Preparing for the Transition to ICD-10 by Chart Reviews of Four Urology Practice Types
Jonathan Rubenstein, MD
Chesapeake Urology Associates, Baltimore, MD
[Rev Urol. 2015;17(2):88-96 doi:10.3909/riu0680]
© 2015 MedReviews ®, LLC
Preparing for the Transition to ICD-10 by Chart Reviews of Four Urology Practice Types
Jonathan Rubenstein, MD
Chesapeake Urology Associates, Baltimore, MD
[Rev Urol. 2015;17(2):88-96 doi:10.3909/riu0680]
© 2015 MedReviews ®, LLC
Preparing for the Transition to ICD-10 by Chart Reviews of Four Urology Practice Types
Jonathan Rubenstein, MD
Chesapeake Urology Associates, Baltimore, MD
[Rev Urol. 2015;17(2):88-96 doi:10.3909/riu0680]
© 2015 MedReviews ®, LLC
On October 1, 2015, coding for medical encounters in the United States will change to the International Classification of Diseases and Related Health Problems, 10th revision (ICD-10) code set, replacing the ICD-9 code set. Compared with ICD-9, ICD-10 has a novel structure that is greatly expanded in its specificity. In addition, ICD-10 contains new code types and new billing rules that must be understood for proper coding. This change may create great challenges for providers and billing staff. Providers will need to provide documentation to support the specific code chosen, based on the codes that are available. To evaluate how an individual urologist may be affected by this transition, a review of charts was undertaken. From a random date, 20 consecutive office charts were reviewed from a general urologist, a male health/infertility subspecialist, a pelvic floor/reconstruction subspecialist, and a pediatric subspecialist. The results and an analysis of the review can be used to give a practicing urologist a sense of the transition to ICD-10, and to highlight some challenges that may be expected.
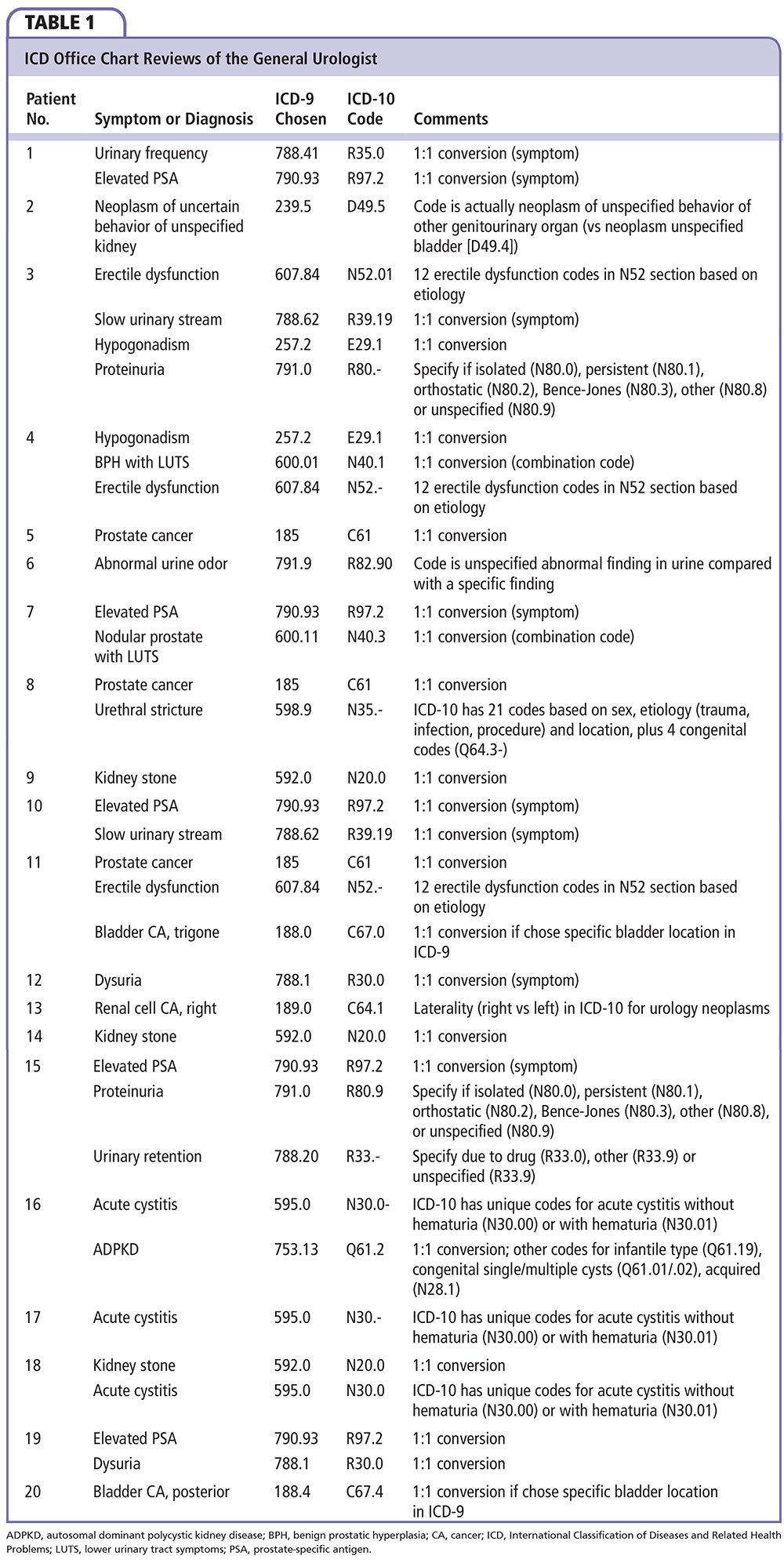
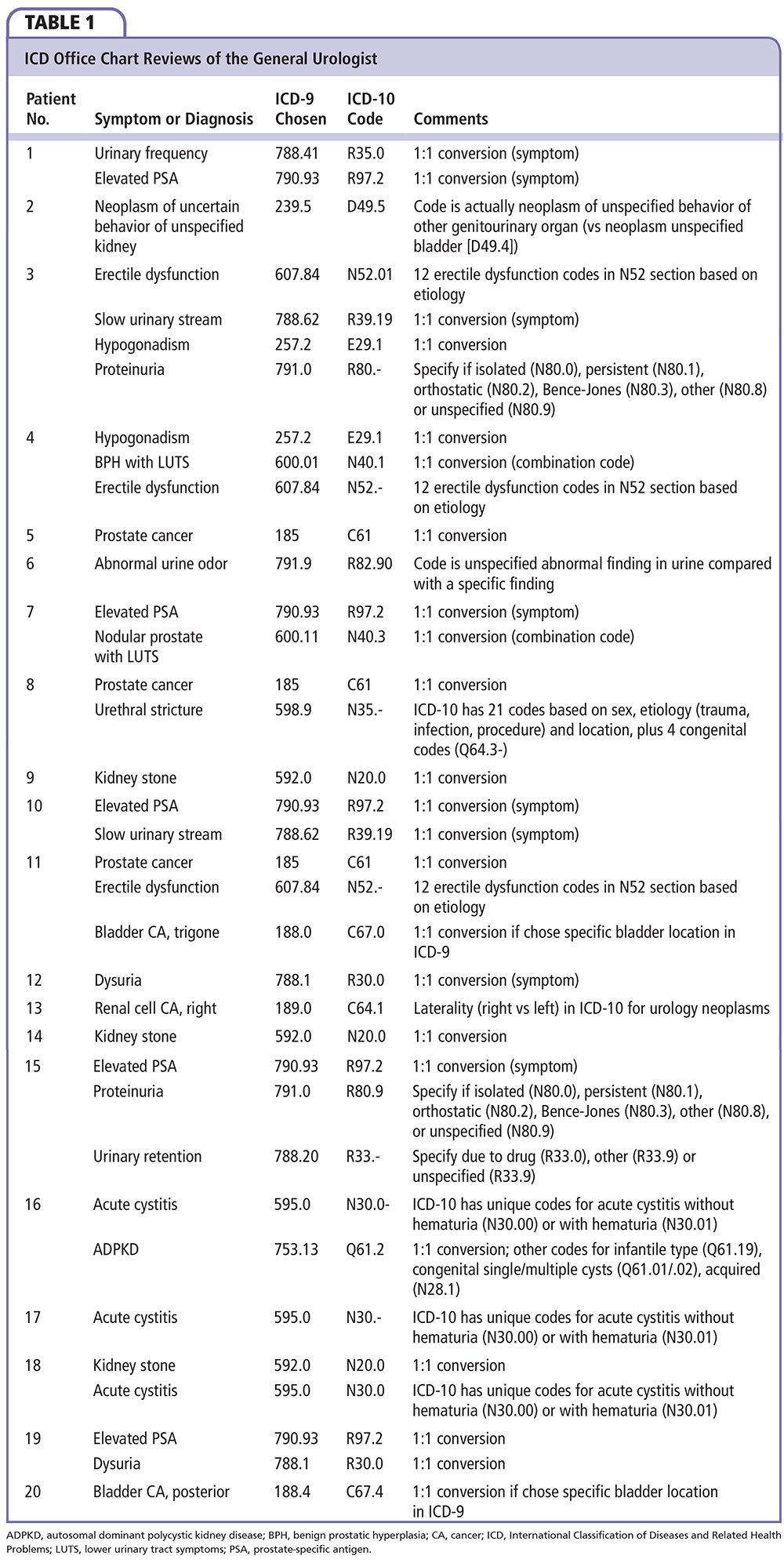
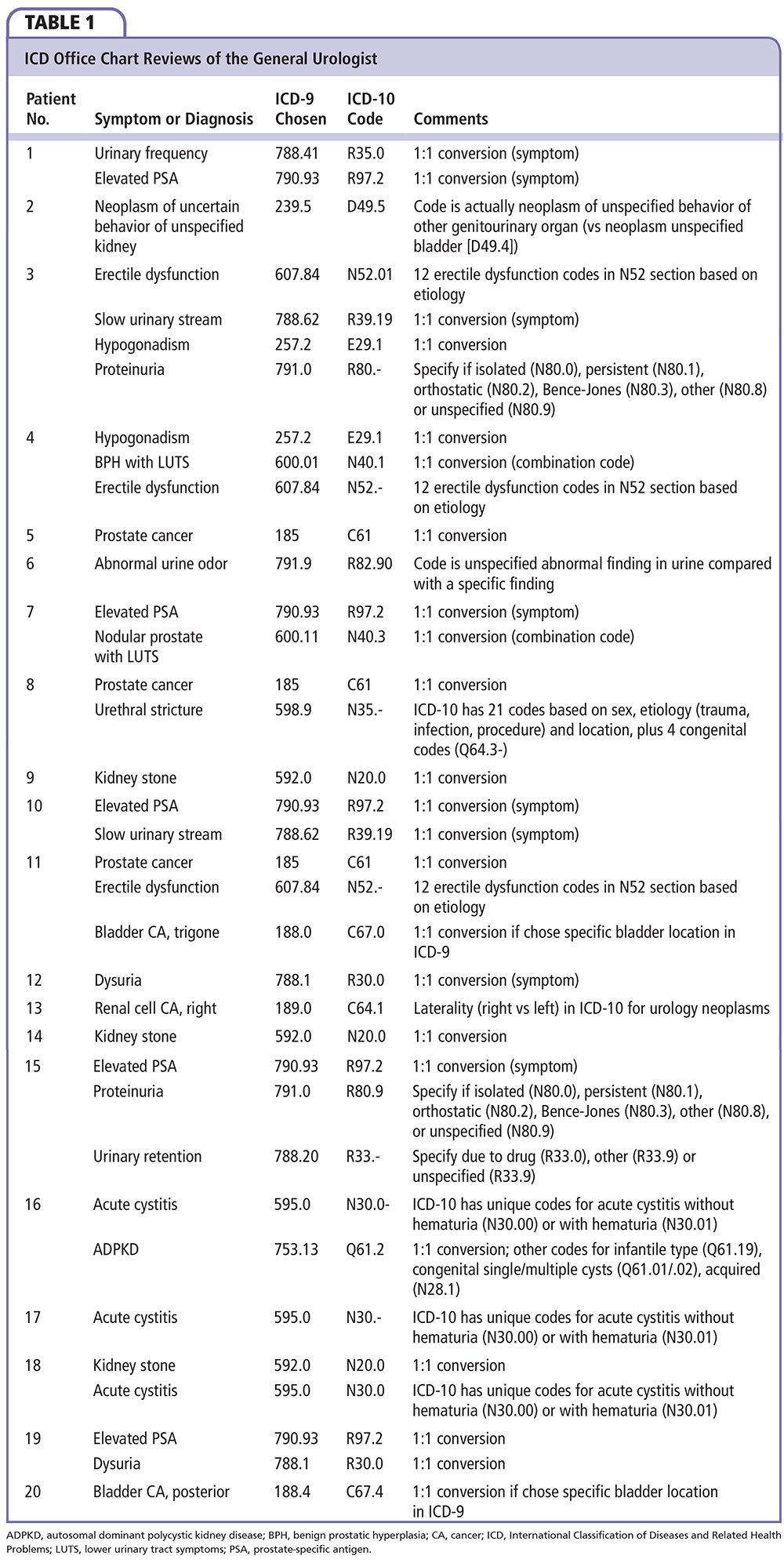
General Urologist
In the 20 patients reviewed, there were 36 total ICD-9 codes chosen (Table 1); 25 of the 36 ICD-9 codes (69.4%) have a 1:1 conversion to ICD-10 (if selected appropriately in ICD-9), whereas 11 codes (6 conditions) have more complexity, such as a 1-to-multiple transition, or require more information for accurate coding. The 1:1 conversion conditions included urinary symptoms (dysuria, slow urinary stream, and urinary frequency), elevated prostate-specific antigen level, kidney stone, prostate cancer, bladder cancer with location specified, autosomal dominant polycystic kidney disease, neoplasm of unspecified behavior of other genitourinary organ, abnormal urine, hypogonadism, benign prostatic hyperplasia with lower urinary tract symptoms, and nodular prostate with lower urinary tract symptoms. Please note that, although kidney stone has a 1:1 conversion from ICD-9 code 192.0 to ICD-10 code N20.0, there are also new codes for ureteral calculus (N20.1), calculus of the kidney and ureter (N20.2), and hydronephrosis due to renal and ureteral calculus (N13.2). Similarly, there are codes for other polycystic disease (infantile type has an ICD-10 code of Q61.19) and other congenital cyst codes.
The six conditions for which there is complexity in ICD-10 compared with ICD-9 in this group include erectile dysfunction, proteinuria, cystitis, kidney cancer, urinary retention, and urethral stricture. This means that the provider must have an understanding of approximately 44 additional codes, or at least know the basics with regard to the coding details needed for accurate documentation. In ICD-10, erectile dysfunction is expanded to 12 codes, based on the etiology of the condition (eg, due to arterial, venous occlusive, or combined arterial and venous disease; due to drug; due to 1 of 5 pelvic surgeries, each with its own code; or due to underlying disease, other, or unspecified), which does not even include the sexual dysfunction codes (5 ejaculatory dysfunction codes, along with other and unspecified) and the nonorganic code (found in the Mental, Behavioral, and Neurodevelopmental Disorders chapter). Proteinuria has six unique codes. In ICD-10, acute cystitis has two codes, as it is coded in combination as being with or without hematuria; there is no option for acute cystitis alone without this further detail. Malignant neoplasm of the kidney except renal pelvis contains unique codes for right and left side (laterality) along with a code for unspecified side. Urinary retention has three codes, based on whether it is due to drug, other, or unspecified. Urethral stricture has 25 code choices, based on whether it is congenital (4 codes), and based on sex, etiology, and location.
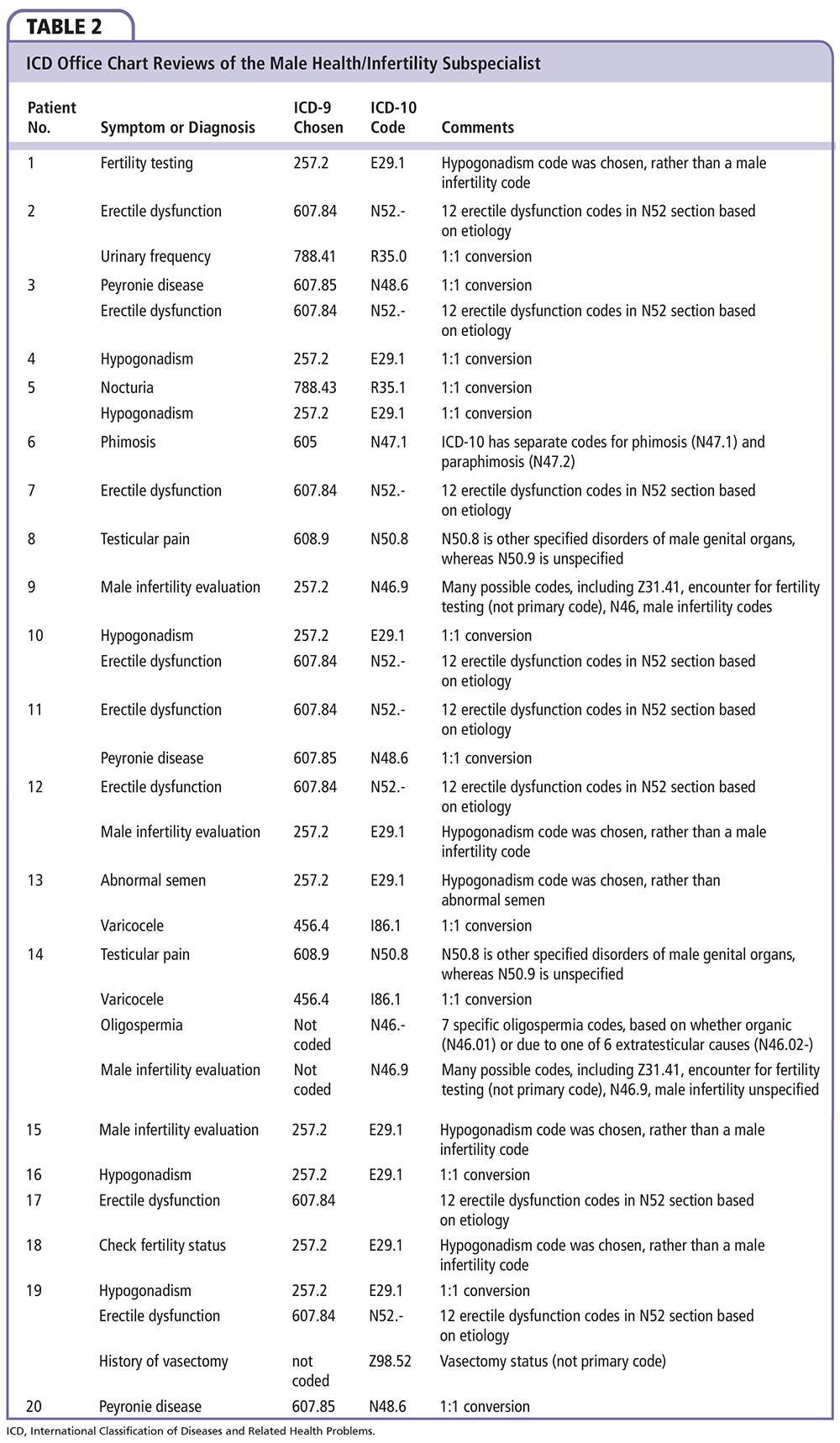
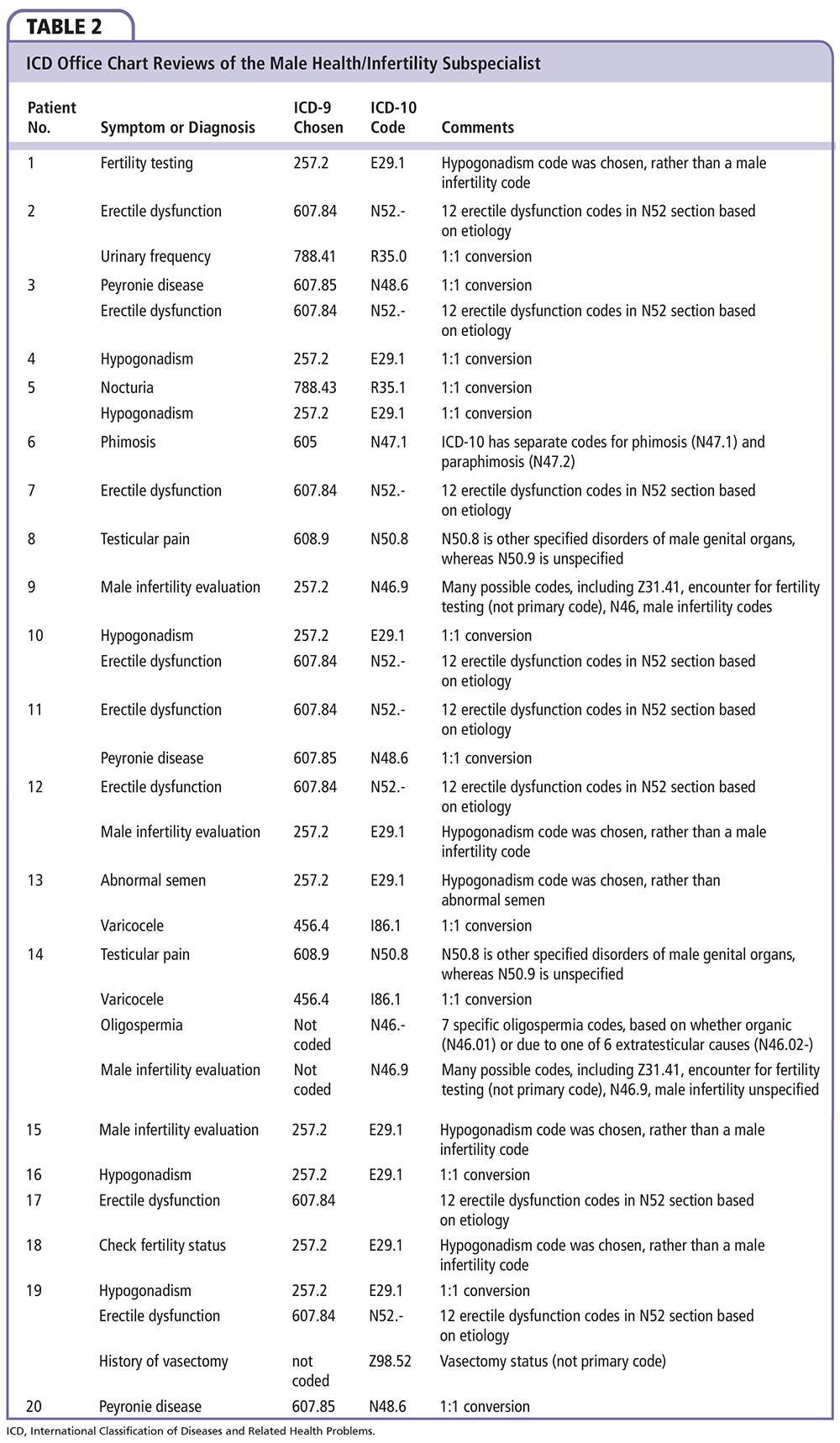
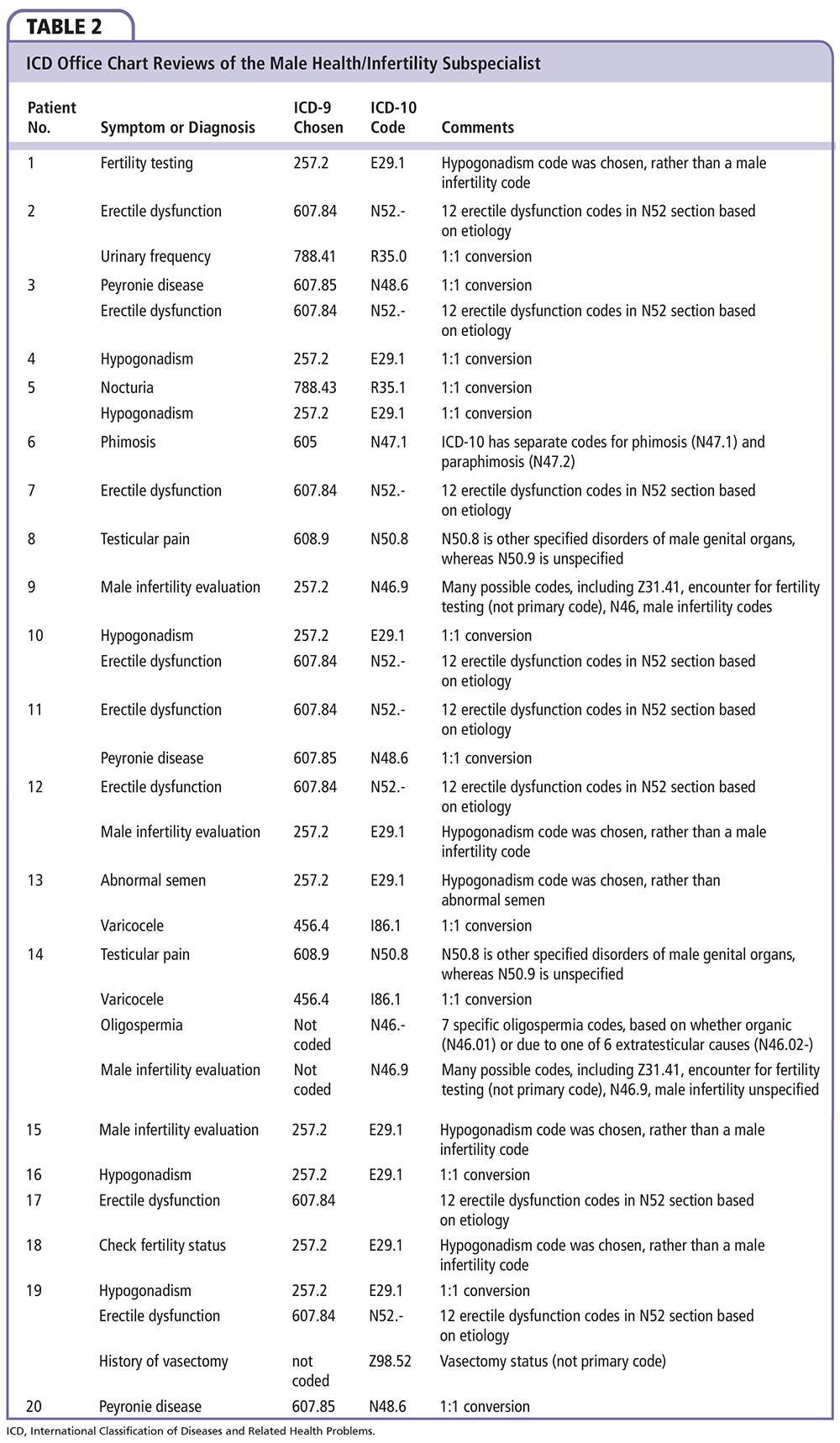
Male Health/Infertility Subspecialist
In the 20 patients reviewed, the male health/infertility subspecialist used 29 total ICD-9 codes, although from reading through the documentation details, it appears that at least three further diagnoses were discussed and treated, yet no ICD-9 code was chosen for billing purposes (Table 2); 12 of the 29 codes (7 conditions; 41.4%) had a 1:1 conversion from ICD-9 to ICD-10, whereas 17 codes (5 conditions) did not. The codes with a simple conversion include the urinary symptom codes (urinary frequency, nocturia), varicocele, Peyronie disease, and hypogonadism. Of the 11 patients for whom hypogonadism was chosen as a diagnosis, five had true hypogonadism (and therefore were included in the 1:1 conversion category), whereas six were being seen for male infertility issues and were therefore put into the complex category.
In ICD-9, code 605 encompassed a number of penile conditions, including phimosis, paraphimosis, redundant foreskin, or adherent prepuce. In ICD-10, each of these conditions has a unique code: N47.0 for adherent prepuce of newborn, N47.1 for phimosis, N47.2 for paraphimosis, N47.5 for adhesions of prepuce and glans, and N47.8 for other disorders of prepuce (including redundant foreskin). For patients who present for fertility testing or due to male infertility issues, there are a number of different available codes. In ICD-10, there are 16 male infertility codes in the N46 section (organic azoospermia and 6 extratesticular causes of azoospermia, organic oligospermia, and 6 extratesticular causes of oligospermia, other and unspecified male infertility), 10 codes for abnormal findings in semen (R86 section), checking vasectomy status (Z98.52, which cannot be used as a primary code), and encounter for fertility testing (Z31.41, which also cannot be used as a primary code). The ICD-9 code for erectile dysfunction was used eight times. The two patients who had testicular pain were given the ICD-9 code of 608.9, which is unspecified disorder of male genital organs; the patient with postvasectomy pain may be given the ICD-10 code N99.89 (other postprocedural complications of the genitourinary tract), and N29.1 (inflammatory disorder of the spermatic cord).
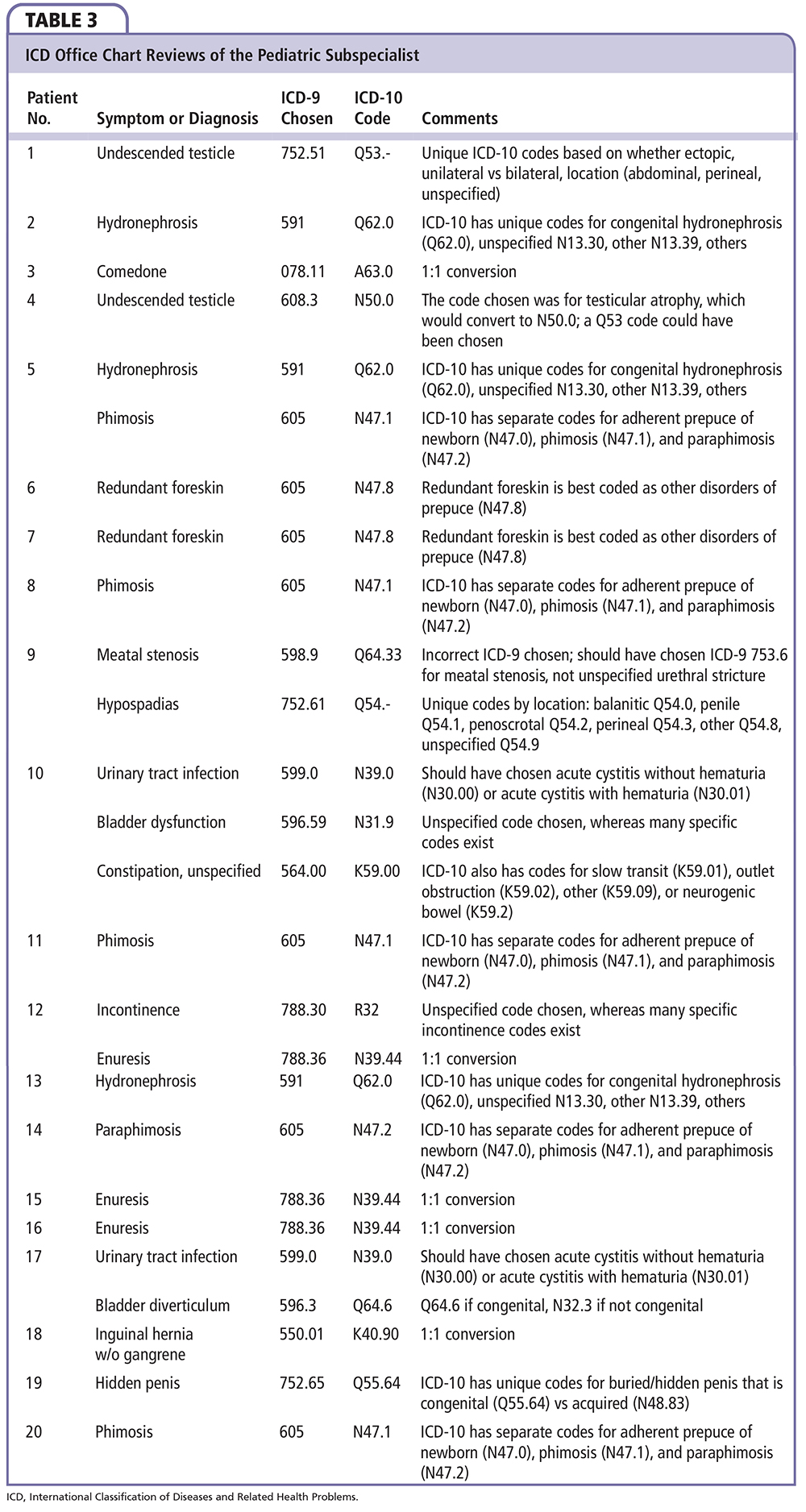
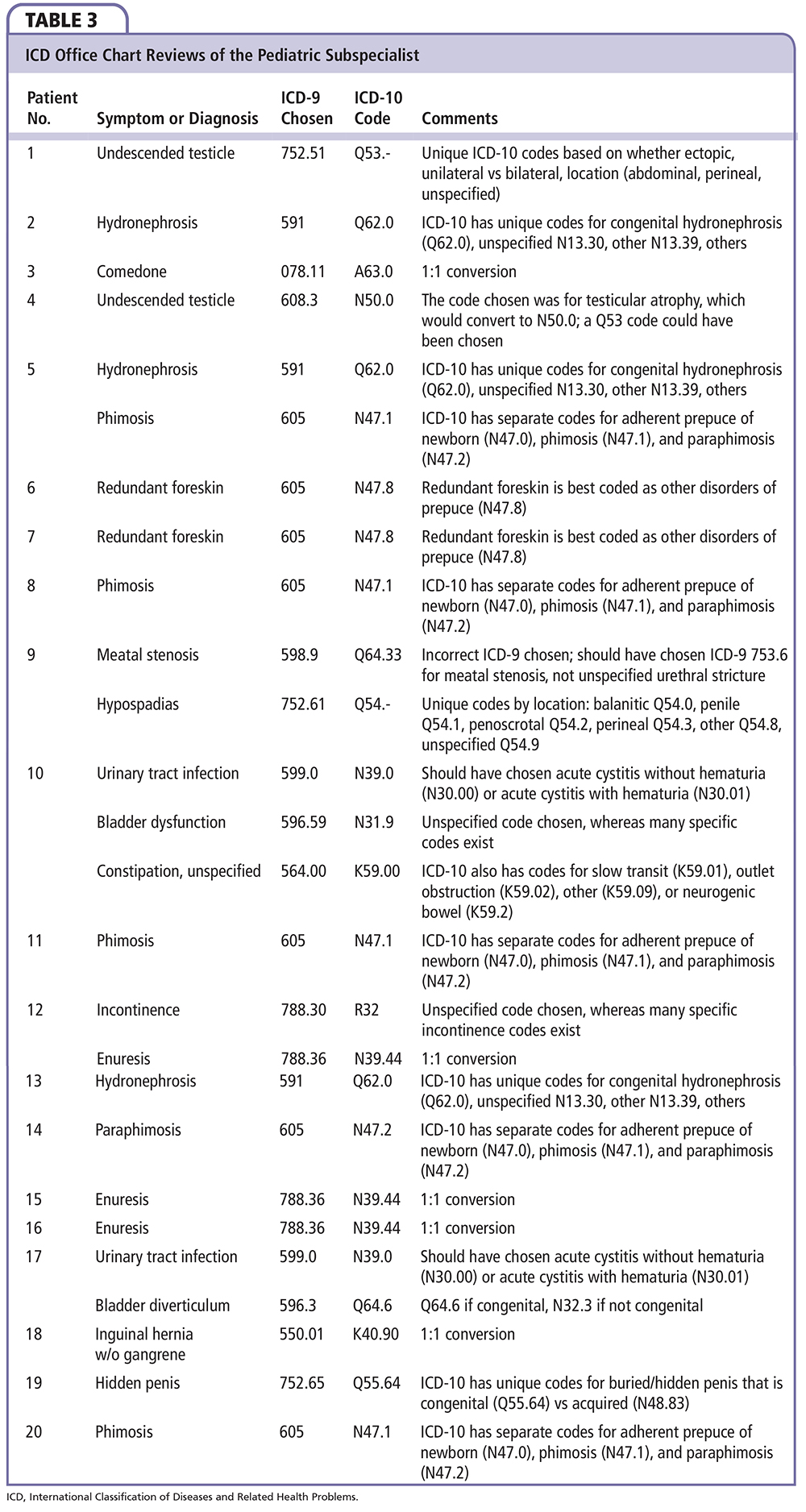
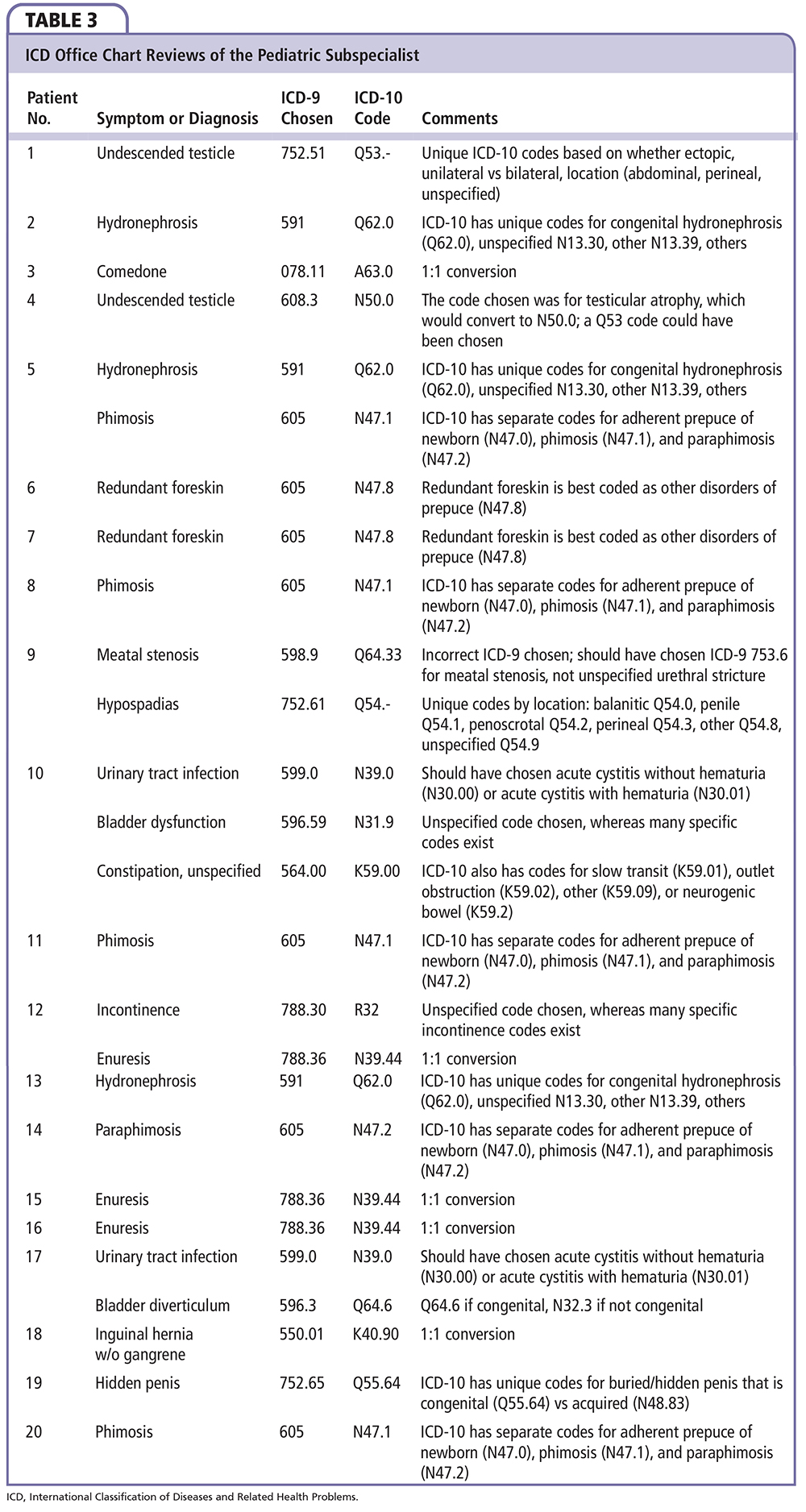
Pediatric Subspecialist
The pediatric subspecialist used 26 total ICD-9 codes in the 20 patients reviewed (Table 3). There was a simple 1:1 conversion for 5 of the 26 codes (3 conditions; 19.2%) with complexity in the remaining 21 codes (13 conditions). The simple 1:1 conversion codes included comedone, enuresis, and inguinal hernia without obstruction or gangrene. Conditions that may have more than one ICD-10 code choice in this group include the patients with phimosis, paraphimosis, redundant foreskin, meatal stenosis, unspecified urinary tract infection, constipation, bladder diverticulum, and buried penis. The ICD-9 code 599.0 is an unspecified urinary tract infection (ICD-10 N39.0); each of the patients seen had the more specific diagnosis of acute cystitis (ICD-9 595.0), which has two codes in ICD-10: acute cystitis without hematuria (N30.00), and acute cystitis with hematuria (N30.01). Constipation can be unspecified (which was chosen), or due to other, more specific conditions. Congenital bladder diverticulum has a single ICD-10 code (Q64.6) but needs to be differentiated from noncongenital diverticulum (N32.3). Congenital meatal stenosis has a single ICD-10 code; in this review, however, the ICD-9 code for urethral stricture unspecified (598.9) was chosen rather than the more specific congenital meatal stenosis code (ICD-9 753.6).
In ICD-10, there is a unique code for congenital hydronephrosis (Q62.0). It is important for documentation and coding purposes to differentiate congenital hydronephrosis from other types of hydronephrosis found in ICD-10, such as hydronephrosis due to ureteral stricture (N13.1), due to stone (N13.2), other (N13.39), and unspecified (N13.30). Undescended testicle has 10 unique codes, based on whether the condition is unilateral or bilateral, if it is ectopic, undescended abdominal, undescended perineal, or unspecified. Hypospadias has six codes based on location, other, or unspecified. In this review, ICD-9 code 596.59 was chosen for bladder dysfunction, which is an unspecified code. Other codes exist, including a variety of codes for neurogenic bladder (ICD-9 596.54), which have a number of more specific ICD-10 codes based on the bladder function (uninhibited, reflex, flaccid, other, and unspecified) and/or underlying cause (cord, cauda equina syndrome, or spinal cord injury). In one case, a code for testicular atrophy was chosen (ICD-9 608.3); this would have a 1:1 conversion to N50.0 if it had been the correct ICD-9 code based on the patient's presentation, but the patient was being evaluated for an undescended testicle.
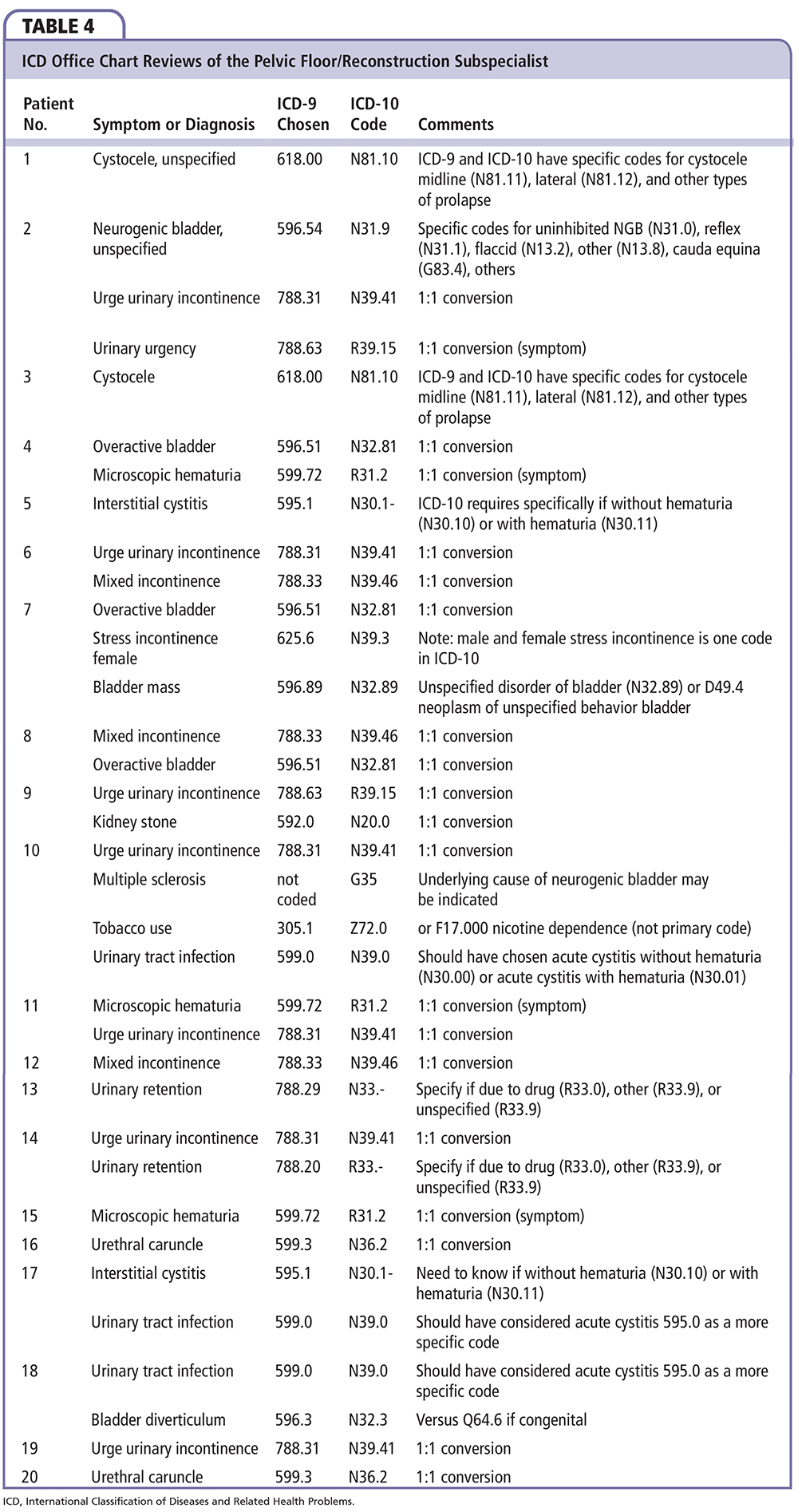
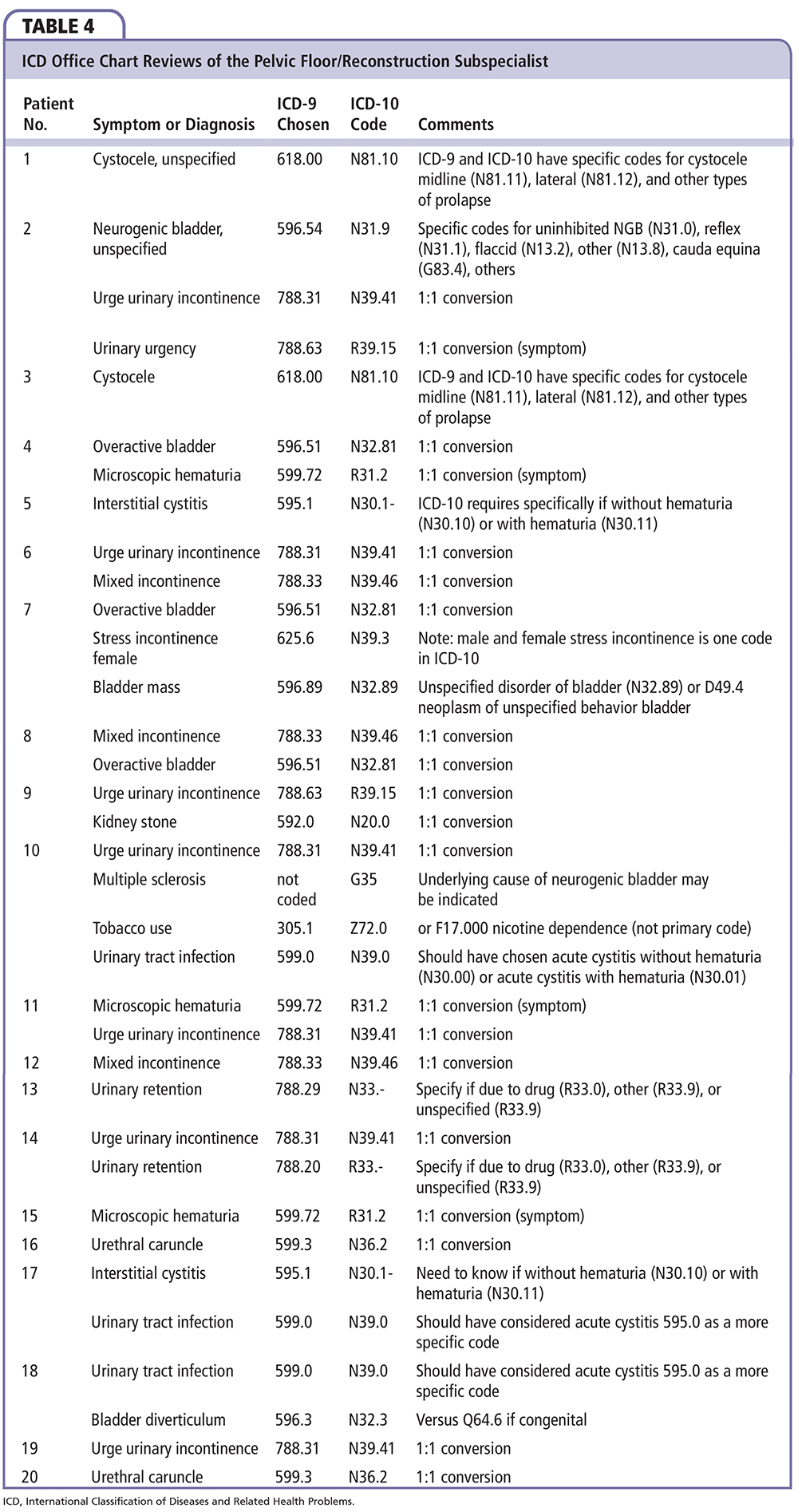
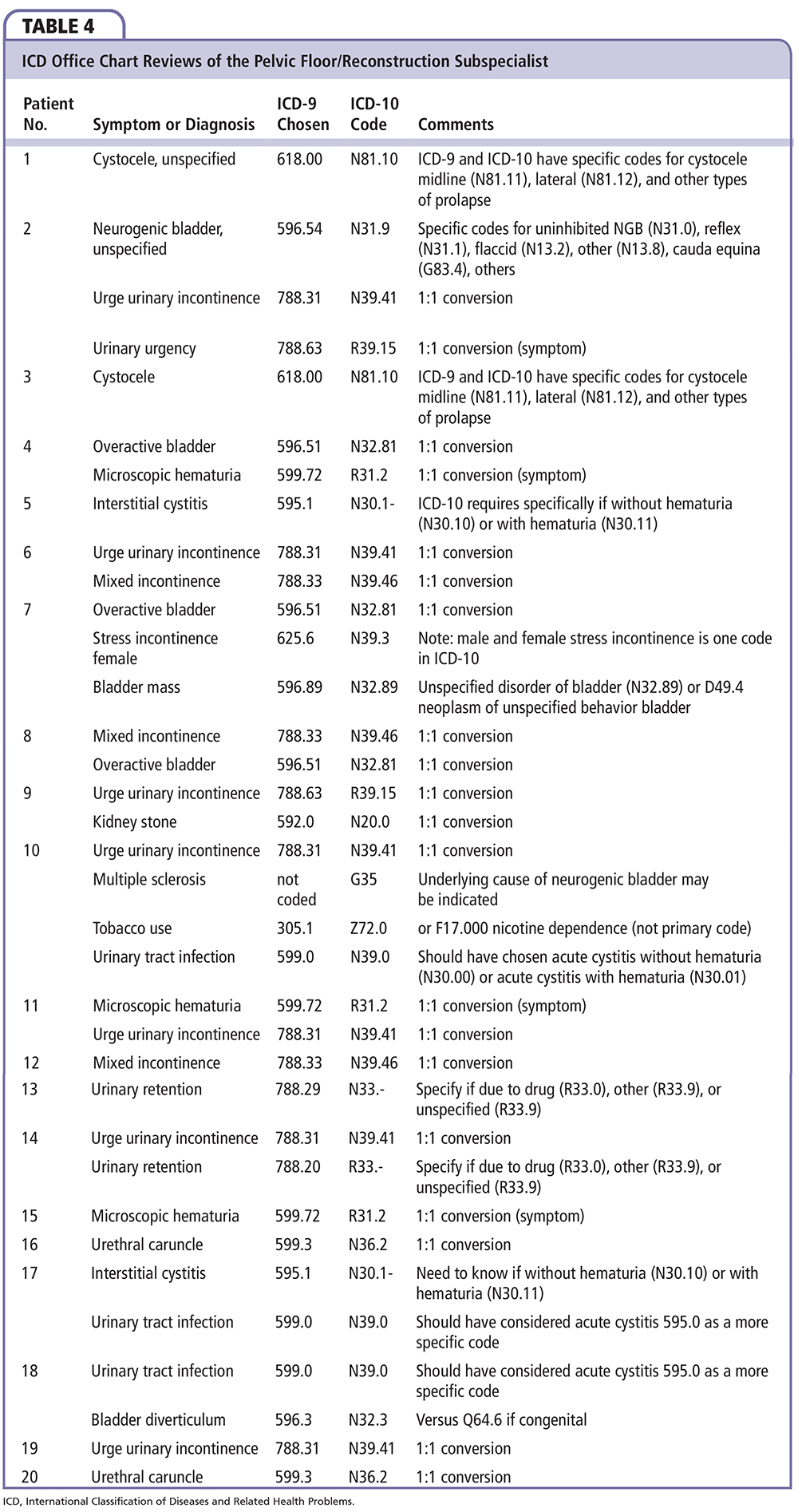
Pelvic Floor/ Reconstruction Subspecialist
In this review, 34 codes were selected for the 20 patients seen (Table 4); 21 of the 34 codes (8 conditions, 61.8%) have a 1:1 conversion from ICD-9 to ICD-10, including urinary symptoms (urge urinary incontinence, urinary urgency, overactive bladder, stress incontinence, mixed incontinence), microscopic hematuria, kidney stone, and urethral caruncle. This number could have been higher had more specific ICD-9 codes been chosen rather than unspecified codes. For example, cystocele has specific codes based on whether it is lateral or midline in both ICD-9 and ICD-10, in addition to other prolapse codes. In ICD-10, urinary retention has several codes, as does neurogenic bladder (based on etiology). Interstitial cystitis has unique ICD-10 codes based on whether it exists without hematuria (N30.10) or with hematuria (N30.11).
Discussion
It is important to recognize that ICD-10 is not merely a more specific and expanded code set from ICD-9, but rather is its own unique system. Along with increased specificity come new rules, new language, and a new structure. A number of codes do have a 1:1 conversion between the two code sets; some will have a 1-to-multiple conversion from ICD-9 to ICD-10, and others are completely different. Providers who are more comfortable with ICD-9 may find the transition to ICD-10 a bit easier. Those who currently use a high number of unspecified codes may encounter more challenges. A pediatric subspecialist may need to make more changes to his or her typical work day than someone whose practice uses a high number of urinary symptom codes. Providers will need to adjust their documentation to support the corresponding ICD-10 codes. This review highlights areas that individual providers may study based on their own practice patterns. ![]()