Challenges and Opportunities in Radiation-induced Hemorrhagic Cystitis
Bernadette M.M. Zwaans, MD,1 Heinz G. Nicolai, MD,2,3 Michael B. Chancellor, MD,1,4 Laura E. Lamb, MD1,2
1Department of Urology, William Beaumont Hospital, Royal Oak, MI; 2Departamento de Urología, Universidad de Chile, Santiago, Chile; 3Hospital Clínico San Borja Arriarán, Santiago, Chile; 4Oakland University William Beaumont School of Medicine, Royal Oak, MI
As diagnosis and treatment of cancer is improving, medical and social issues related to cancer survivorship are becoming more prevalent. Hemorrhagic cystitis (HC), a rare but serious disease that may affect patients after pelvic radiation or systemic chemotherapy, has significant unmet medical needs. Although no definitive treatment is currently available, various interventions are employed for HC. Effects of nonsurgical treatments for HC are of modest success and studies aiming to control radiation-induced bladder symptoms are lacking. In this review, we present current and advanced therapeutic strategies for HC to help cancer survivors deal with long-term urologic health issues.
[Rev Urol. 2016;18(2):57-65 doi: 10.3909/riu0700]
© 2016 MedReviews®, LLC
Challenges and Opportunities in Radiation-induced Hemorrhagic Cystitis
Bernadette M.M. Zwaans, MD,1 Heinz G. Nicolai, MD,2,3 Michael B. Chancellor, MD,1,4 Laura E. Lamb, MD1,2
1Department of Urology, William Beaumont Hospital, Royal Oak, MI; 2Departamento de Urología, Universidad de Chile, Santiago, Chile; 3Hospital Clínico San Borja Arriarán, Santiago, Chile; 4Oakland University William Beaumont School of Medicine, Royal Oak, MI
As diagnosis and treatment of cancer is improving, medical and social issues related to cancer survivorship are becoming more prevalent. Hemorrhagic cystitis (HC), a rare but serious disease that may affect patients after pelvic radiation or systemic chemotherapy, has significant unmet medical needs. Although no definitive treatment is currently available, various interventions are employed for HC. Effects of nonsurgical treatments for HC are of modest success and studies aiming to control radiation-induced bladder symptoms are lacking. In this review, we present current and advanced therapeutic strategies for HC to help cancer survivors deal with long-term urologic health issues.
[Rev Urol. 2016;18(2):57-65 doi: 10.3909/riu0700]
© 2016 MedReviews®, LLC
Challenges and Opportunities in Radiation-induced Hemorrhagic Cystitis
Bernadette M.M. Zwaans, MD,1 Heinz G. Nicolai, MD,2,3 Michael B. Chancellor, MD,1,4 Laura E. Lamb, MD1,2
1Department of Urology, William Beaumont Hospital, Royal Oak, MI; 2Departamento de Urología, Universidad de Chile, Santiago, Chile; 3Hospital Clínico San Borja Arriarán, Santiago, Chile; 4Oakland University William Beaumont School of Medicine, Royal Oak, MI
As diagnosis and treatment of cancer is improving, medical and social issues related to cancer survivorship are becoming more prevalent. Hemorrhagic cystitis (HC), a rare but serious disease that may affect patients after pelvic radiation or systemic chemotherapy, has significant unmet medical needs. Although no definitive treatment is currently available, various interventions are employed for HC. Effects of nonsurgical treatments for HC are of modest success and studies aiming to control radiation-induced bladder symptoms are lacking. In this review, we present current and advanced therapeutic strategies for HC to help cancer survivors deal with long-term urologic health issues.
[Rev Urol. 2016;18(2):57-65 doi: 10.3909/riu0700]
© 2016 MedReviews®, LLC
Key words
Hemorrhagic cystitis • Radiation-induced cystitis • Hematuria • Cancer survivorship
Key words
Hemorrhagic cystitis • Radiation-induced cystitis • Hematuria • Cancer survivorship
The effects of radiation-induced cystitis can occur as early as 6 months to as late as 20 years after radiation treatment.
Early symptoms of RC are thought to be due to damage to the bladder urothelium, which has a low cell turnover and thus is highly susceptible to irradiation-induced damage.

Figure 1. Developmental stages of RC. RC progression consists of three phases: a reversible acute inflammatory phase, a latent symptom-free phase, and a late chronic inflammatory phase. Each phase is characterized by specific pathologic changes that contribute to the symptoms associated with RC. D, detrusor; ECM, extracellular matrix; GAG, glycosaminoglycan; LP, lamina propria; RC, radiation cystitis; UE, uroepithelium. Reprinted with permission from Zwaans BM et al.9

Figure 1. Developmental stages of RC. RC progression consists of three phases: a reversible acute inflammatory phase, a latent symptom-free phase, and a late chronic inflammatory phase. Each phase is characterized by specific pathologic changes that contribute to the symptoms associated with RC. D, detrusor; ECM, extracellular matrix; GAG, glycosaminoglycan; LP, lamina propria; RC, radiation cystitis; UE, uroepithelium. Reprinted with permission from Zwaans BM et al.9
… the most important risk factors are radiation treatment related, including volume of tissue treated, total bladder dose and fractionation, mode of delivery (external beam and/or brachytherapy), concurrent treatments, and radiosensitivity of the affected bladder tissue.
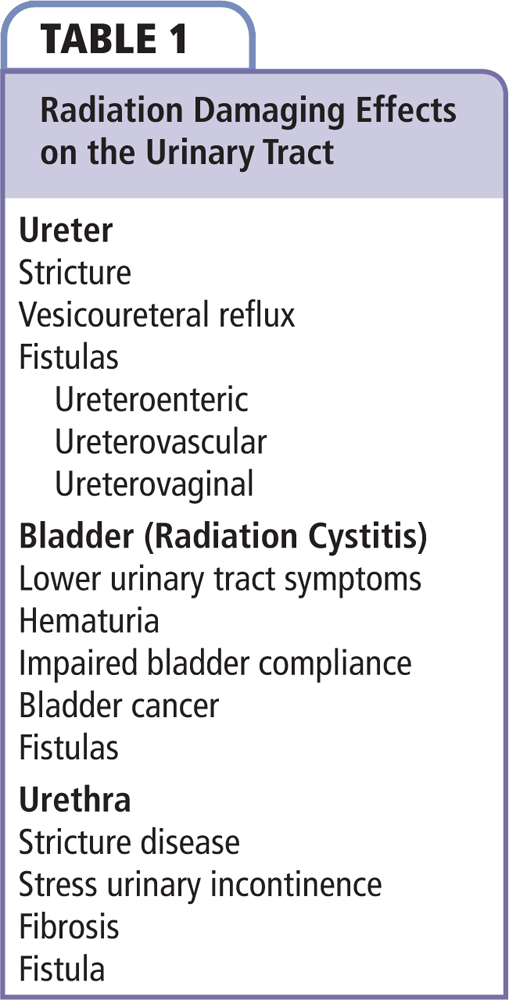

Figure 2. Treatment options for the management of HC. The preferred treatment option for HC is dependent on the severity of hematuria. The first step in the treatment of HC is directed toward clot evacuation and hydration to prevent further clot formation. If hematuria persists, continuous bladder irrigation, fulguration, HBOT and, in case of excessive blood loss, blood transfusion should be considered. Novel therapies such as BoNT injections and intravesical lipo-tacro could be implemented at this stage. If unresponsive to treatments, patient should be subjected to intravesical instillations to arrest bleeding. As an absolute last resort, surgery should be considered. BoNT, botulinum toxin; HBOT, hyperbaric oxygen therapy; HC, hemorrhagic cystitis; lipo-tacro, liposome tacrolimus.

Figure 2. Treatment options for the management of HC. The preferred treatment option for HC is dependent on the severity of hematuria. The first step in the treatment of HC is directed toward clot evacuation and hydration to prevent further clot formation. If hematuria persists, continuous bladder irrigation, fulguration, HBOT and, in case of excessive blood loss, blood transfusion should be considered. Novel therapies such as BoNT injections and intravesical lipo-tacro could be implemented at this stage. If unresponsive to treatments, patient should be subjected to intravesical instillations to arrest bleeding. As an absolute last resort, surgery should be considered. BoNT, botulinum toxin; HBOT, hyperbaric oxygen therapy; HC, hemorrhagic cystitis; lipo-tacro, liposome tacrolimus.
… HBOT can be considered as an alternative treatment for patients with underlying ischemia that is unresponsive to conventional therapy.
Reserved for severe and intractable HC, formaldehyde instillation hydrolyzes protein and coagulates superficial bladder mucosa tissue.
More aggressive treatment options to arrest bleeding include selective embolization or ligation of the iliac or bladder arteries.

Figure 3. Schematic illustration of the anti-inflammatory function of tacrolimus in HC. Irradiation-induced lipid peroxidation and CYP metabolism are sources of acrolein. Acrolein enhances Ca2+ absorption, which in turn stimulates calcineurin to dephosphorylate and activate NF-AT. Once activated, NF-AT moves to the nucleus where it induces transcription of pro-inflammatory cytokines. Tacrolimus inhibits NF-AT activity by binding to calcineurin and preventing the dephosphorylation of NF-AT. CMD, calmodulin; Co, transcriptional co-factor; CYP, cyclophosphamide; FKBP-12, FK506-binding protein; Lipo, liposome; NF-AT, nuclear factor of activated T-cell; Tacro, tacrolimus; TNF, tumor necrosis factor.

Figure 3. Schematic illustration of the anti-inflammatory function of tacrolimus in HC. Irradiation-induced lipid peroxidation and CYP metabolism are sources of acrolein. Acrolein enhances Ca2+ absorption, which in turn stimulates calcineurin to dephosphorylate and activate NF-AT. Once activated, NF-AT moves to the nucleus where it induces transcription of pro-inflammatory cytokines. Tacrolimus inhibits NF-AT activity by binding to calcineurin and preventing the dephosphorylation of NF-AT. CMD, calmodulin; Co, transcriptional co-factor; CYP, cyclophosphamide; FKBP-12, FK506-binding protein; Lipo, liposome; NF-AT, nuclear factor of activated T-cell; Tacro, tacrolimus; TNF, tumor necrosis factor.
Bladder instillation of lipo-tacro significantly decreased systemic exposure in comparison with intraperitoneal delivery of tacrolimus.
Main Points
• Hemorrhagic cystitis (HC) is a rare but serious disease that may affect patients after pelvic radiation or systemic chemotherapy. No standard of care therapy is currently available for patients with HC.
• Although not well understood, the inflammation seen in radiation cystitis (RC) consists of three distinct phases: (1) a short acute phase that lasts up to several weeks after radiation therapy; (2) a symptom-free, dose-dependent phase lasting months to years; and (3) a chronic irreversible late-response phase.
• The first step in the treatment of HC is directed toward clot evacuation and hydration, followed by bladder irrigation and/or cystoscopic fulguration of bleeding points if hemorrhaging persists.
• Hyperbaric oxygen therapy (HBOT) has been used in case studies for the management of HC. HBOT can be considered as an alternative treatment for patients with underlying ischemia that is unresponsive to conventional therapy.
• Reserved for severe and intractable HC, formaldehyde instillation hydrolyzes protein and coagulates superficial bladder mucosa tissue. When considering formalin instillation, it is important to first rule out vesicoureteral reflux.
• Promising novel therapies, such as intravesical instillation of liposomal formulation of tacrolimus, improves local drug delivery and may treat the underlying condition of HC.
Main Points
• Hemorrhagic cystitis (HC) is a rare but serious disease that may affect patients after pelvic radiation or systemic chemotherapy. No standard of care therapy is currently available for patients with HC.
• Although not well understood, the inflammation seen in radiation cystitis (RC) consists of three distinct phases: (1) a short acute phase that lasts up to several weeks after radiation therapy; (2) a symptom-free, dose-dependent phase lasting months to years; and (3) a chronic irreversible late-response phase.
• The first step in the treatment of HC is directed toward clot evacuation and hydration, followed by bladder irrigation and/or cystoscopic fulguration of bleeding points if hemorrhaging persists.
• Hyperbaric oxygen therapy (HBOT) has been used in case studies for the management of HC. HBOT can be considered as an alternative treatment for patients with underlying ischemia that is unresponsive to conventional therapy.
• Reserved for severe and intractable HC, formaldehyde instillation hydrolyzes protein and coagulates superficial bladder mucosa tissue. When considering formalin instillation, it is important to first rule out vesicoureteral reflux.
• Promising novel therapies, such as intravesical instillation of liposomal formulation of tacrolimus, improves local drug delivery and may treat the underlying condition of HC.
As of January 2014, 14.5 million cancer survivors (excluding those with carcinoma-in-situ, and basal and squamous cell skin cancers) were living in the United States. This number is expected to rise to 19 million by 2024.1 With this increase in cancer survivors, cancer survivorship medical and social issues are coming to the forefront. One rare but severely debilitating long-term side effect of cancer therapy is hemorrhagic cystitis (HC). Gorczynska and colleagues2 defined HC as the presence of sustained hematuria and lower urinary tract symptoms in the absence of active tumor and other conditions, such as vaginal bleeding, general bleeding diathesis, and bacterial or fungal urinary tract infections. Urologic adverse events caused by HC include frequency, dysuria, urgency, nocturia, suprapubic pain, bladder infection, fatigue, and both microscopic and gross hematuria. Bleeding from HC ranges from nonvisible (or microscopic) hematuria to gross hematuria with clots.3 Moderately severe cases of HC involve massive bleeding and clot formation. Severe HC is a challenging condition to treat and may give rise to serious complications, leading to prolonged hospitalization and/or mortality.3 Even mild cases of HC can cause disabling symptoms, such as frequency, urgency and pelvic pain, focused around the urethra.4
Other than surgery, chemotherapy and radiation therapy are the most commonly used cancer treatments, and both are risk factors for the development of HC. Chemotherapy-induced HC can be a side effect of treatment with cyclophosphamide or ifosfamide.5 These cytotoxic agents are used to treat a wide variety of cancers, including lymphomas, leukemias, sarcomas, germ cell tumors, blastomas, and carcinomas such as bladder, testicular, breast, endometrial, ovarian, cervical, lung, and head and neck cancer. Metabolism of cyclophosphamide and ifosfamide generates acrolein, a compound that is secreted through the urine and can cause urothelial damage upon storage in the bladder.4 HC can also result from pelvic radiation therapy. Radiation directly delivers high-energy particles to the tumor with limited systemic side effects. However, some irradiation-mediated damage to normal tissue is inevitable. HC can be classified as early or late onset,4 and develops weeks to months after treatment in 20% to 25% of patients who receive high-dose cyclophosphamide. The effects of radiation-induced cystitis (RC) can occur as early as 6 months to as late as 20 years after radiation treatment.6
Radiation Toxicity
Standardized scoring scales were generated by the European Organization for Research and Treatment of Cancer and Radiation Therapy Oncology Group (RTOG) to calculate radiation toxicity in different organs. These scales represent subjective, objective, management, and analytical (SOMA) evaluation of late effects to normal tissues (LENT). Each individual organ or tissue known to be within the target irradiation zone, and thus at risk for radiation damage, has its own LENT-SOMA scale. This scale is based on the original RTOG criteria for radiation morbidity.7 The LENT-SOMA scale is a comprehensive system and provides much information, but may be difficult to implement in routine practice outside of clinical studies.8 Advances in radiation therapy, such as high-energy linear accelerators, conformal radiation therapy, and intensity-modulated radiation therapy, allow higher doses of radiation to be delivered to the tumor while sparing surrounding tissues. However, injury to nontarget organs is still prevalent.6
Radiation Cystitis Pathophysiology
Although not well understood, the inflammation seen in RC consists of three distinct phases: (1) a short acute phase that lasts up to several weeks after radiation therapy; (2) a symptom-free, dose-dependent phase lasting months to years; and (3) a chronic irreversible late-response phase.9 In 2014, approximately 60% of cancer survivors who were men and 22% of cancer survivors who were women were previously treated for cancer located in the pelvic region (eg, prostate, cervical, colon/rectal cancer). At least 5% of those treated with radiation therapy are expected to develop RC.6
High-energy radiation can cause cell death through direct absorption of radiation by DNA or indirectly through cell membrane and DNA damage caused by free oxygen radicals, formed through radiolysis of water atoms.5,10 Early symptoms of RC are thought to be due to damage to the bladder urothelium, which has a low cell turnover and thus is highly susceptible to irradiation-induced damage.5,11 Exposure to urine can cause additional irritability and inflammation of the bladder wall. Late radiation injury can take several months to many years to develop, and is largely a function of the total radiation dose and fraction size. The pathologic hallmark of late radiation tissue injury is obliterative endarteritis resulting in atrophy and fibrosis, and subsequently necrosis of the bladder mucosa and hematuria.12 Impaired healing under ischemic conditions can lead to ulcer and fistula formation. Telangiectasia (permanent dilation of blood vessels, usually in the mucous membranes) develops, and can also cause bleeding. Fibrosis forms as part of the repair process and, if severe, can lead to a reduction in bladder capacity (Figure 1).
Diagnosis
Clinical Presentation
Acute RC-related symptoms include dysuria, increased urinary frequency, and urgency. This condition may be self-limiting, and persists up to 3 months after radiation therapy. Management is conservative, with symptomatic relief through anticholinergic drugs. Late RC can develop from 6 months to as late as 20 years after radiation treatment has ended, with a mean latent period of 35 months, according to one study.13
Pre-existing medical conditions, including prior chemotherapy, diabetes, hypertension, and previous unrelated abdominal surgery, may put patients at increased risk for RC. However, the most important risk factors are radiation treatment related, including volume of tissue treated, total bladder dose and fractionation, mode of delivery (external beam and/or brachytherapy), concurrent treatments, and radiosensitivity of the affected bladder tissue.10 Hematuria is the main presenting symptom, and can vary from mild to life-threatening. Hematuria with clot formation can lead to urinary retention. The patient may also present with other lower urinary tract symptoms such as pain, increased frequency, incontinence, and urgency. Possible long-term consequences of radiation on the urinary system are listed in Table 1. Depending on the etiology, patients may present with obstructive lower urinary tract symptoms, including urinary retention secondary to detrusor dysfunction and urethral stricture, the latter being common in men but rare in women. Urinary incontinence can be stress urinary incontinence due to intrinsic sphincter deficiency or urgency incontinence as a result of small bladder capacity and impaired detrusor compliance.
Patient Evaluation
Clinical features of late RC are nonspecific and overlap with symptoms of bladder infection or malignancy. Thus, diagnosis is focused on exclusion of other causes of hematuria. Microscopic hematuria or urinary tract infection can be detected with urinalysis and urine culture. Urine cytology may be considered to detect high-grade malignancies. Disease-focused history should include details of radiation treatment the patient received, including total and daily dose, number of sessions, and radiation delivery technique. Physical examination should focus on evaluating the presence of possible vaginal fistulas. Postvoid residual volume can diagnose underactive bladder and a bladder diary provides an objective assessment of the patient’s symptoms. Radiographic imaging of the kidneys with ultrasound or computed tomography (CT) is recommended and cystoscopy can be performed to rule out urethral pathology, fistula, and cancer. Bladder biopsy may be performed if there is suspicion of tumor, but should be done with great care to avoid perforation of the irradiated bladder wall or cause further bleeding. Urodynamic tests may help to assess cystometric capacity, detrusor compliance, sphincter function, and vesicoureteral reflux.4
Treatment
No standard of care therapy is currently available for patients with HC. There is also a lack of guidelines available on optimal management. Existing HC treatments are regarded as ineffective, risky, or both. Based on current knowledge, the suggested treatment options for HC are reviewed here (Figure 2).
Clot Evacuation and Fulguration
After diagnosis, the choice of therapy depends on the degree of hematuria, and a stepwise approach to treatment should be taken.4 The first step in the treatment of HC is directed toward clot evacuation.14 Bladder outlet obstruction from clots can lead to sepsis and bladder rupture. Clot evacuation is performed by placing a wide-lumen bladder catheter followed by bladder irrigation with water or sodium chloride solution.4
After clot evacuation, patients should be hydrated using intravenous fluids to prevent clot reformation. If hematuria persists, continuous bladder irrigation can be started through a three-way catheter.14 All clots must be removed before starting continuous irrigation to avoid overdistention and potential bladder ruptures.5 If clot evacuation remains unsuccessful, the patient should undergo cystoscopy with clot evacuation and fulguration of bleeding sites.
Cystoscopic Fulguration. Cystoscopy with fulguration of bleeding points is an effective method of treating HC that is unresponsive to conservative measures.15 This procedure can be performed under local anesthesia, especially in women. Methods of fulguration include the use of electrocoagulation, diathermy, and several types of lasers.16,17 Potential morbidity following cystoscopy and cystoscopy with fulguration includes bladder perforation with subsequent fistula formation.18 More severe cases of HC often do not respond to this treatment modality.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) has been used in case studies for the management of HC. The hyperbaric oxygen chamber provides conditions at which hemoglobin is fully saturated and oxygen is dissolved at very high levels in the blood plasma, providing therapeutic benefits such as increased angiogenesis and fibroblast activity in damaged tissues.19 Therefore, HBOT can be considered as an alternative treatment for patients with underlying ischemia that is unresponsive to conventional therapy. Various HBOT regimens have been used: in general, 100% oxygen is administered at 1.5 to 2.5 atm for 45 to 120 minutes, allowing extra time for compression and decompression. Sessions are once daily for a predetermined length of time (usually 20-40 sessions).9
An advantage of HBOT in HC patients is the absence of adverse effects on bladder structure or function that may occur with other therapies (eg, formalin or silver nitrate instillation), while avoiding surgery. However, HBOT is a time-consuming treatment with variable reported response rates (27%-92%) and relatively high recurrence rates (8%-63%).20-23 Side effects of HBOT include oxygen toxicity, which is rare (eg, seizures and alveolar membrane damage), confinement anxiety, ear pain, and digitalis toxicity (if taking drugs). HBOT is not advised in pregnant women as it may increase erythrocyte fragility. Patients with epilepsy must be sedated because oxygen stimulates the central nervous system. When a patient presents with a fever of unknown origin, the etiology must be found before start of therapy.22,23
Intravesical Instillation
If hematuria persists after the treatments described above, bladder instillation can be performed with astringent intravesical agents, including 1% silver nitrate or aluminum sulfate (alum).4 Although the mechanisms of action of these agents vary, the general principles are sterilization, lavage, and arrest of focal bleeding points. The most commonly used agents are alum and formalin.
Aminocaproic Acid. Treatment with epsilon aminocaproic acid, a drug used to treat excessive postoperative bleeding, has been reported in HC.24 However, it can result in the formation of large, hard clots that are difficult to remove. These clots can cause upper tract bleeding and loss of the respective renal unit.24
Alum. Aluminum salts, such as alum, are astringent agents that act by precipitating proteins on the cell surface and in interstitial spaces. Capillary bleeding is arrested in mild cases, but in severe cases the precipitant tends to clot, resulting in clot retention, distension and more hemorrhaging.25 Aluminum levels must be closely monitored in patients with renal insufficiency as increased levels can cause encephalopathy and acidosis.26 Local adverse effects include suprapubic pain and vesical tenesmus. These can be controlled with antispasmodic and/or analgesic drugs.27
Prostaglandins. Intravesical prostaglandins are also used to treat HC. Prostaglandins are cytoprotective and have anti-inflammatory and vasoconstriction properties, but may cause flushing or severe bladder spasms.28
Formaldehyde (Formalin). Reserved for severe and intractable HC, formaldehyde instillation hydrolyzes protein and coagulates superficial bladder mucosa tissue. When considering formalin instillation, it is important to first rule out vesicoureteral reflux. If present, one may proceed only after placing occlusive balloon catheters in each ureter as reflux can lead to bilateral pyelonephrosis with fatal sepsis.29
Formalin has been used in patients with severe refractory RC.29-31 Intravesical formalin instillation is performed under general or local anesthesia. It causes precipitation of cellular proteins in the mucosa, thereby occluding and fixing telangiectasia tissue and small capillaries. However, fixation of the bladder musculature may result in a small, contracted bladder, and fixation of the intramural ureter can also lead to obstruction with subsequent hydronephrosis and renal failure. The most critical factor is administering the proper formalin dilution (1%-4% for 10-30 min is traditionally used).5 Formalin is toxic even in very dilute (1%) concentration.29 In a retrospective study, 1% formalin solution was equally effective in arresting bleeding as 2% or 4% solution, but caused fewer complications. Treatment of hematuria with 10% formalin-soaked pledgets has been reported to be equally effective in arresting bleeding as 4% formalin instillation, with minimal side effects.32 On the contrary, instillation of 5% and 10% formalin solutions have been associated with increased morbidity and mortality.29
Surgical Interventions
In patients with refractory HC, surgical intervention is warranted. More aggressive treatment options to arrest bleeding include selective embolization or ligation of the iliac or bladder arteries.33 Several urinary diversion methods have been used, including temporary bladder exteriorization with packing of the bladder and ileal conduit diversion. Reports suggest that a transverse colon conduit is the preferred method of urinary diversion, which, in RC patients, has the advantage of using the nonirradiated bowel and ureters for creating the diversion. Alternative options for urinary diversion include percutaneous nephrostomy and cutaneous ureterostomy.34 Complications related to the defunctionalized bladder, including pyocystitis, hemorrhage, pain, and neoplastic transformation, occur in over 50% of patients who have undergone urinary diversion35; therefore, cystectomy is recommended at the time of urinary diversion. Preoperative high-dose radiation therapy is a risk factor for postoperative morbidity, particularly enteroenteric fistulas, urointestinal fistulas, and stenosis of the ureterointestinal anastomosis.35 Because of the high morbidity and mortality risk, especially in elderly patients with comorbidities, surgery should be considered as a last resort for refractory HC.36
Developing Treatment Modalities for Hemorrhagic Cystitis
Botulinum Toxin
Botulinum toxin (BoNT) blocks acetylcholine release at neuromuscular junctions, and bladder injection of BoNT is now an approved therapy for neurogenic and idiopathic detrusor overactivity.37 Recent research has shown that it also limits muscle contraction by inhibiting the release of neurotransmitters and the expression of the TRPV1 receptor, and that it suppresses bladder inflammation by preventing the expression of EP4 receptors and cyclooxygenase-2.38,39
Chuang and colleagues40 used BoNT type-A injections as a treatment for RC in six patients refractory to other treatments. Under sedation or local anesthesia, 200 U BoNT type-A was submucosally injected through a cystoscope into 20 sites in the trigone and floor of the bladder. No side effects were noted from the injections. A moderate to significant improvement was achieved in five of the six patients, with mean bladder capacity increasing from 105 mL to 250 mL and mean urinary frequency decreasing from 14 to 11 episodes per day. Although further studies are needed, BoNT injection is a promising therapy to treat patients with RC.40
Intravesical Instillation of Liposome-Tacrolimus
Tacrolimus has been approved by the US Food and Drug Administration as a systemic therapy for inhibiting transplant rejection and as topical ointment for moderate to severe atopic dermatitis. Tacrolimus acts by inhibiting interleukin (IL)-2-dependent T-cell activation and has a direct inhibitory effect on cell-mediated immunity. Tacrolimus is not water soluble, but can be dissolved in hydrophobic solvents.41 The application of liposomal tacrolimus in HC has two targets: (1) tacrolimus inhibits T-cell activation, and (2) tacrolimus causes acute arteriole vasoconstriction.
Mode of Action. Tacrolimus prolongs the survival of the host and transplanted graft in animal transplant models of liver, kidney, heart, bone marrow, small bowel and pancreas, lung and trachea, skin, cornea, and limb. Furthermore, it is occasionally used in the treatment of various immune-mediated diseases. In animals, tacrolimus has been demonstrated to suppress some humoral immunity and, to a greater extent, cell-mediated reactions such as allograft rejection, delayed type hypersensitivity, collagen-induced arthritis, experimental allergic encephalomyelitis, and graft-versus-host disease.42
Tacrolimus is a macrolide antibiotic and acts primarily on T-helper cells, although some inhibition of suppressor and cytotoxic T-cells also seems to occur. Through binding with the FK506-binding protein (FKBP-12), tacrolimus is a competitive inhibitor of calcineurin, a calcium- and calmodulin-dependent phosphatase. This process inhibits the translocation of the NF-AT (nuclear factor of activated T-cells) family of transcription factors, leading to reduced transcriptional activation of early cytokine genes for IL-2, interferon-ɣ, tumor necrosis factor-α, IL-3, IL-4, CD40L, and granulocyte-macrophage colony-stimulating factor (Figure 3).43 Ultimately, proliferation of lymphocytes is reduced. Cyclosporine is an immunosuppressant that also prevents calcineurin from dephosphorylating and activating NF-AT. Although the mode of action of tacrolimus is similar to that of cyclosporine, tacrolimus has been shown to be less nephrotoxic than cyclosporine.44
Effect of Liposome-tacrolimus on Hemorrhagic Cystitis Animal Models. The urothelium is the primary site of tissue damage in the pathophysiology of cystitis.45,46 Recent studies have highlighted overexpression of genes related to immunity and inflammation, including activation of CD4+ T-helper type-1-related chemokines in cystitis.47 Nirmal and associates43 examined levels of tacrolimus in blood, urine, and bladder tissue of rats following exposure to combination liposome-tacrolimus (lipo-tacro) or tacrolimus. Bladder instillation of lipo-tacro significantly decreased systemic exposure in comparison with intraperitoneal delivery of tacrolimus.
The efficacy of lipo-tacro was examined in a model of RC in which rats received a single dose of 40 Gy delivered directly to the bladder using a three-beam CT-targeted irradiator. Radiation treatment significantly reduced intermicturition intervals, which was successfully reversed with a single dose of intravesical lipo-tacro. Six weeks after irradiation, saline-treated rats showed edematous changes with inflammatory cell infiltration and hyperplastic urothelium. In contrast, lipo-tacro treatment showed minimal edematous changes.48 Lipo-tacro also reduced urinary frequency and suppressed inflammation and edema in the bladder mucosa and submucosal layers of a rat model of chemotherapy-induced HC.49 These studies indicate that lipo-tacro is a promising novel treatment for radiation- and chemotherapy-induced HC.
Clinical Experience. Lipo-tacro has not been tested in clinical subjects; however, we recently reported a compassionate use case of intravesical tacrolimus alone in an 81-year-old man with a history of external beam radiation therapy for the treatment of localized prostate cancer.50 The patient has a medical history of atrial fibrillation, coronary artery disease, congestive heart failure, apnea, hypothyroidism, and gastrointestinal bleeding. No prostate cancer recurrence was noted, but the patient developed progressive HC. Past treatments included HBOT, though without adequate or sustained symptom relief.
During the months prior to treatment, the patient required outpatient visits due to gross hematuria. He was admitted to the hospital twice for nearly 30 days requiring catheterization, bladder irrigation, 8 units of blood transfusion for anemia, antibiotics for urinary tract infection, and two surgeries for fulguration of bleeding. Gross hematuria did not resolve, and bladder instillation of formalin was being considered as a last resort. The patient, family, and medical team had concerns of adverse events associated with formalin and elected intravesical tacrolimus instillation.
The patient received two instillations on consecutive days that were well tolerated. Blood tacrolimus levels were 0.8 ng/mL and 2.3 ng/mL 24 hours after instillation respectively (reference range 5.0-15.0 ng/mL). The patient’s gross hematuria diminished and the patient was discharged without gross hematuria after an additional 48 hours of observation. During the next 6 months the patient was able to stay at home without further hematuria.
Stakeholders in Cancer Survivorship and Radiation Cystitis
Despite a growing interest in RC by both the public and medical community, RC is not globally recognized and remains underinvestigated. Patients and their families with this terrible condition are in desperate need of novel therapies and support. The Radiation Cystitis Foundation (http://www.radiationcystitis.org/) is a nonprofit patient advocacy group working to help improve the lives of all those affected by radiation and to advance treatment of RC. The Radiation Cystitis Foundation is the first organization dedicated entirely to RC and consists of a group of dedicated volunteers.
Conclusions
Time is of the essence for patients with HC as no adequate treatment options are available. New therapies, such as intravesical lipo-tacro formulation, are being investigated for the treatment of this rare but serious disease with unmet medical needs. ![]()
Bernadette M.M. Zwaans is a Urology Care Foundation Scholar. Michael B. Chancellor is the founder and Chief Scientific Officer of Lipella Pharmaceuticals, Inc. (Pittsburgh, PA). The remaining authors declare no relevant conflicts of interest.
References
- Cancer treatment & survivorship. Facts & figures 2014-2015. American Cancer Society website. http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-042801.pdf. Accessed January 29, 2016.
- Gorczynska E, Turkiewicz D, Rybka K, et al. Incidence, clinical outcome, and management of virus-induced hemorrhagic cystitis in children and adolescents after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2005;11:797-804.
- Decker DB, Karam JA, Wilcox DT. Pediatric hemorrhagic cystitis. J Pediatr Urol. 2009;5:254-264.
- Payne H, Adamson A, Bahl A, et al. Chemical- and radiation-induced haemorrhagic cystitis: current treatments and challenges. BJU Int. 2013;112:885-897.
- Basler J. Hemorrhagic cystitis. Medscape website. http://emedicine.medscape.com/article/2056130-overview. Updated October 19, 2015. Accessed January 29, 2016.
- Smit SG, Heyns CF. Management of radiation cystitis. Nat Rev Urol. 2010;7:206-214.
- Pavy JJ, Denekamp J, Letschert J, et al. EORTC Late Effects Working Group. Late Effects toxicity scoring: the SOMA scale. Int J Radiat Oncol Biol Phys. 1995;31:1043-1047.
- Power DA. Late effects of radiotherapy: how to assess and improve outcomes. Br J Radiol. 2005;78:150-152.
- Zwaans BM, Chancellor MB, Lamb LE. Modeling and treatment of radiation cystitis [published online Nov. 10, 2015]. Urology. doi: 10.1016/j.urology.2015.11.001.
- Marks LB, Carroll PR, Dugan TC, Anscher MS. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy. Int J Radiat Oncol Biol Phys. 1995;31:1257-1280.
- Lips IM, Dehnad H, van Gils CH, et al. High-dose intensity-modulated radiotherapy for prostate cancer using daily fiducial marker-based position verification: acute and late toxicity in 331 patients. Radiat Oncol. 2008;3:15.
- Denton AS, Clarke NW, Maher EJ. Non-surgical interventions for late radiation cystitis in patients who have received radical radiotherapy to the pelvis. Cochrane Database Syst Rev. 2002;CD001773.
- Wong-You-Cheong JJ, Woodward PJ, Manning MA, Davis CJ. From the archives of the AFIP: inflammatory and nonneoplastic bladder masses: radiologic-pathologic correlation. Radiographics. 2006;26:1847-1868.
- Choong SK, Walkden M, Kirby R. The management of intractable haematuria. BJU Int. 2000;86:951-959.
- Levenback C, Eifel PJ, Burke TW, et al. Hemorrhagic cystitis following radiotherapy for stage Ib cancer of the cervix. Gynecol Oncol. 1994;55:206-210.
- Ravi R. Endoscopic neodymium:YAG laser treatment of radiation-induced hemorrhagic cystitis. Lasers Surg Med. 1994;14:83-87.
- Wines MP, Lynch WD. A new minimally invasive technique for treating radiation cystitis: the argon-beam coagulator. BJU Int. 2006;98:610-612.
- Vicente Rodríguez J, Fariña LA.. Intestinal perforation after treatment of radiation cystitis using the neodymium:YAG laser [in Spanish]. Actas Urol Esp. 1991;15:459-461.
- Capelli-Schellpfeffer M, Gerber GS. The use of hyperbaric oxygen in urology. J Urol. 1999; 162(3 Pt 1):647-654.
- Bevers RF, Bakker DJ, Kurth KH. Hyperbaric oxygen treatment for haemorrhagic radiation cystitis. Lancet. 1995;346:803-805.
- Chong KT, Hampson NB, Corman JM. Early hyperbaric oxygen therapy improves outcome for radiation-induced hemorrhagic cystitis. Urology. 2005;65:649-653.
- Del Pizzo JJ, Chew BH, Jacobs SC, Sklar GN. Treatment of radiation induced hemorrhagic cystitis with hyperbaric oxygen: long-term followup. J Urol. 1998;160(3 Pt 1):731-733.
- Oliai C, Fisher B, Jani A, et al. Hyperbaric oxygen therapy for radiation-induced cystitis and proctitis. Int J Radiat Oncol Biol Phys. 2012;84:733-740.
- Singh I, Laungani GB. Intravesical epsilon aminocaproic acid in management of intractable bladder hemorrhage. Urology. 1992;40:227-229.
- Arrizabalaga M, Extramiana J, Parra JL, et al. Treatment of massive haematuria with aluminous salts. Br J Urol. 1987;60:223-226.
- Phelps KR, Naylor K, Brien TP, et al. Encephalopathy after bladder irrigation with alum: case report and literature review. Am J Med Sci. 1999;318:181-185.
- Goswami AK, Mahajan RK, Nath R, Sharma SK. How safe is 1% alum irrigation in controlling intractable vesical hemorrhage? J Urol. 1993;149:264-267.
- Laszlo D, Bosi A, Guidi S, et al. Prostaglandin E2 bladder instillation for the treatment of hemorrhagic cystitis after allogeneic bone marrow transplantation. Haematologica. 1995;80:421-425.
- Dewan AK, Mohan GM, Ravi R. Intravesical formalin for hemorrhagic cystitis following irradiation of cancer of the cervix. Int J Gynaecol Obstet. 1993;42:131-135.
- Donahue LA, Frank IN. Intravesical formalin for hemorrhagic cystitis: analysis of therapy. J Urol. 1989;141:809-812.
- Lowe BA, Stamey TA. Endoscopic topical placement of formalin soaked pledgets to control localized hemorrhage due to radiation cystitis. J Urol. 1997;158:528-529.
- Lojanapiwat B, Sripralakrit S, Soonthornphan S, Wudhikarn S. Intravesicle formalin instillation with a modified technique for controlling haemorrhage secondary to radiation cystitis. Asian J Surg. 2002;25:232-235.
- De Berardinis E, Vicini P, Salvatori F, et al. Superselective embolization of bladder arteries in the treatment of intractable bladder haemorrhage. Int J Urol. 2005;12:503-505.
- Bondavalli C, Dall’Oglio B, Schiavon L, et al. Complications of urinary diversion after radiotherapy [in Italian]. Arch Ital Urol Androl. 2003;75:10-13.
- Fazili T, Bhat TR, Masood S, et al. Fate of the leftover bladder after supravesical urinary diversion for benign disease. J Urol. 2006;176:620-621.
- Mukhtar S, Woodhouse C. The management of cyclophosphamide-induced haematuria. BJU Int. 2010;105:908-912.
- Duthie JB, Vincent M, Herbison GP, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst Rev. 2011;CD005493.
- Chuang YC, Yoshimura N, Huang CC, et al. Intravesical botulinum toxin A administration inhibits COX-2 and EP4 expression and suppresses bladder hyperactivity in cyclophosphamide-induced cystitis in rats. Eur Urol. 2009;56:159-166.
- Ha US, Park EY, Kim JC. Effect of botulinum toxin on expression of nerve growth factor and transient receptor potential vanilloid 1 in urothelium and detrusor muscle of rats with bladder outlet obstruction-induced detrusor overactivity. Urology. 2011;78:721.e1-721.e6.
- Chuang YC, Kim DK, Chiang PH, Chancellor MB. Bladder botulinum toxin A injection can benefit patients with radiation and chemical cystitis. BJU Int. 2008;102:704-706.
- Patel P, Patel H, Panchal S, Mehta T. Formulation strategies for drug delivery of tacrolimus: an overview. Int J Pharm Investig. 2012;2:169-175.
- De Bruyne R, Bogaert D, De Ruyck N, et al. Calcineurin inhibitors dampen humoral immunity by acting directly on naive B cells. Clin Exp Immunol. 2015;180:542-550.
- Nirmal J, Tyagi P, Chancellor MB, et al. Development of potential orphan drug therapy of intravesical liposomal tacrolimus for hemorrhagic cystitis due to increased local drug exposure. J Urol. 2013;189: 1553-1558.
- Martins L, Ventura A, Branco A, et al. Cyclosporine versus tacrolimus in kidney transplantation: are there differences in nephrotoxicity? Transplant Proc. 2004;36:877-879.
- Erdogan M, Wright JR Jr, McAlister VC. Liposomal tacrolimus lotion as a novel topical agent for treatment of immune-mediated skin disorders: experimental studies in a murine model. Br J Dermatol. 2002;146:964-967.
- van Dieren JM, Lambers ME, Kuipers EJ, et al. Local immune regulation of mucosal inflammation by tacrolimus. Dig Dis Sci. 2010;55:2514-2519.
- Sakthivel SK, Singh UP, Singh S, et al. CXCL10 blockade protects mice from cyclophosphamide-induced cystitis. J Immune Based Ther Vaccines. 2008;6:6.
- Rajaganapathy BR, Janicki JJ, Levanovich P, et al. Intravesical liposomal tacrolimus protects against radiation cystitis induced by 3-beam targeted bladder radiation. J Urol. 2015;194:578-584.
- Chuang YC, Tyagi P, Huang HY, et al. Intravesical immune suppression by liposomal tacrolimus in cyclophosphamide-induced inflammatory cystitis. Neurourol Urodyn. 2011;30:421-427.
- Dave CN, Chaus F, Chancellor MB, Lajness M, Peters KM. Innovative use of intravesical tacrolimus for hemorrhagic radiation cystitis. Int Urol Nephrol. 2015;47:1679-1681.