Transitioning to ICD-10: Steps for Urologists and Urology Groups
Jonathan Rubenstein, MD
Chesapeake Urology Associates, Baltimore, MD
[Rev Urol. 2014;16(1):44-46 doi: 10.3909/riu0614]
© 2014 MedReviews®, LLC
On October 1, 2015, the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) will replace the ICD-9 for coding used for all medical encounters in the United States. This is a massive shift that could be financially devastating for those providers and groups that are underprepared. For successful implementation, all aspects of the medical practice must be appropriately prepared: providers, office staff, billing staff, the electronic medical record system, practice management system, clearinghouse, and payors. The 1-year delay from October 1, 2014 should only encourage us to continue pushing forward with ICD-10 training now, not to merely delay it a year.
Training
Understanding the specificity of ICD-10 and documentation requirements is of utmost importance. ICD-10 is not just an “expansion” of ICD-9 with more specificity; rather, it has its own unique structure with unique billing rules. Those who try to convert ICD-9 into ICD-10 will find significant frustrations. Rather, providers should learn ICD-10 as a unique system.
Understanding ICD-10, how it is set up, and its rules are the key to a successful transition. Training should involve everyone in the practice, from those who are involved in the initiation of patient care (eg, call center, front desk, triage), to those directly involved in patient care (eg, providers and assistants, electronic medical record administrators), to those who are involved in billing and payment for services (billing staff). Training should be tailored toward the roles in the group; physicians and other providers might merely need to know documentation details based upon the code sets, whereas billing staff will need to understand in greater detail the codes themselves along with the exclusion and sequencing rules.
ICD-10 Specificity
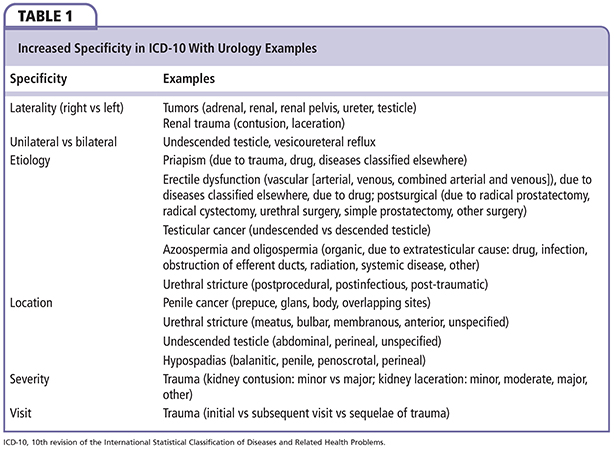
Coding convention for ICD-10 has a number of unique rules and coding conventions. Although a significant number of codes do have a 1:1 correlation between the two code sets, ICD-10 contains many areas of increased specificity, including details about laterality, etiology, location, severity, and visit (ie, initial visit, subsequent visit, and visit for sequelae of the condition). Not all conditions need these levels of specificity. A summary of the details that are specific for common urology conditions, although not an exhaustive list, can be found in Table 1.
In addition, the coding convention and rules must be followed for correct coding. Note that the correct code choice is that which is of the highest level of specificity, and in cases where a specific code exists, that code must be chosen; it is not proper to use an “unspecified” code for ease of code choice when a specific code for the condition exists.
Laterality
In urology coding, the main areas in which laterality (left versus right) needs to be documented for correct code choice are benign and malignant genital and urinary neoplasms (kidney, renal pelvis, ureter, and testicle) and renal trauma (contusion and laceration). There are almost no other urology codes that contain laterality. To highlight this example, consider C64, malignant neoplasm of the kidney, except renal pelvis. C64 itself is not a billable code as this condition is further subclassified into three more specific (billable) codes: C64.1, malignant neoplasm of the right kidney, except renal pelvis; C64.2, malignant neoplasm of the left kidney, except renal pelvis; and C64.9, malignant neoplasm of unspecified kidney, except renal pelvis. There are no codes describing the location within the kidney, the size of the tumor, the type of tumor, severity, or underlying condition. If one knows the side of the tumor, then the specific code should be used; it is not proper to choose the “unspecified” code for convenience if laterality is known. Because there is no “bilateral” code, if a patient has malignant neoplasms of both the right and left kidney, both ICD-10 codes should be chosen.
Etiology
Documenting the underlying etiology of several urologic conditions is necessary for correct coding. Some examples include the cause of a patient’s priapism (eg, due to drug, due to trauma, due to underlying condition, or unspecified cause). It is not proper to choose the “unspecified” cause for priapism if the etiology is due to a drug (eg, intracavernosal injection or α-blocker), due to trauma, or due to an underlying condition (eg, sickle cell or lymphoma). Other common urologic conditions where etiology is necessary for proper coding include azoospermia and oligospermia, erectile dysfunction, testicular cancer, and urethral stricture.
Location
Conditions such as penile cancer, urethral stricture, undescended testicle, and hypospadias require information about the location of the condition for the most accurate code choice.
Visit (Seventh Character)
In select chapters, a “seventh character” is necessary for correct coding. Specifically for urology, this seventh character is used in the S and T chapters, which include trauma and complications. From a documentation standpoint, these conditions require documentation of whether this is the initial visit for the condition/trauma, a subsequent visit, or a visit to help manage the sequelae of the condition. For those who are submitting the codes, a seventh character is used, wherein the character “A” represents the correct seventh character for the initial visit, “D” for a subsequent visit, and “S” indicates a visit for the sequelae of the condition. This letter must always be in the seventh position; a placeholder “X” (or multiple placeholder “X”s) may be used between the code and the seventh character to ensure that the letter is always in the seventh position. For example, puncture wound of the penis with foreign body will be found at S31.24; it is the initial encounter for this condition, the correct code will be S31.24XA, with the “A” in the seventh position and an “X” as a placeholder at the sixth position. A subsequent visit for this condition will be correctly coded as S31.24XD.
Cost
There will be a significant cost associated with the transition. Fixed costs include the necessary upgrades to hardware and software, both for electronic medical records and for practice management. This may require hiring further staff. There will be a significant increased time for documentation due to increased specificity and proper code choice. The most significant cost to practices may be the decreased revenue stream in the first few months after ICD-10 implementation at the level of the payor—urologists and urology groups only need to learn the urology-specific codes, a payor will need to learn the entire ICD-10 code set. There may be a significant delay while a payor asks for documentation and charts to ensure proper codes are chosen. Many practices are considering taking out loans or increasing their lines of credit to handle the possible financial hardship involved.
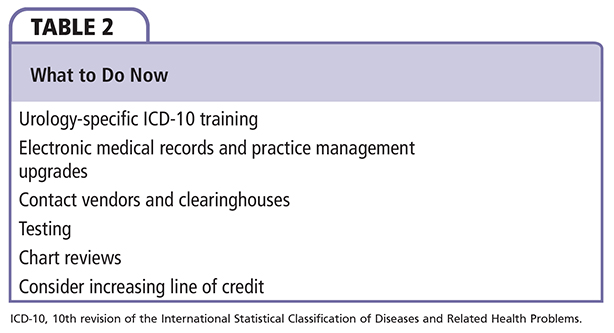
Table 2 contains a list of action items that should be accomplished as soon as possible. It is imperative to start ICD-10 training as soon as possible. Those with the attitude that “ICD-10 is just an expansion of ICD-9” or those who are not concerned because they have electronic medical records or professional coders are those who will feel the financial impact the most. Although the codes sets overall do not appear too challenging to learn, understanding the rules and specificity does take time; there are many nuances that are only learned through practice. I do not believe that a “generic” or “general” ICD-10 course serves anyone in the urology field; rather, urology-specific training will teach the codes and the documentation requirements while providers and practices are learning the rules of ICD-10. The American Urological Association has a basic training course available for purchase on its Web site. Providers must improve their dictations and documentation, whether they are the ones who are choosing the codes (such as from their electronic records) or if they have a coder/biller. There is no way a coder or biller can choose the correct code without proper documentation. Testing should be done as soon as the electronic medical record system, practice management, clearinghouses, and payors are ready. Chart reviews for proper documentation, code choice, and further education is vital prior to the October 1, 2015 implementation. A determination of the potential financial impact on the company (decreased productivity, fewer patients seen, increased time of documentation, and delay in payments) should be undertaken, as should a determination of whether an increased line of credit will be needed to cover expenses during the transition. ![]()