmingly, families desired information about testicular biopsy at the time of diagnosis (94% of parents [144/153], and 90% of survivors [69/77]). In retrospect, parents and survivors reported feeling angry, disappointed, and confused in response to not being given the option for testicular biopsy. Once biopsies were hypothetically presented to families, all groups preferred biopsy versus no biopsy (110/153 [72%] parents, 22/30 [73%] providers, and 52/77 [68%] survivors), and even more so for survivors when a portion of tissue was donated to research (75%). The authors concluded that parents and survivors of childhood cancer want information about testicular biopsy for potential fertility preservation despite the lack of clinical benefit. Knowledge translation and interventions improving access to information need to be developed and tested. Nondisclosure by providers appears to be a suboptimal long-term strategy. ![]()
[Ellen Shapiro, MD, FACS, FAAP]
References
- Nickel JC, Kreger J, Mills I, et al. Tanezumab reduces pain in women with interstitial cystitis/bladder pain syndrome. J Urol. 2015;193(suppl):e397.
- Kleinhans N, Yang C, Strachan E, et al. Alterations in connectivity on fMRI with provocation of lower urinary tract symptoms in urologic chronic pelvic pain syndromes. J Urol. 2015;193(suppl):e400.
- Kim JH, Kim SW, Jee S, et al. Progressive, multicenter, randomized clinical trial comparing the effect of hydrodistension and transurethral fulguration of bladder in interstitial cystitis/bladder pain syndrome patients. J Urol. 2015;193(suppl):e401.
- Bahlani S, King A, Moldwin R. Endoscopic injection of triamcinolone - a simple, minimally invasive, and effective therapy for Hunner’s lesions. J Urol. 2015;193(suppl):e401-e402.
- Nickel JC, Pontari MA, Shoskes, DA. Chronic pelvic pain syndrome. Panel discussion presented at: American Urological Association Annual Meeting; May 15-19, 2015; New Orleans, LA.
- Klumpp D, Braud Meier-Fleming A, Yaggie R, et al. Altered microbiome in chronic pelvic pain patients. J Urol. 2015;193(suppl):e401.
- Telang D, Liu A, Gao Y, et al. Utilization and outcomes of repeat prostate biopsy in a statewide quality improvement collaborative. J Urol. 2015; 193(suppl):e256.
- Hadjipavlou M, Mohamed A, Sriprasad S, et al. Abnormal digital rectal examination (DRE) of the prostate increases the likelihood of future high grade prostate cancer diagnosis in patients with initial benign prostate biopsy. J Urol. 2015; 193(suppl):e900.
- Sterling WA, Weiss JP, Schreiber D, et al. Is race predictive of a future prostate cancer diagnosis after an initial negative biopsy? J Urol. 2015;193(suppl): e993-e994.
- Partin AW, Van Neste L, Stewart GD, et al. Risk stratification of aggressive prostate cancer based on combined epigenetic and clinical data of men with initial cancer-negative biopsies. J Urol. 2015;193(suppl): e959-e960.
- McKiernan J, Donovan M, O’Neill V, et al. PII-LBA2: Validation of a novel non-invasive urine exosome gene expression assay to predict high-grade prostate cancer in patients undergoing initial biopsy with an equivocal PSA. J Urol. 2015;193(suppl): e495-e496.
- George A, Shakir N, Siddiqui MM, et al. Confidence in biopsy findings in the era of MRI-targeted prostate sampling. J Urol. 2015;193(suppl):e899.
- Mendhiratta N, Rosenkrantz AB, Meng X, et al. Outcomes of MRI-US fusion targeted prostate biopsy in men with history of previous negative biopsy: improved cancer detection and risk stratification. J Urol. 2015;193(suppl):e705.
- Felker E, Lee-Felker S, Feller J, et al. Performance of in-bore MR-guided targeted prostate biopsy for detection of clinically significant prostate cancer: a multicenter study. J Urol. 2015;193(suppl):e827.
- Ball MW, Ross A, Kim C, et al. Safety and feasibility of robot-assisted direct MRI-guided transperineal prostate biopsy. Presented at: Proceedings of the 30th Annual Meeting of the Engineering and Urology Society; May 16, 2015; New Orleans, LA. Abstract 28.
- Canales B, Hatch M. Oxalobacter formigenes colonization normalizes oxalate excretion in a gastric bypass model of hyperoxaluria. J Urol. 2015;193(suppl): e373-e374.
- Larson J, Potretzke A, Desai A, Benway B. Is preoperative antibiotic prophylaxis for high-risk patients necessary before percutaneous nephrolithotomy? A retrospective review of 7 vs 2 vs 0 day therapy. J Urol. 2015;193(suppl):e347-e348.
- Chew BH, Shah O, Sur RL, et al. Dusting vs basketing during ureteroscopic lithotripsy-what is more efficacious? Interim analysis from a multi-centre prospective trial from the Edge Research Consortium. J Urol. 2015;193(suppl):e261-e262.
- Dauw C, Yi Y, Bierle M, et al. Consequences of non-adherence to selective medical therapy among patients with kidney stones. J Urol. 2015;193(suppl):e501.
- Bailey G, Vaughan L, Bergstralh E, et al. Perinatal outcomes with tamsulosin therapy for symptomatic urolithiasis. J Urol. 2015;193(suppl):e501.
- Scales C, Bergman J, Carter S, et al. Quality of acute care for patients with upper tract stones in the United States. J Urol. 2015;193(suppl):e503.
- Harper J, Dunmire B, Cunitz B, et al. Report on the feasibility of ultrasound to reposition kidney stones in humans. J Urol. 2015;193(suppl):e885.
- Maxwell A, Cunitz B, Kreider W, et al. Preclinical image-guided therapy system for burst wave lithotripsy. J Urol. 2015;193(suppl):e886.
- Punnen S, Sjoberg D, Zappala S, Parekh D. The performance of the 4Kscore for predicting high-grade cancer on biopsy of the prostate does not depend on the age of the patient. J Urol. 2015;193(suppl):e740.
- Cuzick J, Stone S, Fisher G, et al. Validation of an active surveillance threshold for the CCP score in conservatively managed men with localized prostate cancer. J Urol. 2015;193(suppl):e4.
- Shore N, Boczko J, Kella N, et al. Significant reduction in therapeutic burden from use of CCP test in treatment decisions among newly diagnosed prostate cancer patients in a large prospective registry. J Urol. 2015;193(suppl):e708.
- Whalen M, McKiernan J, Benson M, Badani K. Prospective correlation between probability of favorable pathology on the 17-gene genomic prostate score and actual pathologic outcomes at radical prostatectomy. J Urol. 2015;193(suppl):e3-e4.
- Katz A, Ho A, Burke E, et al. The 17-gene genomic prostate score (GPS) assay: initial clinical experience of 4,000 patients. J Urol. 2015;193(suppl):e1.
- Ross A, Johnson M, Yousefi K, et al. Validation of the Decipher® prostate cancer classifier in intermediate to high risk men treated with radical prostatectomy but without additional therapy upon PSA rise. J Urol. 2015;193(suppl):e4-e5.
- Yamoah K, Johnson M, Choeurng V, et al. A novel biomarker signature which may predict aggressive disease in African-American men with prostate cancer. J Urol. 2015;193(suppl):e55.
- Abraham N, Makovey I, King A, et al. The effect of time to revision of an obstructing synthetic mid-urethral sling on reoperation for stress urinary incontinence. J Urol. 2015;193(suppl):e646-e647.
- Liu JS, Doolittle J, Hofer MD, et al. Changes in female urologic case distribution with new subspecialty certification and surgeon gender. J Urol. 2015;193(suppl):e1031-e1032.
- Rajaganapathy BR, Janicki J, Levanovich P, et al. Intravesical liposomal tacrolimus protects against radiation cystitis induced by 3-beam targeted bladder radiation. J Urol. 2015;193(suppl):e230.
- Loeb S, Berglund A, Stattin P. Population based study of use and determinants of active surveillance and watchful waiting for low and intermediate risk prostate cancer. J Urol. 2013;190:1742-1749.
- Loeb S, Folkvaljon Y, Bratt O, Robinson D. Expanding use of active surveillance: data from the National Prostate Cancer Register (NPCR) of Sweden. J Urol. 2015;193(suppl):e512.
- Shelton J, Buffington P, Koo A, Shore N. Contemporary active surveillance rates for newly diagnosed prostate cancer patients in community urology practices. J Urol. 2015;193(suppl):e27-e28.
- Kim D, Hurwitz L, Cullen J, et al. Treatment decision-making patterns among low risk prostate cancer patients managed on active surveillance in an equal access health care setting. J Urol. 2015; 193(suppl):e757.
- Cooperberg M, Carroll P. National prostate cancer practice trends: evolving toward evidence-based practice across risk strata. J Urol. 2015;193(suppl): e148.
- Komisarenko M, Timilshina N, Alibhai S, et al. No significant difference in patient outcomes when stricter active surveillance criteria are applied: a comparison of contemporary active surveillance protocols. J Urol. 2015;193(suppl):e508.
- Komisarenko M, Timilshina N, Alibhai S, et al. Use of initial active surveillance among men with low-risk prostate cancer- follow up and follow out. J Urol. 2015;193(suppl):e28-e29.
- Tosoian J, Mamawala M, Epstein J, et al. Prospective longitudinal active surveillance program for favorable-risk prostate cancer: long term. J Urol. 2015;193(suppl):e147.
- Yeung CK. John Duckett Memorial Lecture. Minimally invasive surgery in pediatric urolgy: present and future. Lecture presented at: American Urological Association Annual Meeting; May 15-19, 2015; New Orleans, LA.
- MacNeily A, Steinbok P, Afshar K, Landgraf J. Treatment of persistent urinary incontinence in children with occult tethered cord syndrome by section of the filum terminale: a randomized controlled pilot study. Presented at: Society for Pediatric Urology 63rd Annual Meeting; May 15-19, 2015; New Orleans, LA.
- Arlen AM, Kirsch AJ, Weiss AD, et al. Chordee matters: meatal position may not be the most important feature of the hypospadias complex. Presented at: Society for Pediatric Urology 63rd Annual Meeting; May 15-19, 2015; New Orleans, LA.
- Lorenzo AJ, Donen RM, Maloney AM, et al. Testicular biopsy for fertility preservation in prepubertal boys with cancer: identifying preferences for procedure and barriers to disclosure. Presented at: Society for Pediatric Urology 63rd Annual Meeting; May 15-19, 2015; New Orleans, LA.