Long-term Survival From Muscle-invasive Bladder Cancer With Initial Presentation of Symptomatic Cerebellar Lesion: The Role of Selective Surgical Extirpation of the Primary and Metastatic Lesion
Ganesh K. Kartha, MD,1 Joseph Sanfrancesco, MD,2 Esther Udoji, MD,3 Hemant Chaparala (MS4),4 Donna Hansel, MD, PhD,2 J. Stephen Jones, MD1
1Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH; 2Department of Pathology, Cleveland Clinic Foundation, Cleveland, OH; 3Imaging Institute, Cleveland Clinic Foundation, Cleveland, OH; 4Case Western Reserve University School of Medicine, Cleveland, OH
A 59-year-old man was diagnosed with urothelial carcinoma involving an isolated cerebellar metastasis after presenting to the emergency department for headache complaints. After selective surgical excision of the symptomatic brain lesion and delayed cystectomy due to intractable hematuria, he survived 11 years without evidence of recurrence or subsequent systemic chemotherapy. He eventually expired after delayed recurrence in the lung, supraclavicular lymph node, and brain. To our knowledge, this is the only case of prolonged survival from urothelial carcinoma after selective surgical extirpation of the primary and metastatic lesion without subsequent systemic chemotherapy.
[Rev Urol. 2015;17(2):106-109 doi: 10.3909/riu0643]
© 2015 MedReviews, LLC
Long-term Survival From Muscle-invasive Bladder Cancer With Initial Presentation of Symptomatic Cerebellar Lesion: The Role of Selective Surgical Extirpation of the Primary and Metastatic Lesion
Ganesh K. Kartha, MD,1 Joseph Sanfrancesco, MD,2 Esther Udoji, MD,3 Hemant Chaparala (MS4),4 Donna Hansel, MD, PhD,2 J. Stephen Jones, MD1
1Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH; 2Department of Pathology, Cleveland Clinic Foundation, Cleveland, OH; 3Imaging Institute, Cleveland Clinic Foundation, Cleveland, OH; 4Case Western Reserve University School of Medicine, Cleveland, OH
A 59-year-old man was diagnosed with urothelial carcinoma involving an isolated cerebellar metastasis after presenting to the emergency department for headache complaints. After selective surgical excision of the symptomatic brain lesion and delayed cystectomy due to intractable hematuria, he survived 11 years without evidence of recurrence or subsequent systemic chemotherapy. He eventually expired after delayed recurrence in the lung, supraclavicular lymph node, and brain. To our knowledge, this is the only case of prolonged survival from urothelial carcinoma after selective surgical extirpation of the primary and metastatic lesion without subsequent systemic chemotherapy.
[Rev Urol. 2015;17(2):106-109 doi: 10.3909/riu0643]
© 2015 MedReviews, LLC
Long-term Survival From Muscle-invasive Bladder Cancer With Initial Presentation of Symptomatic Cerebellar Lesion: The Role of Selective Surgical Extirpation of the Primary and Metastatic Lesion
Ganesh K. Kartha, MD,1 Joseph Sanfrancesco, MD,2 Esther Udoji, MD,3 Hemant Chaparala (MS4),4 Donna Hansel, MD, PhD,2 J. Stephen Jones, MD1
1Glickman Urological & Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH; 2Department of Pathology, Cleveland Clinic Foundation, Cleveland, OH; 3Imaging Institute, Cleveland Clinic Foundation, Cleveland, OH; 4Case Western Reserve University School of Medicine, Cleveland, OH
A 59-year-old man was diagnosed with urothelial carcinoma involving an isolated cerebellar metastasis after presenting to the emergency department for headache complaints. After selective surgical excision of the symptomatic brain lesion and delayed cystectomy due to intractable hematuria, he survived 11 years without evidence of recurrence or subsequent systemic chemotherapy. He eventually expired after delayed recurrence in the lung, supraclavicular lymph node, and brain. To our knowledge, this is the only case of prolonged survival from urothelial carcinoma after selective surgical extirpation of the primary and metastatic lesion without subsequent systemic chemotherapy.
[Rev Urol. 2015;17(2):106-109 doi: 10.3909/riu0643]
© 2015 MedReviews, LLC
Key words
Bladder cancer • Cystectomy • Metastasis • Urothelial carcinoma
Key words
Bladder cancer • Cystectomy • Metastasis • Urothelial carcinoma
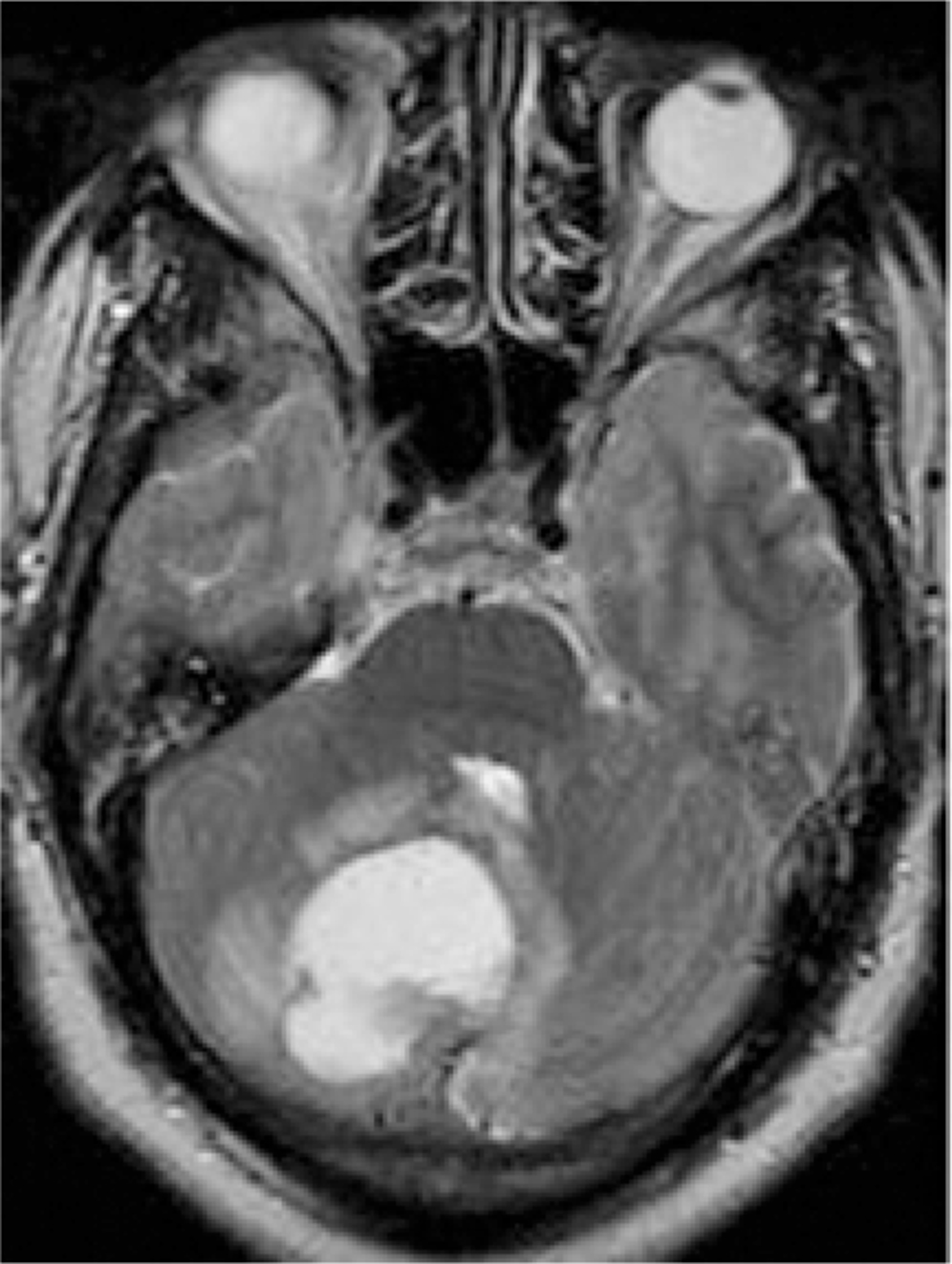
Figure1. Magnetic resonance image of the right cerebellar vermis mass consistent with neoplasm.
Surgical pathology of the brain lesion was consistent with metastatic non-small-cell carcinoma.

Figure2. Computed tomography image of the abdomen and pelvis showing a left-sided bladder mass (A) with associated left hydronephrosis (B).

Figure3. Final tissue pathology status postcystectomy showing urothelial carcinoma invasive to deep muscle of the bladder. Hematoxylin and eosin stain, original magnification, 10 ×.
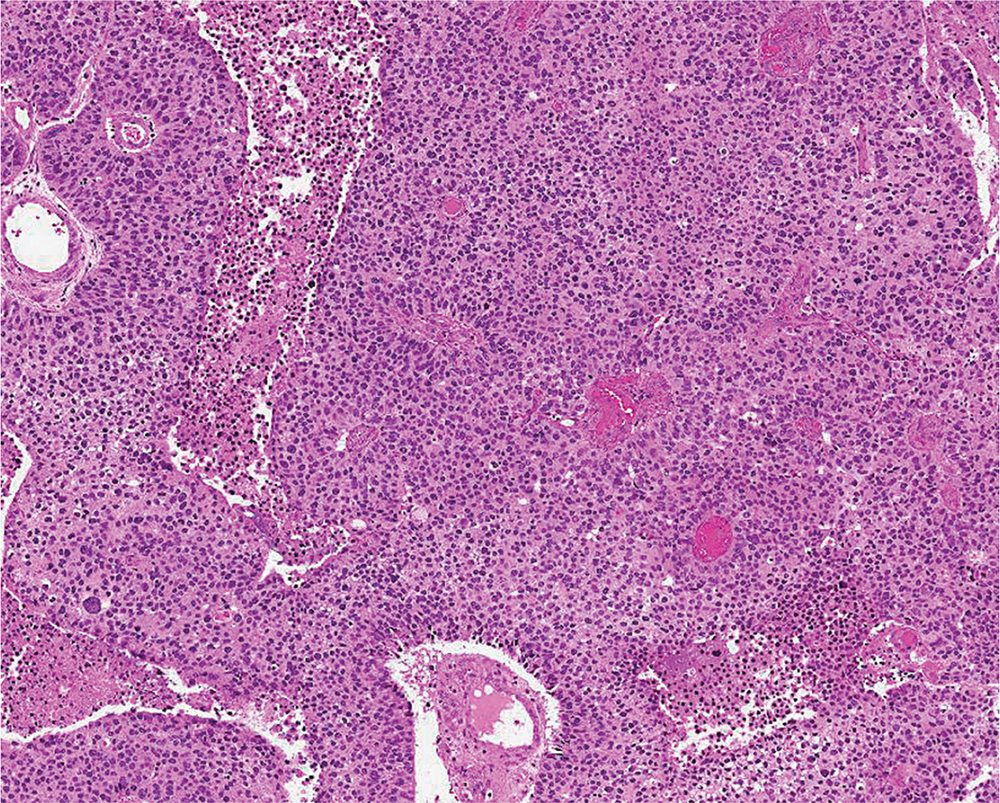
Figure4. Microscopic pathology of excised brain tumor consistent with infiltrative urothelial carcinoma and areas of necrosis. Hematoxylin and eosin stain, original magnification, 5 ×.
The uniqueness of this case resides in this patient's unlikely prolonged survival in the face of a disease status that historically leads to death within weeks to months.
Main Points
• Brain metastasis of bladder urothelial carcinoma is typically associated with widespread systemic disease and/ or multiple brain lesions. It is exceedingly rare to have bladder cancer metastasize to the brain without evidence of additional systemic manifestations.
• Some have proposed that an increase in the incidence of brain metastasis over the past three decades is due to the use of systemic chemotherapy for treatment of invasive bladder cancer.
• The uniqueness of this case resides in this patient's unlikely prolonged survival in the face of a disease status that historically leads to death within weeks to months. Despite bladder cancer metastasis to the brain, he remained under our surveillance with no evidence of disease recurrence for more than a decade.
Main Points
• Brain metastasis of bladder urothelial carcinoma is typically associated with widespread systemic disease and/ or multiple brain lesions. It is exceedingly rare to have bladder cancer metastasize to the brain without evidence of additional systemic manifestations.
• Some have proposed that an increase in the incidence of brain metastasis over the past three decades is due to the use of systemic chemotherapy for treatment of invasive bladder cancer.
• The uniqueness of this case resides in this patient's unlikely prolonged survival in the face of a disease status that historically leads to death within weeks to months. Despite bladder cancer metastasis to the brain, he remained under our surveillance with no evidence of disease recurrence for more than a decade.
Usually, brain metastasis of bladder urothelial carcinoma is associated with widespread systemic disease and/or multiple brain lesions. It is exceedingly rare to have bladder cancer metastasize to the brain without evidence of additional systemic manifestations.1 As with other forms of distant urothelial carcinoma metastasis, brain metastasis is associated with poor prognosis, with survival often less than 14 months in those with solitary brain lesions.2 We report an isolated bladder urothelial carcinoma metastasis to the cerebellum with an 11-year survival following extirpative therapy of both the primary lesion and brain metastasis.
Case Report
A 59-year-old man presented to the emergency department (ED) in 2002 with a 4-day history of worsening headache. Physical examination revealed no focal neurologic signs or symptoms. The ED workup included a computed tomography (CT) brain scan without contrast showing a 4 cm × 3 cm × 2 cm right cerebellar mass displaying prominent mass effect and mild obstructive hydrocephalus. Magnetic resonance imaging (MRI) showed a large right cerebellar vermis mass consistent with primary neoplasm or metastasis (Figure 1). He was admitted to the neurosurgery service and underwent suboccipital craniectomy with complete resection of the symptomatic right cerebellar brain tumor.
Surgical pathology of the brain lesion was consistent with metastatic non-small-cell carcinoma. The metastatic workup that followed included a negative CT chest scan result, and a CT abdomen and pelvis scan showing left hydroureteronephrosis secondary to an obstructing bladder mass (Figure 2). Urine cytology was positive for malignant cells of non-small-cell carcinoma. Urology consultation was obtained and transurethral resection was performed of a large left bladder wall tumor that was obstructing the left ureteral orifice. Surgical pathology of the bladder lesion revealed a grade III, poorly differentiated urothelial carcinoma invading the deep smooth muscle and consistent with the brain lesion.
The Hematology-Oncology department was consulted; chemotherapy was not recommended as the patient did not show any evidence of active systemic disease. He was discharged from the hospital with scheduled follow-up for whole brain radiation, which he underwent 6 weeks postoperatively Based on the presumption that cure was not possible, further treatment of the primary lesion was not entertained.
The patient underwent repeat cystoscopy with fulguration of the bladder tumor, but due to intractable postprocedure hematuria, definitive cystoprostatectomy with ileal conduit and complete pelvic lymphadenectomy was performed 7 months after his initial presentation. Surgical pathology revealed muscle-invasive urothelial carcinoma with metastatic spread to multiple pelvic lymph nodes (Figure 3). Secondary review of the surgical pathology of the excised brain lesion was consistent with metastatic urothelial carcinoma (Figure 4).
He continued to be followed by the Hematology-Oncology department, and systemic chemotherapy again was not recommended as he had no evidence of recurrent or measurable systemic disease. Repeat CT scans of the abdomen and pelvis over the years showed stable reactive retroperitoneal lymphadenopathy and no signs of metastasis. Results of repeat MRIs of the brain were negative for recurrence. Complications after cystectomy with ileal conduit formation included significant bilateral kidney stone burden requiring percutaneous nephrolithotomy.
In mid-2012, he showed evidence of a lung nodule and supraclavicular lymph node on a surveillance CT chest scan. Fine-needle aspiration of the supraclavicular node was consistent with metastatic urothelial carcinoma. He subsequently developed a recurrence of the brain metastasis in multiple cerebral locations. After a short course of palliative radiation to the chest, supraclavicular node, and brain, he ultimately expired in March 2013, 11 years after his diagnosis of bladder cancer with distant metastasis.
Discussion
Historically, brain metastasis of bladder urothelial carcinoma is exceedingly rare (<1%).1 Some have stated an increase in the incidence of brain metastasis over the past three decades due to the use of systemic chemotherapy for treatment of invasive bladder cancer. One theory is that common chemotherapeutic regimens such as MVAC (methotrexate, vinblastine, doxorubicin, and cisplatin) for bladder cancer do not effectively penetrate the blood brain barrier.3
Furthermore, it is exceedingly rare for patients with bladder cancer to initially present with neurologic complaints from brain metastasis, and it has only once been reported in a patient with isolated brain metastasis with no other systemic disease. In our review, we were only able to find four cases in which the primary presentation for metastatic bladder cancer were signs and symptoms related to brain lesions. Three of those four patients were found to have widespread systemic disease and/or multiple brain lesions on metastatic workup.4,5 Only one case was found of an isolated brain lesion and no evidence of disease outside the brain and bladder.6 Of note, one other case was found of neurologic complaints related to an isolated cerebellar lesion, but the patient had a previous history of localized bladder cancer and received intravesical thiotepa.7 Unlike our patient, neither of these patients with isolated brain lesions underwent cystectomy at any point after the diagnosis of metastatic disease. Interestingly, the two identified cases with isolated brain lesions and no other systemic metastasis consisted of isolated cerebellar metastasis, which is similar to the brain lesion found in our patient. There is no evidence that urothelial carcinoma has a propensity for cerebellar development.
The uniqueness of this case resides in this patient's unlikely prolonged survival in the face of a disease status that historically leads to death within weeks to months. Despite bladder cancer metastasis to the brain, he remained under our surveillance with no evidence of disease recurrence for more than a decade. In a series from the Cleveland Clinic (Cleveland, OH) prior to this patient's treatment, 16 patients with bladder cancer and metastasis to the brain between 1982 and 1999 were retrospectively reviewed; 11 patients were treated with whole-brain radiation only, with a median survival of 2 months (range, 2-11 mo). Two patients underwent cystectomy followed by radiation (similar to our patient's treatment) with survival of 12.75 months and 2.75 months, respectively.8 Rosenstein and colleagues2 reported a 14-month median survival at Memorial Sloan Kettering Cancer Center (New York, NY) in their bladder cancer population with solitary brain metastatic lesions.2 To our knowledge, this is the only case report of a patient with prolonged survival after treatment of metastatic bladder cancer to the brain. ![]()
References
- Whitmore WF Jr. Assessment and management of deeply invasive and metastatic lesions. Cancer Res. 1977;37(8 Pt 2):2756-2758.
- Rosenstein M, Wallner K, Scher H, Sternberg CN. Treatment of brain metastases from bladder cancer. J Urol. 1993;149:480-483.
- Dhote R, Beuzeboc P, Thiounn N, et al. High incidence of brain metastases in patients treated with an M-VAC regimen for advanced bladder cancer. Eur Urol. 1998;33:392-395.
- Quinn CM, Thomas H, Prentice MB. Urinary bladder carcinoma initially manifested as brain metastases. Postgrad Med J. 1992;68:689-690.
- Angulo JC, López JI, Unda-Urzaiz M, Flores N. Urinary bladder carcinoma initially manifested as brain metastases. Postgrad Med J. 1992;68:150-151.
- Davies BJ, Bastacky S, Chung SY. Large cerebellar lesion as original manifestation of transitional cell carcinoma of the bladder. Urology. 2003;62:749.
- Shamdas GJ, McLaren GD, Grimm T, Everson LK. Solitary cerebellar metastasis from transitional cell carcinoma of bladder. Urology. 1992;40:50-53.
- Mahmoud-Ahmed AS, Suh JH, Kupelian PA, et al. Brain metastases from bladder carcinoma: presentation, treatment and survival. J Urol. 2002;167:2419-2422.