Metastatic Urethral Melanoma: Case Report and Review of the Literature
Rogério Saint-Clair Pimentel Mafra, MD, MSc, PhD,1 Luiz Ronaldo Alberti, MD, MSc, PhD,2 Bruno Moraes Vasconcelos,1 Rafaela Saint-Clair Pimentel Mafra De Oliveira, MD3
1Instituto Metropolitano de Ensino Superior-IMES, Ipatinga, MG, Brazil; 2Department of Surgery, Faculty of Medicine, UFMG, Belo Horizonte, MG, Brazil; 3Belo Horizonte Health System, Belo Horizonte, MG, Brazil
Melanoma is a cancer that originates from melanocytes, is predominant in adults with white skin, represents 4% of skin cancers, and has high possibility of forming metastasis. This review reports on the case of a young man, age 36 years, previously diagnosed with melanoma. The patient complained of obstructive urinary symptoms and, while he was undergoing a cystoscopy, it was discovered that he had a lesion corresponding with metastatic melanoma of the prostatic urethra, which occluded almost the entire urethra and resulted in blocked urinary flow. He underwent a transurethral resection of the prostate, followed by resection of the lesion. After the procedure, he had good urinary flow and is currently on follow-up.
[Rev Urol. 2014;16(1):47-49 doi: 10.3909/riu0584]
© 2014 MedReviews®, LLC
Key words
Melanoma • Urethra • Urinary obstruction • Metastasis • Urethral melanoma
Melanoma can appear on normal skin or on a pigmented lesion. In the case of a preexisting pigmented lesion, there may be an increase in size, and change in color and shape that begins to show irregular edges. The color may vary from light brown to various shades to reach the black color that is typical of melanoma, or it may display on a nonpigmented area.
With regard to treatment, only stage I through stage III disease is potentially curable by aggressive surgery (total or partial penectomy with lymphadenectomy without nodal commitment) with microscopic surgical margins of > 2 cm free from the infirmity; partial urethrectomy is associated with a risk of local recurrence of 50% to 70% within the first year.
Main Points
•A working knowledge of the varied presentations associated with primary urethral melanoma as well as its histopathologic features is an important component to early diagnosis and effective treatment. Many adverse prognostic factors exist such as age > 60 years, thickness > 3.5 mm, ulceration, and diameter > 15 mm.
•Due to its atypical location, melanoma of the urethra has a delayed diagnosis, and therefore, delayed treatment initiation. Due to its poor prognosis and the aggressiveness of the tumor, diagnosis should be made as early as possible due to the risk of impaired renal function.
•The cystoscopy is an indispensable method for diagnosis in the case of young patients who present with urinary symptoms not typical for that age range, with a severe pathology and high degree of metastasis. In our case, it was essential for the diagnosis and treatment planning.
•The presence or absence of lymph node metastasis is the most significant prognostic factor for survival, as survival rates are approximately halved by the presence of nodal metastasis.
•Surgical resection is the preferred treatment. Radiotherapy and chemotherapy may also be used depending on the stage of the neoplasm. Once it has metastasized, melanoma is incurable in most cases. The treatment strategy for advanced disease should then aim to relieve symptoms and improve a patient’s quality of life.
Primary malignant melanoma of the urethra is rare, representing < 1% of all melanomas1,2; it is often misdiagnosed, which leads to delays in treatment.2 The lethality is high, but its incidence is low. Prognosis is considered good if it is detected in its early stages.1 In recent years, there have been great improvements in patient survival rates. In developed countries, the average estimated 5-year survival is 73%, whereas in developing countries, the average survival is 56%. The estimated world average is 69%.1 Risk factors in order of importance are sensitivity to the sun, light skin, excessive sun exposure, history of skin cancer, family history of melanoma, congenital nevi, maturity, xeroderma pigmentosum, and dysplastic nevi.1
Individual management according to the clinical presentation is based on extrapolation of evidence for other melanoma treatments.2 Due to low occurrence rates of urethral melanoma, the optimal therapy has not yet been established, and surgery remains the mainstay of primary therapy; adjuvant locoregional and systemic therapies are needed.2 This article reports on the case of a young patient with metastatic melanoma in the urethra which led to urinary obstruction and urinary symptoms.
Case Report
A 36-year-old man with a previous diagnosis of cutaneous melanoma presented with metastases in various parts of his body. The patient progressed with hematuria and obstructive urinary symptoms, with a slow and gradual onset, followed by dysuria, alguria, and pollakiurie, as well as elevated kidney waste. There was no need for dialysis and no episodes of anuria, oliguria, or urethral bleeding. The patient did not have vitiligo or melanuria.
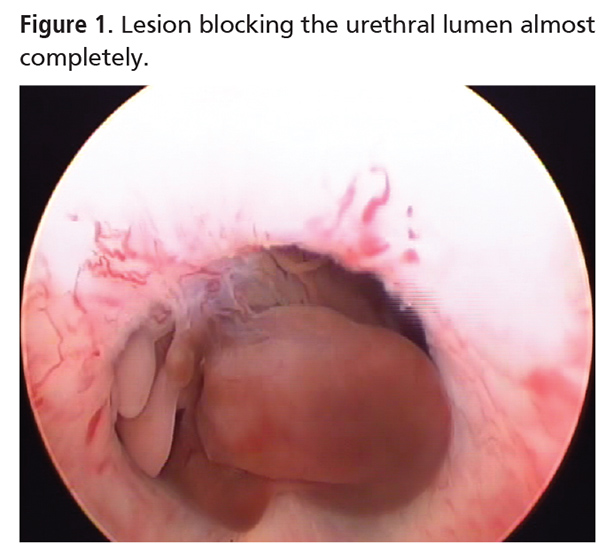
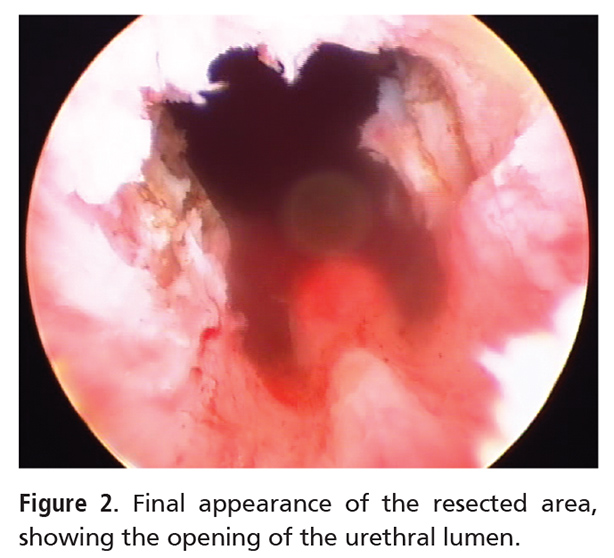
The patient initially submitted to a cystoscopy that resulted in the discovery of a brown-colored lesion on the prostatic urethra (Figure 1) located above the vero montanum. The lesion almost completely obstructed the urethral lumen, forming an obstruction to the valve mechanism that blocked the exit of the normal urinary flow, and resulted in the onset of the patient’s symptoms. During cystoscopy, it was observed that the bladder had trabeculations compatible with hypertrophic bladder, and showed chronicity of the pathology. The patient underwent a transurethral resection (TUR), in which the lesion and the wound bed were excised. The resection was uneventful, and the urethral catheter remained for 24 hours. After catheter removal, the patient experienced good urination, with a preserved urinary stream and relief of previous symptoms (Figure 2).
On histopathologic examination, it was confirmed as a poorly differentiated metastatic melanoma that showed nuclear atypia with few mitoses, a brownish pigment, and associated areas of transitional mucosa. Currently, the patient continues to be free of previous urinary symptoms, and is being monitored at our institution.
Discussion
Melanoma can appear on normal skin or on a pigmented lesion. In the case of a preexisting pigmented lesion, there may be an increase in size, and change in color and shape that begins to show irregular edges.1 The color may vary from light brown to various shades to reach the black color that is typical of melanoma, or it may display on a nonpigmented area.1 A working knowledge of the varied presentations associated with primary urethral melanoma as well as its histopathologic features is an important component to early diagnosis and effective treatment. Many adverse prognostic factors exist, such as age > 60 years, thickness > 3.5 mm, ulceration, and diameter > 15 mm.2 However, the presence or absence of lymph node metastasis is the most significant prognostic factor for survival, as survival rates are approximately halved by the presence of nodal metastasis.2 The lesion we found through cystoscopy was exophytic, irregular, and light brown (Figure 1). The growth or change of its form is progressive and occurs horizontally or vertically.1 The cystoscopy is an indispensable method for diagnosis in the case of young patients who present with urinary symptoms not typical for that age range, with a severe pathology and high degree of metastasis. In our case, it was essential for the diagnosis and treatment planning.
Surgical resection is the preferred treatment. Radiotherapy and chemotherapy may also be used depending on the stage of the neoplasm. Once it has metastasized, melanoma is incurable in most cases. The treatment strategy for advanced disease should then aim to relieve symptoms and improve a patient’s quality of life.1 Due to its atypical location,3,4 melanoma of the urethra has a delayed diagnosis,5,6 and, therefore, delayed treatment initiation.5 Due to its poor prognosis5-7 and the aggressiveness of the tumor, diagnosis should be made as early as possible6,8 due to the risk of impaired renal function. Approximately one third of patients have lymphatic involvement at diagnosis, with an overall 5-year survival of < 30%.3,9,10 With regard to treatment, only stage I through stage III disease is potentially curable by aggressive surgery (total or partial penectomy with lymphadenectomy without nodal commitment) with microscopic surgical margins of > 2 cm free from the infirmity; partial urethrectomy is associated with a risk of local recurrence of 50% to 70% within the first year.3 Thus, the goal of our patient’s treatment was palliative, as there was no chance for a cure.
Conclusions
Due to the seriousness of urethral melanoma, high probability of metastasis, and generally delayed diagnosis, palliative treatment with disobstruction of the urethra to re-establish urine flow is the treatment of choice. The goal is to improve symptoms along with the well-being of the patient because there is no curative treatment at such an advanced stage. Cystoscopy plays an important role in the evaluation of obstructive symptoms of the lower urinary tract, especially in atypical situations such as in a young man, as is presented here, as well as in malignancies with a high degree of metastasis. ![]()
References
- The Brazilian National Cancer Institute. http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/pele_melanoma. Accessed January 18, 2014.
- Comploj E, Palermo S, Trenti E, et al. Unexpected long survival in primary malignant melanoma of the male urethra. Case Rep Dermatol. 2009;20:93-99.
- Gutiérrez LC, Márquez-Rodas I, Lovelle AS, et al. [Melanoma of male urethra: a clinical case]. Actas Urol Esp. 2010;34:651-652.
- Antolín AR, López BM, Aparicio TF, et al. [Melanoma in urology: our experience and review of the literature]. Actas Urol Esp. 1991;15:361-365.
- Filipkowski LA, Barker MA, Karram MM. Primary genitourinary melanoma presenting as voiding dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1141-1143.
- Gassara M, Delongchamps NB, Legrand G, et al. Primary metastatic urethral melanoma: a case study [Article in French]. Prog Urol. 2010;20:80-82.
- Das P, Kumar N, Ahuja A, et al. Primary malignant melanoma at unusual sites: an institutional experience with review of literature. Melanoma Res. 2010;20:233-239.
- Sánchez-Ortiz R, Huang SF, Tamboli P, et al. Melanoma of the penis, scrotum and male urethra: a 40-year single institution experience. J Urol. 2005;173:1958-1965.
- Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol. 2007;56:823-834.
- Chang AE, Karnell LH, Menck HR, for The American College of Surgeons Commission on Cancer and the American Cancer Society. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. Cancer. 1998;83:1664-1678.