Preceptor Development Series
An Accelerated, Practice-Based Model for Fostering
Precepting Skills in Pharmacy Residents
Sammuel V. Anderegg, PharmD, MS, BCPS*; Jay C. Christenson, PharmD, MS†; and Carson P. Padgett, PharmD, MS, BCPS‡
Preceptor Development Series
An Accelerated, Practice-Based Model for Fostering
Precepting Skills in Pharmacy Residents
Sammuel V. Anderegg, PharmD, MS, BCPS*; Jay C. Christenson, PharmD, MS†; and Carson P. Padgett, PharmD, MS, BCPS‡
Preceptor Development Series
An Accelerated, Practice-Based Model for Fostering
Precepting Skills in Pharmacy Residents
Sammuel V. Anderegg, PharmD, MS, BCPS*; Jay C. Christenson, PharmD, MS†; and Carson P. Padgett, PharmD, MS, BCPS‡
Abstract
Sound precepting skills are vitally important for all pharmacists and for the future of our profession. Residency training provides a fertile environment for the resident to learn and foster new skills. This article outlines an accelerated model for developing precepting skills in residents and provides helpful advice for residents seeking to gain experience as a preceptor.
Key Words—resident, preceptor development, practice model
Hosp Pharm—2014;2014;49:713–716
Abstract
Sound precepting skills are vitally important for all pharmacists and for the future of our profession. Residency training provides a fertile environment for the resident to learn and foster new skills. This article outlines an accelerated model for developing precepting skills in residents and provides helpful advice for residents seeking to gain experience as a preceptor.
Key Words—resident, preceptor development, practice model
Hosp Pharm—2014;2014;49:713–716
Abstract
Sound precepting skills are vitally important for all pharmacists and for the future of our profession. Residency training provides a fertile environment for the resident to learn and foster new skills. This article outlines an accelerated model for developing precepting skills in residents and provides helpful advice for residents seeking to gain experience as a preceptor.
Key Words—resident, preceptor development, practice model
Hosp Pharm—2014;2014;49:713–716
Hosp Pharm 2014;49(8):713–716
2014 © Thomas Land Publishers, Inc.
doi: 10.1310/hpj4908-713
Residency training is a special experience in the life of a pharmacy professional. It is the one time in the residents’ pharmacy career when they are able to demonstrate and develop clinical knowledge, time management skills, and interpersonal communication techniques while practicing pharmacy, all under the watchful eye of an experienced preceptor. Preceptors give valuable feedback and advice that mold the residents as practitioners and prepares them for the next step in their career. This is an opportune time for the skills of effective preceptors to be passed down to preceptees. The American Society of Health-System Pharmacists (ASHP) requires residents to use the 4 preceptor roles that are employed in practice-based teaching to complete residency expectations.1Residents are extremely talented, highly motivated individuals. New residency graduates often accept jobs that require a portion of their time be dedicated to pharmacy students or residents on rotation. This may be their first experience acting as a primary preceptor. Residency programs should incorporate a structured model for developing preceptor skills for residents.
The American College of Clinical Pharmacy recently released guidelines for resident teaching experiences.2 This article expands on these recommendations and outlines an accelerated model that has worked at one institution and provides helpful advice for residents seeking to gain experience as a preceptor.
MODEL
Residents experience a stepwise evolution from a recently graduated pharmacy student into a well-trained practitioner over the course of postgraduate year 1 (PGY-1). During postgraduate year 2 (PGY-2), residents work on perfecting their skills in an area of specialization. Precepting experience should be integrated into this evolution.
Precepting opportunities need to be pre-coordinated. Pharmacy students and/or PGY-1 residents must be on rotation for PGY-1 and PGY-2 residents to precept. Residency program coordinators and directors should work to make these opportunities available. Opportunities should ideally start after orientation and training. It may take 2 or 3 rotations for the residents to get up to speed on policies, procedures, and operation fundamentals. Once the residents are fully oriented, preceptor training may begin.
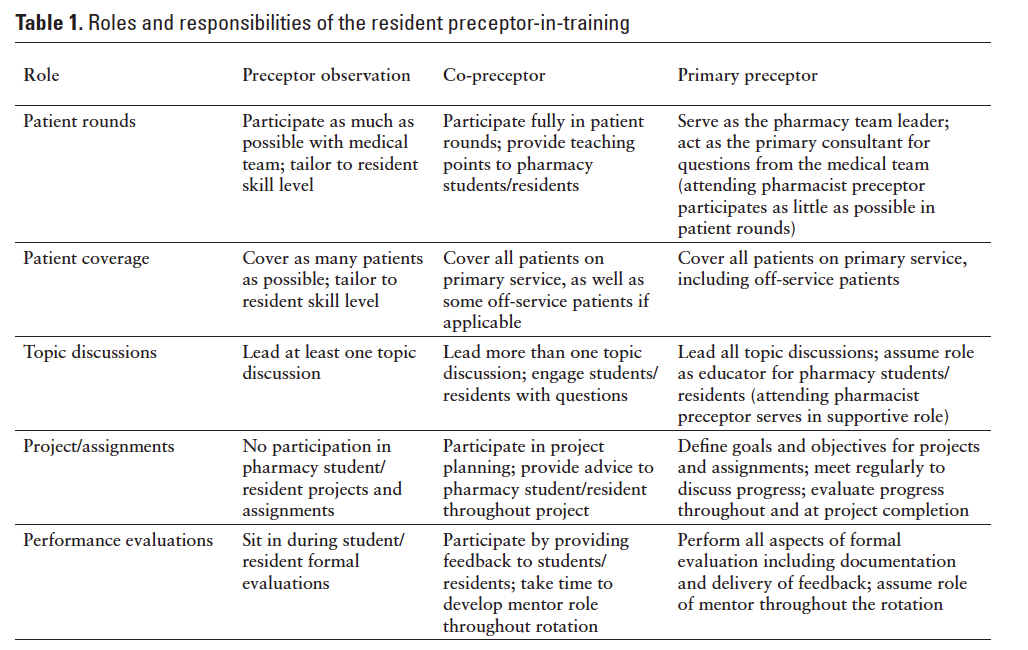
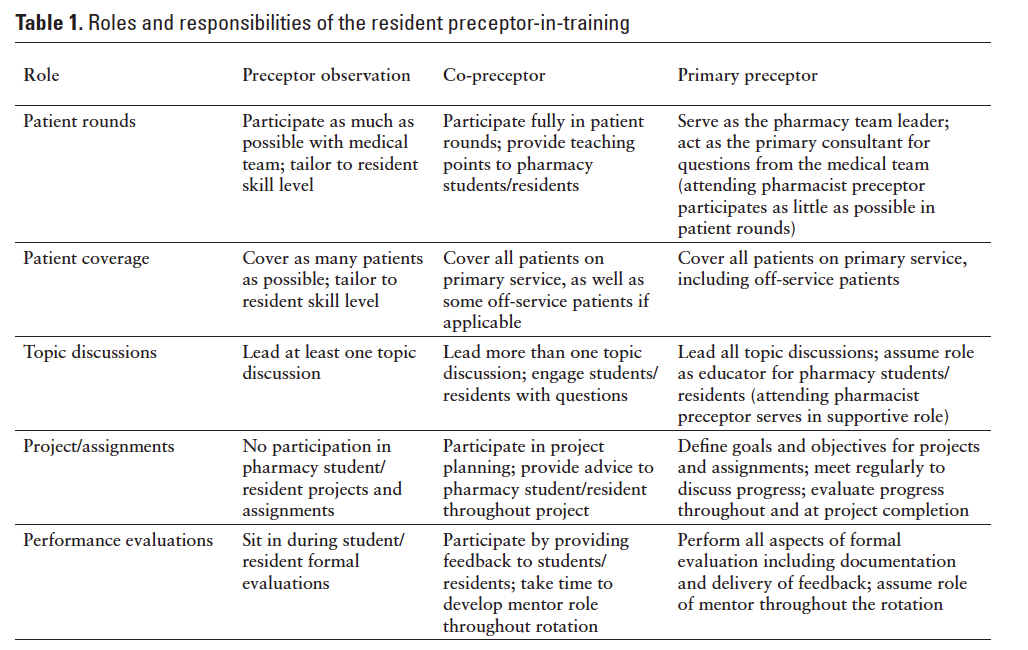
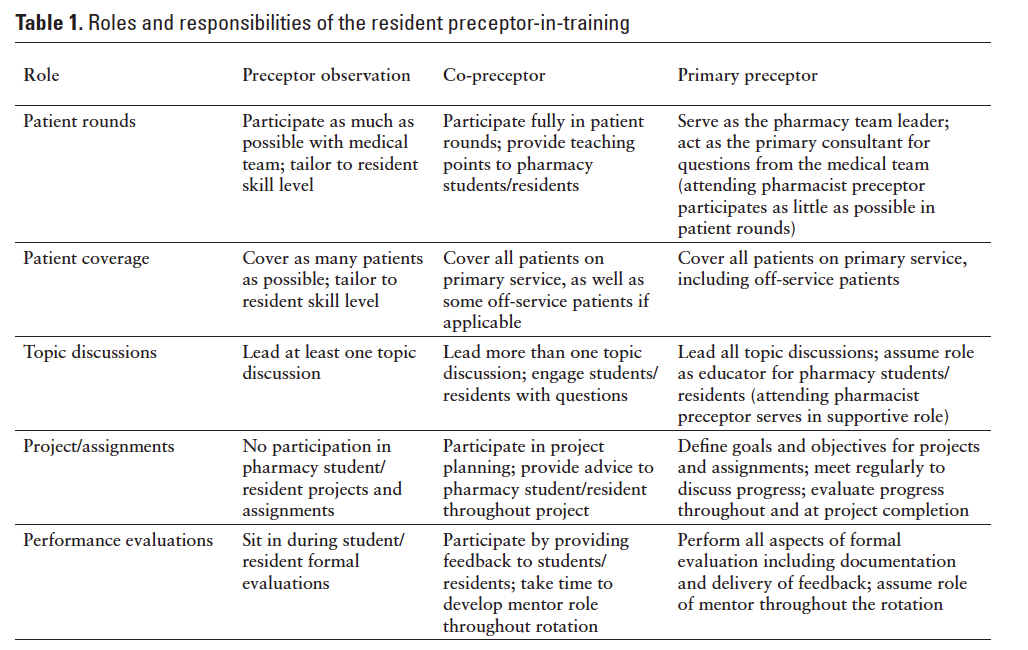
There are 3 stages of development for resident preceptors-in-training: (1) preceptor observation, (2) co-preceptor, and (3) primary preceptor. Each stage has distinct responsibilities and goals (Table 1). Surveys have revealed that staff pharmacists and faculty preceptors believe that residents have varying skill levels and progress at different speeds.3 This model serves as a guideline for planning these stages of training. Residents may repeat stages if needed, with the ultimate goal of serving as a primary preceptor prior to completing their residency.
The PGY-2 precepting experience for residents is more independent. At this point in the resident’s development, they should be fully prepared to independently precept students, begin precepting PGY-1 residents, and assume a leadership role within the pharmacy team. At this stage, they will further develop and fine-tune their precepting skills. Specialty residents have a full year of clinical training under their belt and are focused on refining their knowledge as experts. These individuals are great candidates to precept and mentor incoming PGY-1 residents. The residents can use the experience they gain in student precepting to precept PGY-1s. In addition, PGY-2 residents are able to take on additional responsibilities by precepting students and serving as the team leader. This method is a great way to extend pharmacy services. The PGY-2 resident assumes the team lead responsibilities, reviewing patients with residents and students, taking the lead during medical rounds, delivering advanced topic discussions, and performing evaluations. The attending pharmacist4 preceptor serves in an advisor role. He or she is present during each of these activities and is there to offer input that supplements the specialty residents’ teaching and serves as the final say on clinical decision making. This role frees up the attending pharmacist to spend time on clinical or laboratory research, projects, committee participation, faculty responsibilities, and more. The PGY-2 resident is fully capable of leading the team when the pharmacist is off the floor. This tiered-learning model is paramount for resident development and to elevate department productivity and outreach.
SETTING GOALS AND PLANNING THE ROTATION: WORKING WITH THE ATTENDING PHARMACIST PRECEPTOR
Resident preceptors need to ask themselves what they want to accomplish before starting the precepting experience. Possible objectives include learning to provide constructive feedback, mentoring, improving presentation skills, prioritizing tasks, and organizing each day. Setting clear goals is the best way to make sure the precepting experience is positive for both resident preceptors and students. The goals should be SMART (specific, measurable, attainable, relevant, time bound).5
When meeting with the attending pharmacist preceptor, resident preceptors should be prepared to discuss potential goals for rotation students and PGY-1s (if the resident is a PGY-2) along with the timeline for achieving those goals. The attending pharmacist preceptor should assess the residents’ readiness for providing topic discussions and feedback.
PGY-1 residents are uniquely situated in order to learn precepting skills on a daily basis from their preceptor. By the time the residents have the opportunity to precept on their own, they have already been exposed to several different precepting styles. This allows the residents to take examples and techniques learned from each of their preceptors and combine them to form a unique and personal precepting style. The residents are able to take chances and try out new precepting styles while an attending pharmacist is available to provide guidance. This allows the residents to develop their own style in a supportive environment.
Being Proactive
One of the most challenging parts of residency is time management. To effectively manage a resident schedule and keep on top of projects, residents must be proactive. This can be demonstrated in several ways when precepting. The preceptor, residents, and students need to know what is expected of them prior to starting the rotation. The residents should be proactive in reaching out to their preceptor, providing them with personal goals, and aligning these goals with the goals for the rotation. The resident preceptors should also meet with their students prior to the rotation, if possible. This allows the residents to familiarize themselves with the preceptees and set expectations from the beginning. The students should understand that the resident will be their primary contact as a day to day preceptor, but an experienced mentor preceptor will be available for issues that may arise.
Obtaining Feedback
It is important for the resident preceptors to receive ongoing feedback regarding their precepting. Feedback should not only be given at the end of the rotation or during a midpoint evaluation. Ongoing feedback allows the residents to learn what they are doing well or what needs improvement. Feedback should always be constructive. A simple, “You did a good job” does not allow the residents to learn. The feedback should include specific examples of what they did well and what they should work on. It may be beneficial for the residents to schedule weekly one-on-one meetings with the attending pharmacist preceptor. Scheduled meetings allow time for the attending pharmacist to provide feedback and for the residents to discuss any issues or questions they have.
Providing constructive feedback can be difficult for preceptors with and without precepting experience. One suggestion is to keep in mind how you as a resident or pharmacist would want to have feedback presented. Would you want to have people tell you that you had done a “good job” when you performed well without any constructive feedback? Most pharmacists would prefer to have feedback provided in a way that allows them to learn from what they did and to improve from that experience.
Pearls
- Longitudinal feedback is important. A mentor or member of residency program leadership should assess residents’ progress and provide constructive criticism as they move through the stages of precepting.
- Pharmacy departments should develop a close relationship with affiliated schools of pharmacy to improve coordination of student rotations throughout the year. They should ensure that students are available at opportune times for residents to precept.
- Precepting residents should obtain feedback from students and PGY-1 residents to determine how they have performed. This will be valuable in helping them learn from the experience.
SUMMARY
Precepting is a vital part of the pharmacy profession. Residency training should provide a well-rounded experience and produce a highly qualified candidate, ready to practice in any setting. Residency-trained new practitioners must also be ready to pass what they have learned to the next generation of pharmacists. An accelerated model allows residents to become innately familiar with serving in a precepting role prior to graduation.
ACKNOWLEDGMENTS
The authors have no conflicts of interest to disclose.
REFERENCES
- Required and elective educational outcomes, goals, objectives, and instructional objectives for postgraduate year one (PGY1) pharmacy residency programs, 2nd ed. Effective July 2008. www.ashp.org/menu/Accreditation/ResidencyAccreditation.aspx. Accessed December 31, 2013.
- Havrda DE, Engle JP, Anderson KA, et al. Guidelines for resident teaching experiences. Pharmacotherapy. 2013; 33(7):e147-e161
- Anderson, SL. Precepting opportunities for pharmacy residents. Presented at: American Society of Health-System Pharmacists Midyear Clinical Meeting; December 8, 2013; Orlando, Florida.
- Ashby DM. Permission granted. Am J Health Syst Pharm. 2011;68:1497-1504.
- Doran GT. There’s a S.M.A.R.T. way to write management’s goals and objectives. Manage Rev. 1981;70(11):35-36.

*Pharmacy Manager, Oncology Service Line, Georgia Regents Medical Center, Augusta, Georgia; †Director of Pharmacy, Cumberland Healthcare, Cumberland, Wisconsin; ‡Pharmacy Manager, St. Joseph’s Hospitals, Tampa, Florida. Corresponding author: Sammuel V. Anderegg, PharmD, MS, BCPS, Georgia Regents Medical Center, 1411 Laney Walker Boulevard, AN-2602, Augusta, GA 30912; phone: 706-721-0661; fax: 706-721-0372; e-mail: sanderegg@gru.edu