Retroperitoneal Ancient Schwannoma: A Case Report
Selahattin Çalişkan, MD,1 Gülistan Gümrükçü, MD,2 Cevdet Kaya, MD1
1Urology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey; 2Pathology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey
Schwannomas are extremely rare tumors that are composed of Schwann cells. Retroperitoneal localization comprises 0.7% to 2.6% of all schwannomas. Patients usually present with nonspecific symptoms. There are no pathognomonic features on radiologic evaluation. Preoperative biopsy is not recommended because of complication risks; however, surgery is necessary for diagnosis and treatment. Although most schwannomas are benign tumors, those that are associated with von Recklinghausen disease are malignant. Schwannomas exhibit regions of high and low cellularity, termed Antoni A and Antoni B areas, with a diffuse positivity of S100 protein on pathologic evaluation. If there are degenerative changes, such as cyst formation, hemorrhage, calcification, and hyalinization, these tumors are termed ancient schwannomas. We present a case of retroperitoneal ancient schwannoma.
[Rev Urol. 2015;17(3):190-193 doi: 10.3909/riu0638]
© 2015 MedReviews®, LLC
Retroperitoneal Ancient Schwannoma: A Case Report
Selahattin Çalişkan, MD,1 Gülistan Gümrükçü, MD,2 Cevdet Kaya, MD1
1Urology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey; 2Pathology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey
Schwannomas are extremely rare tumors that are composed of Schwann cells. Retroperitoneal localization comprises 0.7% to 2.6% of all schwannomas. Patients usually present with nonspecific symptoms. There are no pathognomonic features on radiologic evaluation. Preoperative biopsy is not recommended because of complication risks; however, surgery is necessary for diagnosis and treatment. Although most schwannomas are benign tumors, those that are associated with von Recklinghausen disease are malignant. Schwannomas exhibit regions of high and low cellularity, termed Antoni A and Antoni B areas, with a diffuse positivity of S100 protein on pathologic evaluation. If there are degenerative changes, such as cyst formation, hemorrhage, calcification, and hyalinization, these tumors are termed ancient schwannomas. We present a case of retroperitoneal ancient schwannoma.
[Rev Urol. 2015;17(3):190-193 doi: 10.3909/riu0638]
© 2015 MedReviews®, LLC
Retroperitoneal Ancient Schwannoma: A Case Report
Selahattin Çalişkan, MD,1 Gülistan Gümrükçü, MD,2 Cevdet Kaya, MD1
1Urology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey; 2Pathology Department, Haydarpaşa Numune Training and Research Hospital, Istanbul, Turkey
Schwannomas are extremely rare tumors that are composed of Schwann cells. Retroperitoneal localization comprises 0.7% to 2.6% of all schwannomas. Patients usually present with nonspecific symptoms. There are no pathognomonic features on radiologic evaluation. Preoperative biopsy is not recommended because of complication risks; however, surgery is necessary for diagnosis and treatment. Although most schwannomas are benign tumors, those that are associated with von Recklinghausen disease are malignant. Schwannomas exhibit regions of high and low cellularity, termed Antoni A and Antoni B areas, with a diffuse positivity of S100 protein on pathologic evaluation. If there are degenerative changes, such as cyst formation, hemorrhage, calcification, and hyalinization, these tumors are termed ancient schwannomas. We present a case of retroperitoneal ancient schwannoma.
[Rev Urol. 2015;17(3):190-193 doi: 10.3909/riu0638]
© 2015 MedReviews®, LLC
Key words
Retroperitoneal schwannoma • Neurilemmoma • Schwannoma • Retroperitoneal tumor • Retroperitoneum
Key words
Retroperitoneal schwannoma • Neurilemmoma • Schwannoma • Retroperitoneal tumor • Retroperitoneum
Retroperitoneal localization accounts for 0.75% to 2.6% of all schwannomas; most are found in the limbs, head, and neck.
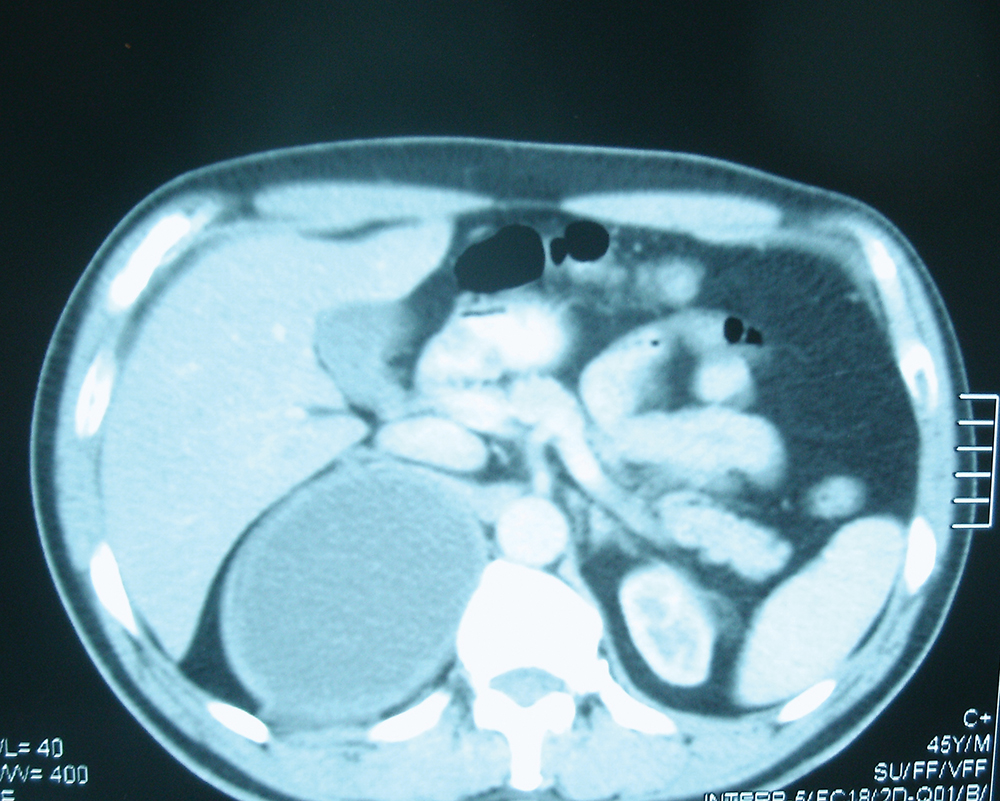
Figure 1. Image of retroperitoneal mass on computerized tomography.
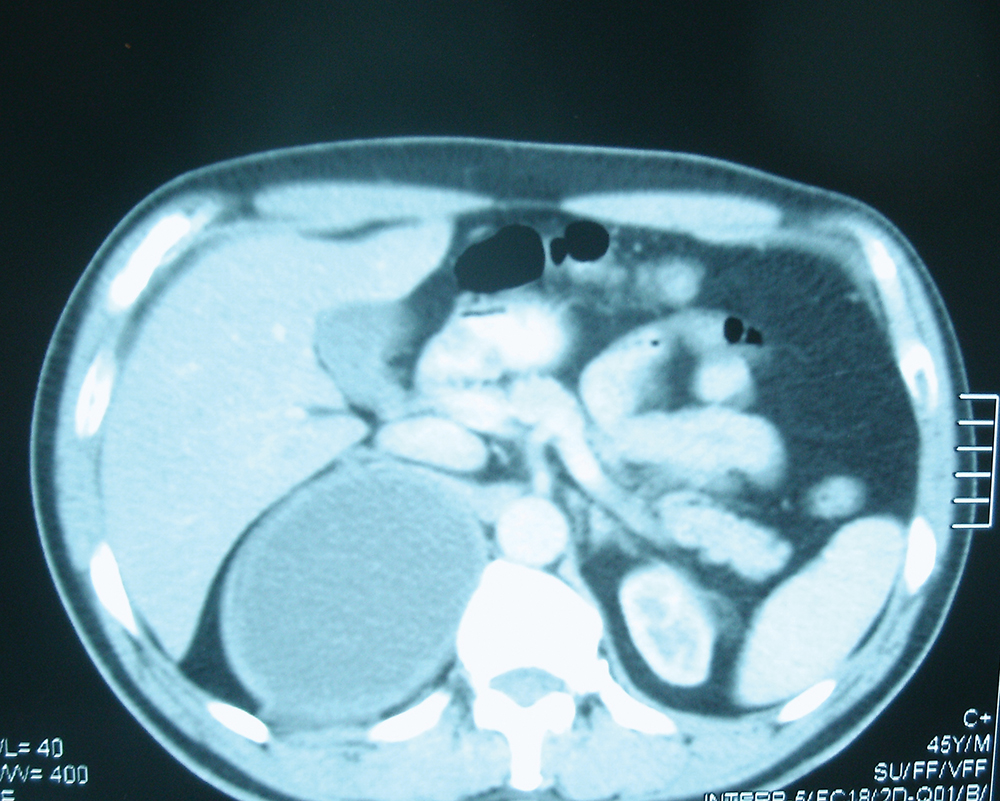
Figure 1. Image of retroperitoneal mass on computerized tomography.
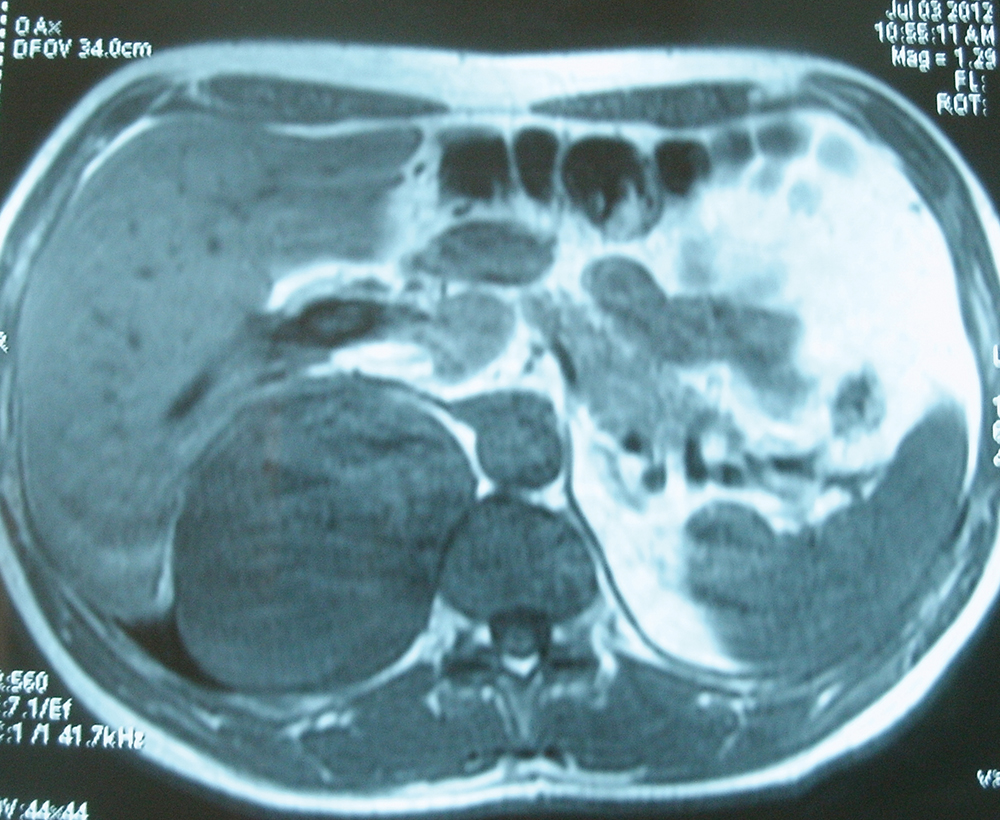
Figure 2. Magnetic resonance imaging of the retroperitoneal mass.
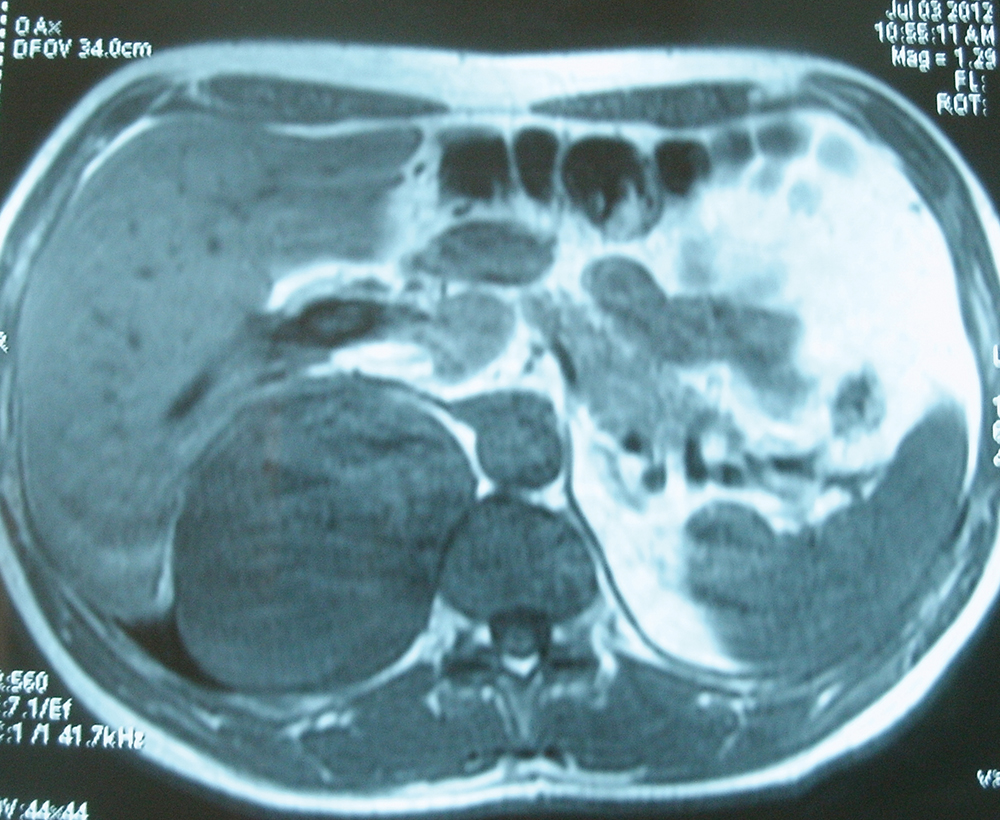
Figure 2. Magnetic resonance imaging of the retroperitoneal mass.
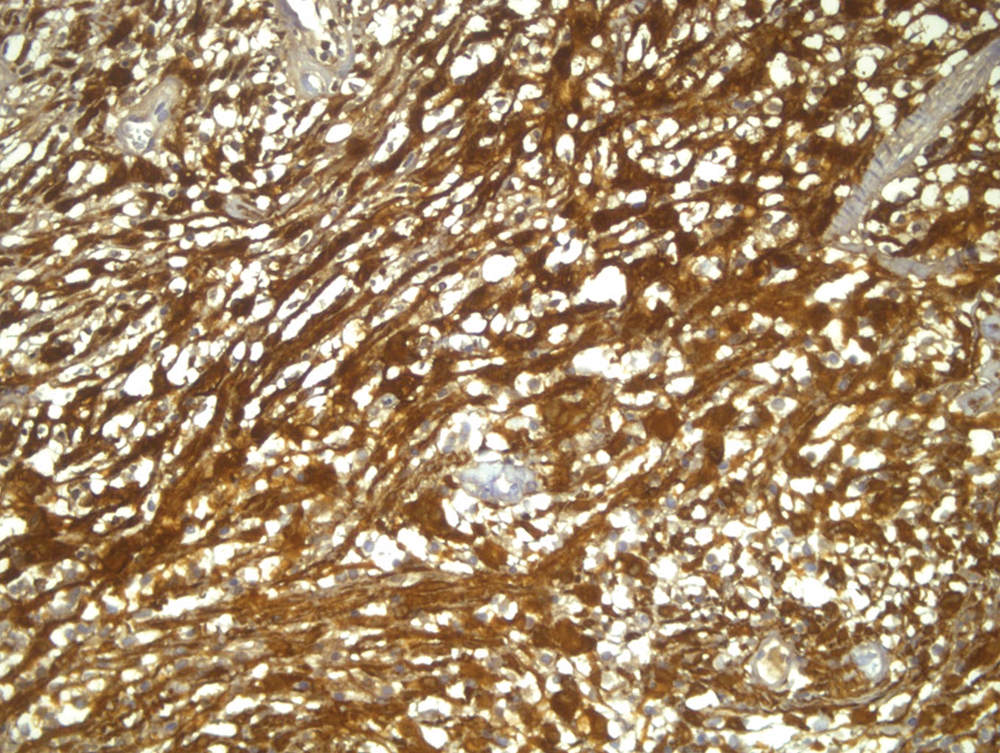
Figure 3. Positive staining of the schwannoma with S100 protein (original magnification, 1003).
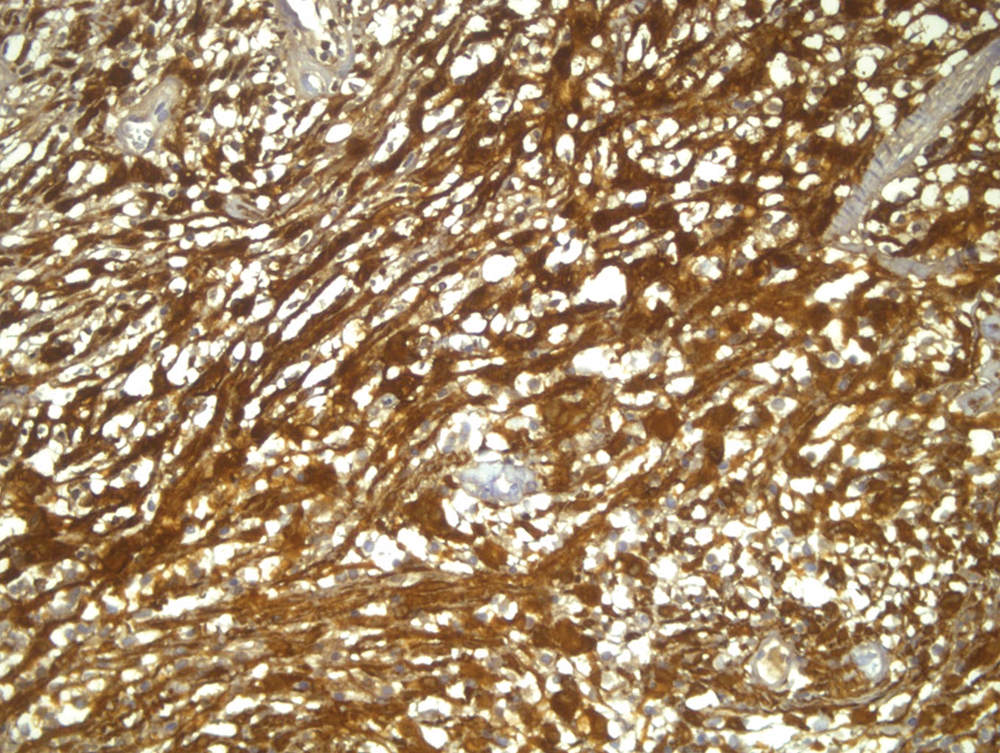
Figure 3. Positive staining of the schwannoma with S100 protein (original magnification, 1003).
Symptoms include vague abdominal pain, flank pain, hematuria, headache, secondary hypertension, and recurrent renal colic pain.
Complete surgical resection is recommended, because malignancy cannot be excluded preoperatively…
Main Points
• Retroperitoneal schwannomas are rare tumors, and account for approximately 1% to 5% of all retroperitoneal masses. Most are located in the limbs, head, and neck. Retroperitoneal schwannomas are usually solid, encapsulated tumors and originate from the paravertebral region, and have a greater tendency to undergo spontaneous degeneration and hemorrhage compared with those that arise in the head, neck, and extremities.
• If degenerative changes are present, such as cyst formation, hemorrhage, calcification, and hyalinization, these tumors are termed ancient schwannomas.
• Retroperitoneal schwannomas are diffIcult to diagnose preoperatively. CT-guided biopsy and fine-needle aspiration are reliable for diagnosis. Magnetic resonance imaging can be used to image large retroperitoneal tumors, because of better visualization of the tumor’s origin, vascular architecture, and involvement of other organs.
• Although some investigators advocate complete excision, including the sacrifice of adjacent tissue, others believe that simple enucleation or partial excision is sufficient. We believe the best treatment of retroperitoneal schwannoma is complete excision because malignancy cannot be excluded preoperatively.
Main Points
• Retroperitoneal schwannomas are rare tumors, and account for approximately 1% to 5% of all retroperitoneal masses. Most are located in the limbs, head, and neck. Retroperitoneal schwannomas are usually solid, encapsulated tumors and originate from the paravertebral region, and have a greater tendency to undergo spontaneous degeneration and hemorrhage compared with those that arise in the head, neck, and extremities.
• If degenerative changes are present, such as cyst formation, hemorrhage, calcification, and hyalinization, these tumors are termed ancient schwannomas.
• Retroperitoneal schwannomas are diffIcult to diagnose preoperatively. CT-guided biopsy and fine-needle aspiration are reliable for diagnosis. Magnetic resonance imaging can be used to image large retroperitoneal tumors, because of better visualization of the tumor’s origin, vascular architecture, and involvement of other organs.
• Although some investigators advocate complete excision, including the sacrifice of adjacent tissue, others believe that simple enucleation or partial excision is sufficient. We believe the best treatment of retroperitoneal schwannoma is complete excision because malignancy cannot be excluded preoperatively.
Aschwannoma is a tumor of the Schwann cell or nerve cell sheath.1 This tumor may occur anywhere there is a nerve with Schwann cells—predominantly in the head and neck region, or flexor surfaces of the extremities. Most schwannomas are benign tumors2; however, malignant schwannomas may be associated with von Recklinghausen disease.3 Retroperitoneal schwannomas are usually larger than those in other sites, and have a greater tendency to undergo spontaneous degeneration and hemorrhage when compared with head, neck, and extremity locations.4 We present a case of a retroperitoneal schwannoma that was reported to be an ancient schwannoma on pathologic evaluation.
Case Report
A 45-year-old man presented with right back pain that was present for 1 month. Laboratory test results were within normal ranges. Ultrasonography revealed a 141 × 130 × 80-mm cystic mass that localized near the adrenal glands and the liver. Computerized tomography (CT) showed a 12 × 10 × 10-cm cystic mass that localized near the kidney and liver (Figure 1). Contrast-enhanced T1- and T2-weighted magnetic resonance imaging (MRI) on the capsule revealed an 82 × 116-mm cystic mass with retroperitoneal localization (Figure 2). After this evaluation the patient underwent laparotomy. The mass was excised via an open transperitoneal technique. The mass was localized between the left adrenal gland and the liver; no complications occurred in pre- or postoperative periods. Macroscopically, an 8 × 8 × 6-cm capsulated cystic mass was pathologically evaluated. Histologic examination revealed Antoni A and B areas with positive staining for S100 protein (Figure 3). Because of the cyst formation, an ancient schwannoma was reported. No recurrence and metastasis were detected on postoperative CT after 6 months. The patient did not have any complaints during follow-up at 9 months.
Discussion
Retroperitoneal schwannomas are rare tumors that comprise approximately 1% to 5% of all retroperitoneal masses.4 Retroperitoneal localization accounts for 0.75% to 2.6% of all schwannomas5,6; most are found in the limbs, head, and neck.7 Retroperitoneal schwannomas are usually solid, encapsulated tumors and originate from the paravertebral region.4 Macroscopically, schwannomas are solitary, well-circumscribed, firm, and smooth-surfaced tumors.7 Retroperitoneal schwannomas are larger and have a greater tendency to undergo spontaneous degeneration and hemorrhage compared with those that arise in the head, neck, and extremities.4
Patients are typically diagnosed between ages 40 and 60 years, with a ratio of 2:3 between men and women.7 Diagnosis of retroperitoneal schwannomas is very diffıcult. A study from Singapore reported that symptoms were nonspecific, and neurologic symptoms were rare.4 Symptoms include vague abdominal pain, flank pain, hematuria, headache, secondary hypertension, and recurrent renal colic pain.7 Preoperative diagnosis is difficult, because of the absence of pathognomonic features.4 Ultrasonography is both a useful and inexpensive modality for detecting this tumor. CT scans can reveal well-defined low or mixed attenuation with cystic necrotic central areas. Cystic changes are seen more commonly in retroperitoneal schwannomas than in other retroperitoneal tumors.7 MRI can be used to image large retroperitoneal tumors because of better visualization of the tumor’s origin, vascular architecture, and involvement of other organs.4
CT-guided biopsy and fine-needle aspiration are reliable for diagnosis of retroperitoneal schwannomas.7 CT-guided biopsy may be helpful if the sample contains sufficient Schwann cells for microscopic visualization. Many investigators do not recommend preoperative biopsy as a diagnostic tool, because of the risks of hemorrhage, infection, and tumor seeding.8
The differential diagnosis of retroperitoneal schwannomas includes neurofibroma, paraganglioma, pheochromocytoma, liposarcoma, malignant fibrous histiocytoma, lymphangioma, and hematoma.4 The best treatment of retroperitoneal schwannoma is complete excision in healthy patients. Considerable controversy exists over negative soft tissue margins, especially when adjacent tissue or viscera need to be sacrificed.8 Some investigators advocate complete excision, if necessary, including the sacrifice of adjacent tissue.8,9 Others believe that simple enucleation or partial excision is sufficient.10 Local recurrence rates range from 16% to 54% after conservative intralesional enucleation. Complete surgical resection is recommended because malignancy cannot be excluded preoperatively with frozen section analysis.7 Laparoscopy is a safe and effective treatment modality for schwannomas, because it offers better visualization in narrow anatomic spaces.6
Histologically, schwannomas are composed of Schwann cells with regions of high and low cellularity termed Antoni A and Antoni B areas, with a diffuse positivity of S100 protein.4 The presence of degenerative changes, such as cyst formation, hemorrhage, calcification, and hyalinization, classifies these tumors as ancient schwannomas. Microscopically, Antoni A and B areas, and S100 positivity with cyst formation were seen in our case.
Retroperitoneal schwannomas are very rare and diffıcult to diagnose preoperatively. The best treatment of schwannomas is complete surgical excision. Although malignant transformations have been reported, the prognosis of retroperitoneal schwannomas is extremely good. Careful monitoring is suggested after surgery. ![]()
References
- Guo YK, Yang ZG, Li Y, et al. Uncommon adrenal masses: CT and MRI features with histopathologic correlation. Eur J Radiol. 2007;62:359-370.
- Geol H, Kim DW, Kim TH, et al. Laparoscopic partial cystectomy for schwannoma of urinary bladder: case report. J Endourol. 2005;19:303-306.
- Sharma SK, Koleski FC, Husain AN, et al. Retroperitoneal schwannoma mimicking an adrenal lesion. World J Urol. 2002;20:232-233.
- Goh BK, Tan YM, Chung YF, et al. Retroperitoneal schwannoma. Am J Surg. 2006;192:14-18.
- Deshmukh SN, Agarwal SG, Bolde SA, Shah VR. Retroperitoneal schwannoma: common tumour in an uncommon place. Sri Lanka J Surg. 2013;31:59-60.
- Okuyama T, Tagaya N, Saito K, et al. Laparoscopic resection of a retroperitoneal pelvic schwannoma [published online January 8, 2014]. J Surg Case Rep. doi: 10.1093/jscr/rjt122
- Cury J, Coelho RF, Srougi M. Retroperitoneal schwannoma: case series and literature review. Clinics (Sao Paulo). 2007;62:359-362.
- Daneshmand S, Youssefzadeh D, Chamine K, et al. Benign retroperitoneal schwannoma: a case series and review of the literature. Urology. 2003;62:993-997.
- Guz BV, Wood DP Jr, Montie JE, Pontes JE. Retroperitoneal neural sheath tumors: Cleveland Clinic experience. J Urol. 1989;142:1434-1437.
- Miller PL, Tessler A, Alexander S, Pinck BD. Retroperitoneal neurilemmoma. Urology. 1978;11: 619-623.