Bladder Leiomyoma Presenting With LUTS and Coexisting Bladder and Uterine Leiomyomata: A Review of Two Cases
Sudhir Kumar Jain, MS, FRCS (Edinburgh), FACS, FICS, Raman Tanwar, MS, FMAS, Aparajita Mitra, MS
Department of Surgery, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India
Mesenchymal tumors of the urinary bladder are a rare occurrence, the most common among them being leiomyoma of the bladder. These tumors commonly present with irritative urinary symptoms progressing gradually to obstructive symptoms as the size increases. We report on two patients who presented with lower urinary tract symptoms (LUTS). One of the patients also had concomitant bladder and uterine leiomyomata, which is the first such case to be reported in the literature. It is essential to differentiate leiomyoma from other common causes of LUTS. Cold cup biopsy has a significant false-negative rate and, in such cases, a wide local excision provides an optimal cure with excellent results.
[Rev Urol. 2014;16(1):50-54 doi: 10.3909/riu0586]
© 2014 MedReviews®, LLC
Key words
Bladder leiomyoma • Uterine fibroid • Lower urinary tract symptoms
Approximately 250 cases of bladder leiomyoma have been reported in the literature. The development of these tumors has been reported to be primarily intravesical (63%), labeled endovesical by Campbell and Gislason, although extravesical growth (30%) and intramural growth (7%) have also been reported.
Many theories exist on the etiology of this condition and the reason for its predominance in females. It has been suggested that chromosomal abnormalities, chronic inflammatory stimuli (Blum’s irritative theory), metaplastic reaction around the perivascular walls following inflammation of the bladder, dysontogenesis of embryonic rests (Piegel), or endocrine disorders (Lipschutz) may lead to the genesis of leiomyomas.
Main Points
•Benign tumors of the urinary bladder are rare and can present with a wide spectrum of complaints. Approximately 20% of women with bladder leiomyomas are asymptomatic; others’ complaints at presentation range from irritative symptoms, hematuria, and flank pain, to obstructive symptoms, such as acute urinary retention.
•Many imaging modalities have been used to diagnose leiomyomas. Even though both computed tomography and magnetic resonance imaging (MRI) offer excellent delineation of the tumor, it has been suggested that MRI should be the method of choice as it offers superior contrast and spatial resolution.
•For histologic diagnosis, tissue samples have been procured by a variety of means including cup biopsy forceps, a resectoscope, or an ultrasound-guided transvaginal biopsy.
•The management of leiomyomas depends on the dimensions and location of the tumor. A small tumor in an asymptomatic patient may be treated conservatively with regular follow-up. An increase in size or the onset of symptoms merits surgery. Transurethral resection is appropriate for small endovesical tumors, whereas larger tumors and those located intramurally or extravesically may require open/laparoscopic enucleation or partial cystectomy, based on the specific case.
•Prognosis for these benign tumors is excellent and no cases of malignant degeneration have yet to be reported.
Benign tumors of the urinary bladder are rare and can present with a wide spectrum of complaints ranging from irritative to obstructive urinary symptoms.1 Here we report on two patients who presented with lower urinary tract symptoms (LUTS), one of whom also had concomitant multiple uterine fibroids. To our knowledge, this is the first case to be reported in the literature.
Case Reports
Case 1
A premenopausal 42-year-old woman presented to the outpatient department with complaints of frequency, urgency, and occasional suprapubic discomfort unrelated to voiding that had occurred for the previous 6 months. She denied any history of hematuria, pyuria, graveluria, fever, or loin pain. No significant findings were detected on physical examination. Urine analysis showed pus cells without any other significant findings. Urine culture was sterile. Routine blood tests were within normal limits.
A plain radiograph of the kidney-ureter-bladder (KUB) showed no significant findings. Ultrasonography detected a 6 × 3-cm hypoechoic mass lesion in the left lateral wall of the bladder that did not move with postural changes. A contrast-enhanced computed tomography (CT) scan revealed a smooth, well-defined, 6 × 4-cm growth in the left posterolateral wall, with evidence of cystitis but no involvement of either ureteric orifice. The upper urinary tract was functionally and structurally normal. The CT findings were confirmed on cystoscopy which showed a smooth, sessile, spherical, submucosal growth. A deep biopsy obtained with a resectoscope showed a benign proliferation of smooth muscle in a connective tissue stroma suggestive of leiomyoma.
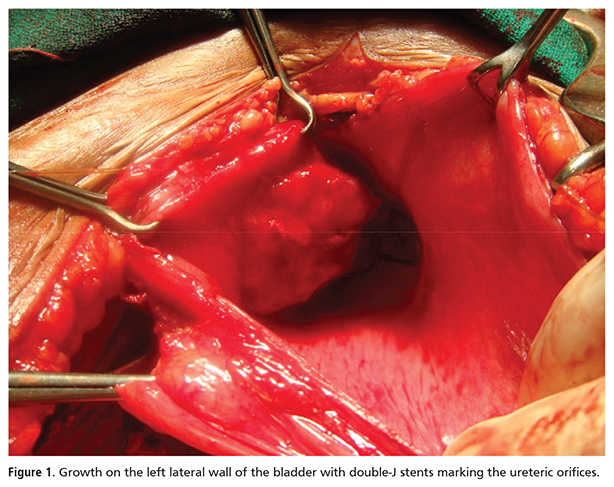
The patient underwent an open local excision of this well-encapsulated tumor (Figure 1) and postoperative histopathology showed a well-encapsulated leiomyoma with focal areas of degeneration without any evidence of malignant change. The postoperative period was uneventful and the urinary catheter was removed after 2 weeks. Over a 36-month follow-up period, no recurrence was detected on biannual cystoscopic examinations.
Case 2
The second case was a premenopausal 46-year-old woman who presented with LUTS along with two episodes of hematuria and intermittent pyuria for the previous 18 months. Physical examination yielded no positive findings. Urine analysis was suggestive of a urinary tract infection (UTI) with pus cells and 10 to 20 erythrocytes/high power field (HPF). No atypical cells were seen. Urine culture was sterile. Appropriate blood laboratory values were within normal limits.
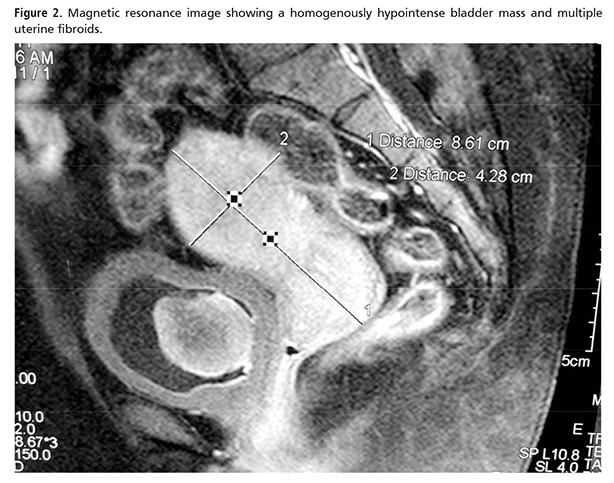
A plain radiograph KUB was normal. Ultrasonography revealed a 5 × 4-cm mass lesion in the bladder that was confirmed on contrast-enhanced CT to be an enhancing 3.5 × 3.4-cm soft tissue mass located in the posterior wall of the bladder. There was a thickening of the urinary bladder wall. Additional findings included multiple uterine fibroids. Magnetic resonance imaging (MRI) showed a submucosal homogenously hypointense lesion (T1- and T2-weighted images) with postgadolinium enhancement (Figure 2). There was no evidence of locoregional invasion. Cystoscopy revealed a smooth, rounded, sessile growth arising from the interureteric ridge distorting the medial margin of both ureteric orifices. Double J stents could be passed with ease bilaterally.
The biopsies taken with a transurethral resection (TUR) loop showed normal epithelium with a high nuclear:cytoplasmic ratio of the subepithelial elements. Excision biopsy was planned, in which a 4 × 3 × 2-cm grayish-white, encapsulated tumor (with a whorled appearance on sectioning) was removed (Figure 3). The diagnosis of leiomyoma was confirmed on histopathology. The postoperative period was uneventful. The patient was followed by regular cystoscopy at 6-month intervals for 30 months, with no evidence of recurrence.
The LUTS symptoms of both patients resolved within 3 weeks of surgery.
Discussion
Of all benign bladder tumors, 1% to 5% are suggested to be of mesenchymal origin1 with leiomyoma accounting for 0.43%.2 Goluboff and colleagues reviewed 37 cases of bladder leiomyoma and noted that the mean patient age was 44 years and that 76% of patients were women.3 Approximately 250 cases of bladder leiomyoma have been reported in the literature.4 The development of these tumors has been reported to be primarily intravesical (63%), labeled endovesical by Campbell and Gislason,1 although extravesical growth (30%) and intramural growth (7%) have also been reported.5
Approximately 20% of women with bladder leiomyomas are asymptomatic; complaints at presentation range from irritative symptoms (38%), hematuria (11%), and flank pain (13%), to obstructive symptoms (49%),3 including acute urinary retention.6 Neither of our patients had any positive findings on physical examination, although one series in the literature reported on a palpable pelvic lump in approximately 50% of patients on bimanual examination.3 The symptomatology of both patients was concordant with the observation that LUTS occurs more frequently in submucosal large tumors.7
Many imaging modalities have been used to diagnose this entity. Intravenous pyelogram shows a smooth filling defect in the bladder.8 Ultrasonography can detect a smooth-walled hypoechoic solid tumor, with varying degrees of internal echoes, covered by a thin hyperechoic line of mucosa.8 This submucosal location, akin to uterine leiomyomata, is characteristically unlike transitional cell carcinoma that arises from the mucosa. The patient may also have hydronephrosis due to increased intravesical pressure caused by bladder outlet obstruction or direct compression of the ureter orifice.9 Even though both CT and MRI offer excellent delineation of the tumor, Wong and colleagues opined that MRI should be the method of choice as it offers superior contrast and spatial resolution.10 Leiomyomas are known to show a variety of tumor-enhancement patterns after gadolinium injection but cystic degeneration always produces heterogeneous signal intensity on T2-weighted and postgadolinium T1-weighted images.11
For histologic diagnosis, tissue samples have been procured by a variety of means including cup biopsy forceps, a resectoscope, or an ultrasound-guided transvaginal biopsy.6 In our second case, biopsies were taken with cup biopsy forceps and TUR loop, respectively, and were inconclusive. Similar findings were observed by Silva-Ramos and colleagues, who reviewed 90 cases of bladder leiomyomata in literature, 28 of which were biopsied before the definitive treatment. Those obtained with a Tru-Cut® needle (Medline Industries, Inc, Mundelein, IL) and TUR were diagnostic, whereas results from 50% of the cold cup biopsy samples were false-negative.12
On histopathologic examination, a proliferation of spindle-shaped cells with eosinophilic cytoplasm and centrally located cigar-shaped nuclei within a fibrous stroma was suggestive of a leiomyoma. There was no evidence of mitotic figures. Focal areas of coagulative necrosis were noted in the first case. Leiomyoma may normally have up to two mitotic figures per HPF.13 Leiomyosarcoma, on the other hand, may also have few mitotic figures, but it is the myxoid degeneration and invasion of the muscularis propria that reliably distinguishes it from the benign counterpart. Immunohistochemistry analysis of benign leiomyoma shows a positive expression for smooth muscle actin and a negative expression for Ki-67.
The management of leiomyomas depends on the dimensions and location of the tumor. A small tumor in an asymptomatic patient may be treated conservatively with regular follow-up. An increase in size or the onset of symptoms merits surgery.3 TUR is appropriate for small endovesical tumors. Larger tumors and those located intramurally or extravesically may require open/laparoscopic enucleation or partial cystectomy,14 based on the specific case. Enucleation via a transvaginal approach is another option, especially for tumors close to the urethra, but this is subject to anatomic constraints and a higher risk of recurrence.13
Many theories exist on the etiology of this condition and the reason for its predominance in women.It has been suggested that chromosomal abnormalities,15 chronic inflammatory stimuli (Blum’s irritative theory), metaplastic reaction around the perivascular walls following inflammation of the bladder, dysontogenesis of embryonic rests (Piegel), or endocrine disorders (Lipschutz) may lead to the genesis of leiomyomas.3 The latter theory is supported by the observation of a higher incidence in women in the fertile period and the presence of steroidal ovarian receptors in the tumor.16 Estrogen has also been reported to increase the growth of leiomyomata of the bladder17 and its receptors have been identified in leiomyomatous tissues. In addition, estrogen and progesterone receptors are expressed in the bladder. These factors could also be a plausible explanation for the presence of concurrent multiple uterine leiomyomata in one of our patients, although Cornella and colleagues 15 attributed the sex-related disparity to the increased use of pelvic ultrasonography in women.
Prognosis for these benign tumors is excellent and no cases of malignant degeneration have yet to be reported.17
Conclusions
Leiomyoma must be differentiated from other common causes of LUTS. Confirmation of diagnosis may be difficult due to poor yield of cold cup biopsy. In our cases, open local excision provided optimal cure with excellent results. ![]()
References
- Campbell EW, Gislason GJ. Benign mesothelial -tumors of the urinary bladder: review of literature and a report of a case of leiomyoma. J Urol. 1953;70:733-741.
- Blasco Casares FJ, Sacristán Sanfelipe J, Ibarz Servio L, et al. Characteristics of bladder leiomyoma in our setting [in Spanish]. Arch Esp Urol. 1995;48:987-990.
- Goluboff ET, O’Toole K, Sawczuk IS. Leiomyoma of bladder: report of case and review of literature. Urology. 1994;43:238-241.
- Hernandez DJ, Chan DY. Bladder leiomyomata and pelvic pain. Urology. 2007;70:807-808.
- Maya MM, Slywotzky C. Urinary bladder leiomyoma: magnetic resonance imaging findings. Urol Radiol. 1992;14:197-199.
- Matsushima M, Asakura H, Sakamoto H, et al. Leiomyoma of the bladder presenting as acute urinary retention in a female patient: urodynamic analysis of lower urinary tract symptoms: a case report. BMC Urol. 2010;10:13.
- Greco A, Baima C, Piana P. Leiomyoma of the bladder: report of a case and review of the literature [in Italian]. Minerva Urol Nefrol. 1999;51:33-38.
- Yoon IJ, Kim KH, Lee BH. Leiomyomas of the urinary bladder: MR findings. AJR Am J Roentgenol. 1993;161:449-450.
- Lee CY, Wang LJ, Chuang KL, et al. Bladder leiomyoma with hydronephrosis. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:215-217.
- Wong FK, Wong YFM, Ma KF, Lui CY. Urinary bladder leiomyoma. J HK Coll Radiol. 2002;5:193-196.
- Chen M, Lipson SA, Hricak H. MR imaging evaluation of benign mesenchymal tumors of the urinary bladder. AJR Am J Roentgenol. 1998;168:399-403.
- Silva-Ramos M, Massó P, Versos R et al. [Leiomyoma of the bladder. Analysis of a collection of 90 cases]. [Article in Spanish] Actas Urol Esp. 2003;27:581-586.
- Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol. 1986;136:906-908.
- Jeschke K, Wakonig J, Winzely M, Henning K. Laparoscopic partial cystectomy for leiomyoma of the bladder wall. J Urol. 2002;165:2115.
- Cornella JL, Larson TR, Lee RA, et al. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol. 1997;176:1278-1285.
- Furuhashi M, Suganuma N. Recurrent bladder leiomyoma with ovarian steroid hormone receptors. J Urol. 2002;167:1399-1400.
- Kim IY, Sadeghi F, Slawin KM. Dyspareunia: an unusual presentation of leiomyoma of the bladder. Rev Urol. 2001;3:152-154.