Preceptor Development Series
Coaching for Success: A Residency Search Primer and
Update for Preceptors and Faculty
David R. Bright, PharmD, BCACP*; Alex J. Adams, PharmD†; Timothy R. Ulbrich, PharmD‡; and Mate M. Soric, PharmD, BCPS§,¶
Preceptor Development Series
Coaching for Success: A Residency Search Primer and
Update for Preceptors and Faculty
David R. Bright, PharmD, BCACP*; Alex J. Adams, PharmD†; Timothy R. Ulbrich, PharmD‡; and Mate M. Soric, PharmD, BCPS§,¶
Preceptor Development Series
Coaching for Success: A Residency Search Primer and
Update for Preceptors and Faculty
David R. Bright, PharmD, BCACP*; Alex J. Adams, PharmD†; Timothy R. Ulbrich, PharmD‡; and Mate M. Soric, PharmD, BCPS§,¶
Abstract
Pharmacy residency programs have become increasingly competitive in recent years, and changes to the residency search and application process have altered the process for matching with a residency. In this article, major residency topics, from the benefits of residency training to searching for and ranking programs, are summarized. A discussion of tips and tricks for applying for residencies and interviewing for positions is included along with specific suggestions developed with data following the implementation of the Pharmacy Online Residency Centralized Application Service (PhORCAS). The article is organized in a question and answer format to help facilitate understanding of key concepts and common questions that may arise from applicants. Many changes have taken place in the residency search and application process in recent years, and the process of obtaining a residency is complex. Residency applicants and those advising applicants may find value in the answers to commonly asked residency application questions to help ensure the greatest chance of a successful residency match.
Key Words—pharmacy student, postgraduate training, preceptor, residency
Hosp Pharm—2015;50:467–476
Abstract
Pharmacy residency programs have become increasingly competitive in recent years, and changes to the residency search and application process have altered the process for matching with a residency. In this article, major residency topics, from the benefits of residency training to searching for and ranking programs, are summarized. A discussion of tips and tricks for applying for residencies and interviewing for positions is included along with specific suggestions developed with data following the implementation of the Pharmacy Online Residency Centralized Application Service (PhORCAS). The article is organized in a question and answer format to help facilitate understanding of key concepts and common questions that may arise from applicants. Many changes have taken place in the residency search and application process in recent years, and the process of obtaining a residency is complex. Residency applicants and those advising applicants may find value in the answers to commonly asked residency application questions to help ensure the greatest chance of a successful residency match.
Key Words—pharmacy student, postgraduate training, preceptor, residency
Hosp Pharm—2015;50:467–476
Abstract
Pharmacy residency programs have become increasingly competitive in recent years, and changes to the residency search and application process have altered the process for matching with a residency. In this article, major residency topics, from the benefits of residency training to searching for and ranking programs, are summarized. A discussion of tips and tricks for applying for residencies and interviewing for positions is included along with specific suggestions developed with data following the implementation of the Pharmacy Online Residency Centralized Application Service (PhORCAS). The article is organized in a question and answer format to help facilitate understanding of key concepts and common questions that may arise from applicants. Many changes have taken place in the residency search and application process in recent years, and the process of obtaining a residency is complex. Residency applicants and those advising applicants may find value in the answers to commonly asked residency application questions to help ensure the greatest chance of a successful residency match.
Key Words—pharmacy student, postgraduate training, preceptor, residency
Hosp Pharm—2015;50:467–476
Hosp Pharm 2015;50(6):467–476
2015 © Thomas Land Publishers, Inc.
doi: 10.1310/hpj5006-467
The practice of pharmacy is becoming increasingly diverse, and more students are pursuing postgraduate training programs to gain a competitive edge in the job market.1 Pharmacy residency programs are the most commonly pursued postgraduate training opportunity.2 In 2014, for example, the American Society of Health-System Pharmacy (ASHP) reported that 4,142 applicants participated in the postgraduate year 1 (PGY1) residency match process, a number that corresponds to roughly 30% of the entry-level doctor of pharmacy graduates in the United States.2,3
In addition to the rising number of residency applicants, the supply of residency programs has increased significantly in recent years. From 2010 to 2014, the number of PGY1 residency positions offered through the National Matching Service has grown from 1,941 to 2,859, a 47% increase.4,5 Similarly, the supply of postgraduate year 2 (PGY2) residency positions has grown by 77%, from 449 in 2010 to 795 in 2014. Even though the number of residency programs has increased over the past several years, the number of applicants has increased to a greater extent, which has led to a large number of unsuccessful residency match applicants. In 2014, 1,502 of the 4,142 applicants (36%) participating in the match were unsuccessful in obtaining a position.
Given the rapid pace of change in pharmacy residency supply and demand, it is imperative that faculty members and preceptors are able to guide and mentor students as they navigate the increasingly diverse maze of postgraduate training opportunities. The purpose of this article is to provide a brief primer and update on the residency search process for preceptors and faculty who advise residency candidates.
What is a pharmacy residency?
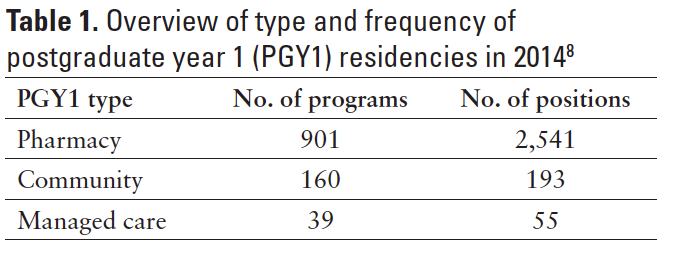
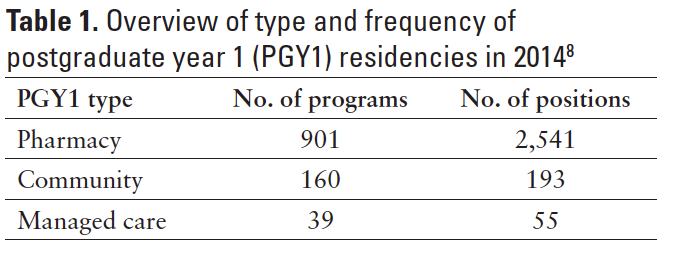
PGY1 residency programs are designed to “build upon knowledge, skills, attitudes, and abilities gained from an accredited professional pharmacy degree program…[and] enhance general competencies in managing medication-use systems.”6 PGY1 residencies fall into 1 of 3 domains: (1) pharmacy (general; most often in a hospital or health system), (2) community, and (3) managed care. In 2014, 89% of all PGY1 positions fell into the pharmacy category.7 Table 1 provides an overview of the number of programs and positions of PGY1 residencies by practice setting.
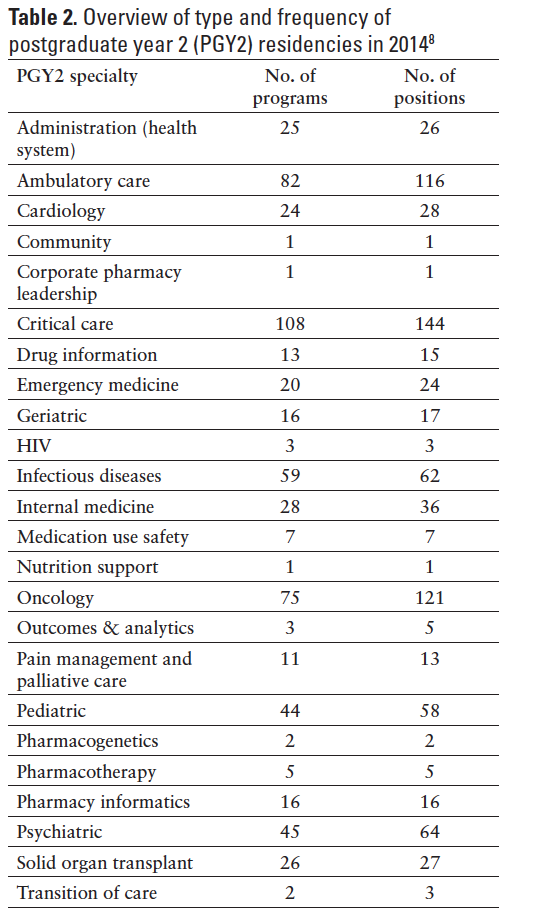
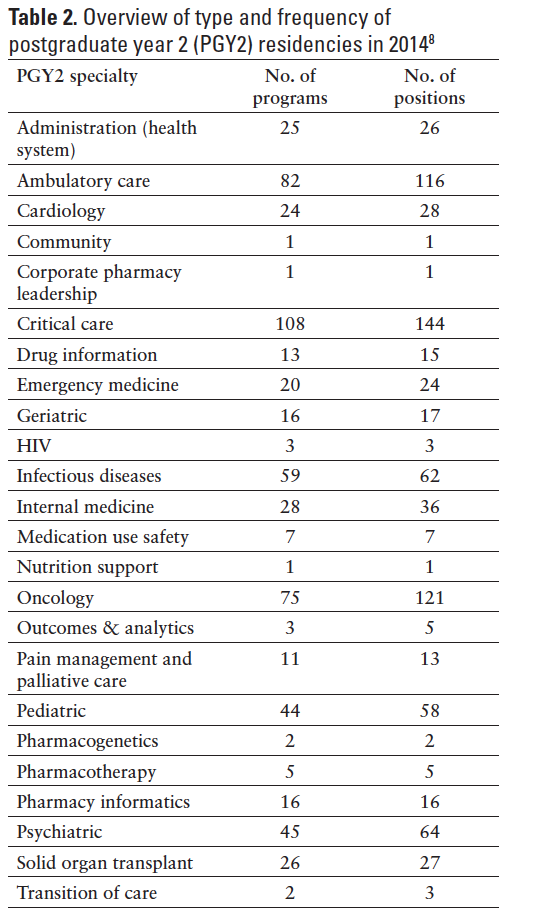
PGY1 graduates seeking to develop specialized expertise in focused areas may pursue a PGY2 residency. Table 2 provides an overview of the types of PGY2 specialties and their frequency. Critical care, oncology, and ambulatory care are the most commonly offered PGY2 residencies, with 144, 121 and 116 positions offered, respectively, in the 2014 match.7,8 Students also may pursue a joint PGY1/PGY2 position. In 2014, there were 70 such positions in the match process including health-system administration and pharmacotherapy.7Some of these programs also confer a master’s degree upon completion.
What benefits can a residency provide for a pharmacist?
ASHP notes that completing a residency offers the following benefits: (a) a competitive advantage in the job market, (b) networking opportunities, (c) a clearer picture for career planning, and (d) a wider professional vision.9 Further, the American Pharmacist Association (APhA) reports that a PGY1 residency is viewed as 3 to 5 years of practice experience.10 Residencies have become a prerequisite for many career opportunities and may impact the career paths of pharmacists.11 Some national organizations, such as the American College of Clinical Pharmacy (ACCP), have stated that by 2020 a pharmacy residency should be a prerequisite for positions focused on direct patient care.8 Despite this call, there is not a professional consensus around required residencies.12 Some states, however, have created specialized designations for advancing the scope of pharmacist’s care where residency training comes into play. California, for example, established an “advanced practice pharmacist” designation that affords a broadened scope of professional practice.13 To become an advanced practice pharmacist in California, an individual must meet 2 out of 3 requirements, one of which includes completing accredited postgraduate residency training where there is at least 50% or more of time spent in direct patient care with interdisciplinary teams.
What is the general timeline for the residency search process?
The residency search timeline may differ depending on whether or not the candidate is searching for programs that participate in the ASHP Resident Matching Program (“Match”).14 The majority of programs participate in the Match, so the timelines described below will refer to programs that participate in the Match. Candidates pursuing programs not participating in the Match should contact the residency program directors for pertinent timeline information.
With the advent of the Pharmacy Online Residency Centralized Application Service (PhORCAS), applicants must be registered with the Match to apply for residencies. Many residency programs have application due dates in December and January; thus it is advised that candidates register for the Match as early as possible following the opening of registration in early November.14,15 Applicants should solicit references and transcripts and prepare other application materials, including a curriculum vitae (CV) and letter of intent, in advance of the program’s specific application deadline to avoid any last-minute problems.
Programs will review application materials and make offers to applicants for interviews. Interviews typically take place in January, February, and early March, as they must be completed when rank listings are due to the National Matching Service, typically within the first week of March. Results of the Match are released to programs and applicants in late March. Applicants who did not match with a residency program may apply to programs that did not match beginning a few days after Match results are released, through a process unofficially referred to as the “scramble.” ASHP recommends that programs wait approximately 10 days after the Match to make offers to candidates, but some programs make offers before this date.16,17
Early commitments are not allowed for PGY1 programs; but if there is mutual interest from a PGY2 program and a PGY1 resident, an early commitment process is allowed for PGY2 programs. In these cases, the PGY1 resident must be a current resident in a PGY1 residency offered by the same sponsor as the PGY2 residency and the PGY1 and PGY2 residencies must be continuous years of employment.18 The final date for receiving letters of agreement for the early commitment of PGY2 positions occurs during the third week of December.
How should the residency search process differ for introductory and advanced students?
Introductory students (those in the first half of their professional training) should focus on the following:
- Identify practice areas of interest through internships and experiential rotations.
- Align internships and rotations with residency sites and/or practice areas of interest.
- Build a professional network through rotations and internships, involvement in professional organizations, and participation in service activities.
- Build a CV and obtain feedback from several faculty or preceptors.
- Shadow pharmacy residents.
- Brainstorm important criteria for selecting a residency program (as discussed below).
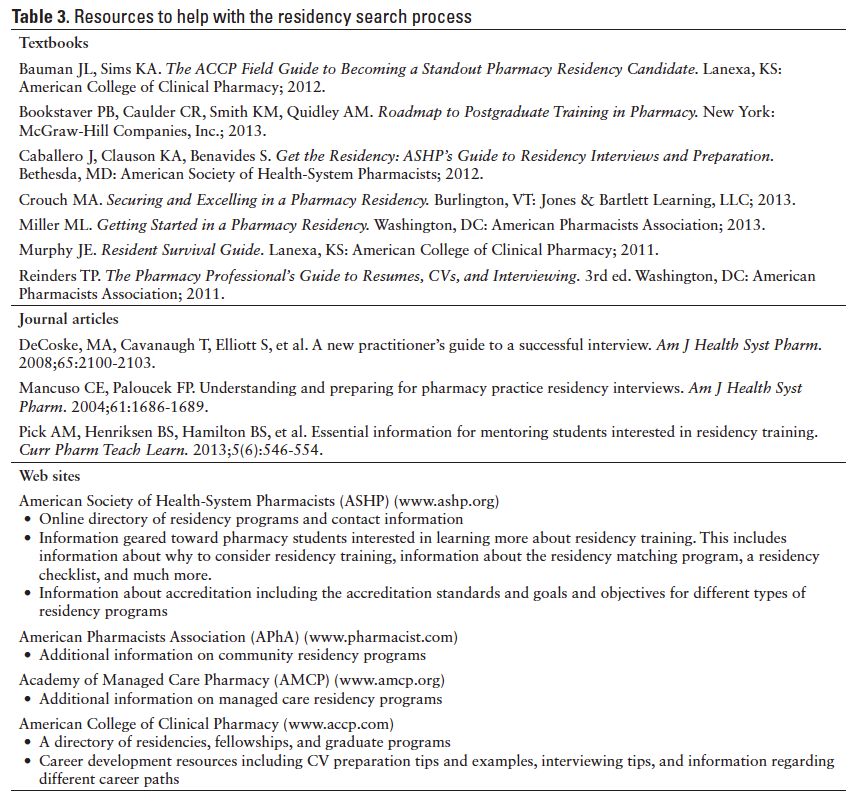
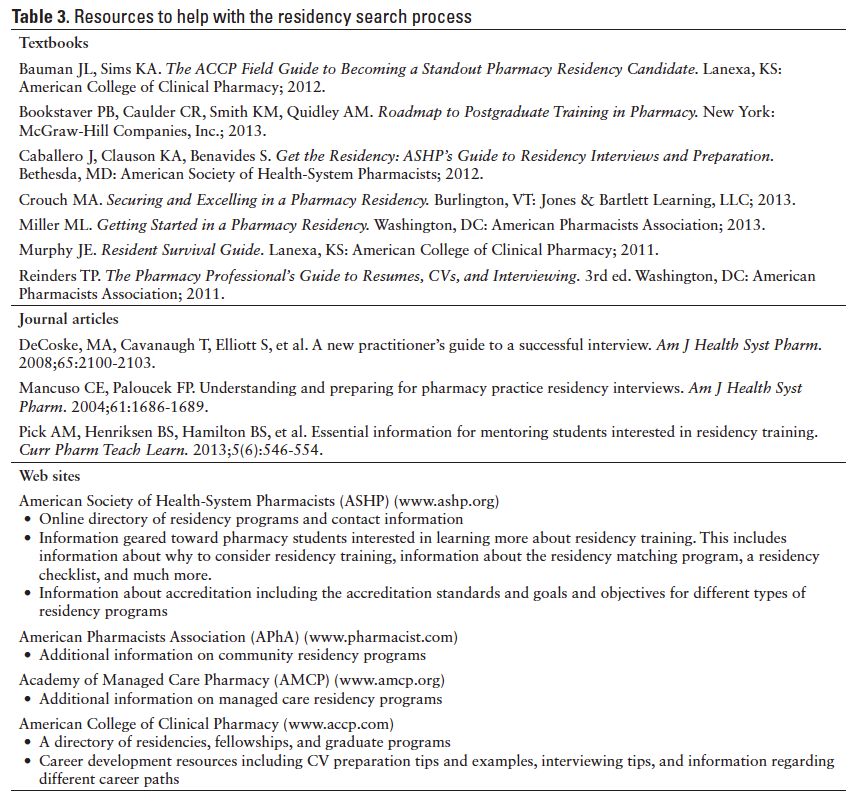
- Learn more about available PGY1 and PGY2 opportunities and the residency search and application process (see Table 3 for information on additional resources helpful in this process).
- Attend local, state, and national meetings to gain exposure to residency programs through job fairs and/or residency showcases.
Assuming they have completed the items listed for introductory students, advanced students (those in the second half of their professional training) should focus on the following:
- Solidify practice area of interest (eg, health system, community, managed care) to focus residency applications and advanced pharmacy practice experiences (APPE).
- When possible, align rotations with residency sites of interest. Considerations should be given to both the type and timing (eg, first half of the final year) to allow for exposure to the site before the application deadline.
- Finalize the CV.
- Draft a letter of intent and obtain feedback from faculty or preceptors.
- Develop a timeline with important deadlines to stay on track during the application process in the final year. This should include application deadlines, goals for finalizing application requirements, and meetings to attend.
What factors should a candidate consider when applying to programs?
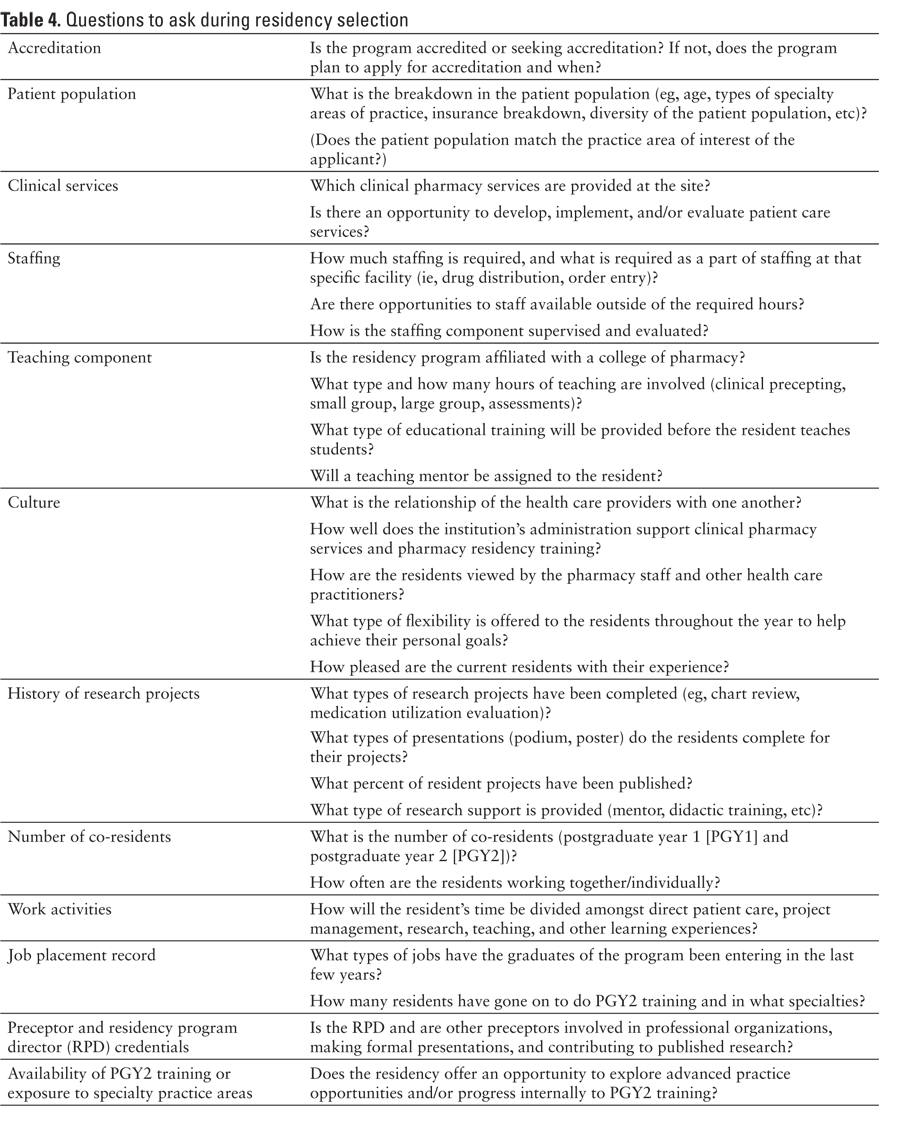
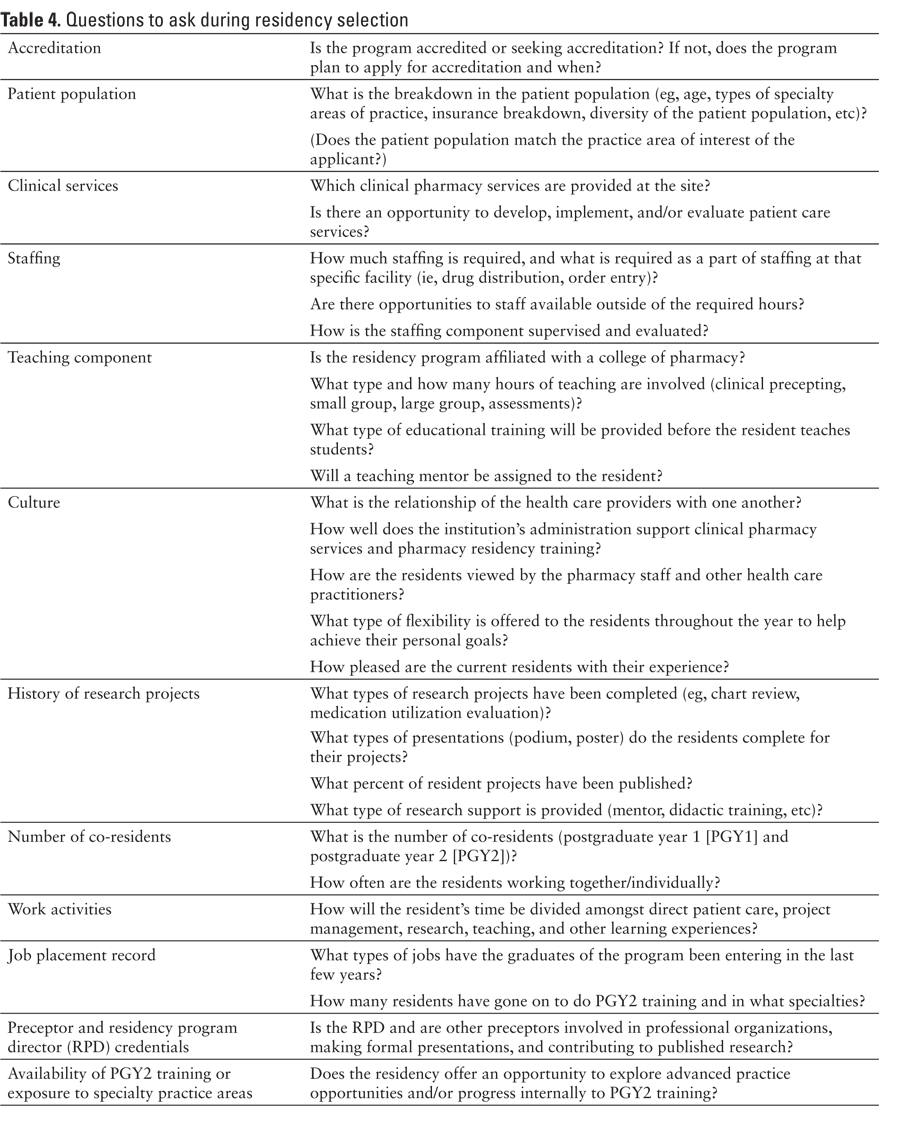
Residency programs should not be viewed as one-size-fits-all. Each applicant needs to spend time identifying the factors that are important to find a residency program that will help him or her work toward achieving career goals. A sample of factors appropriate for consideration are included in Table 4.
Should a resident go to local, state, or national residency showcases?
Local, state, and national residency showcases are a valuable tool for residency candidates to express their interest to a site, make an impression upon that program, and learn more about the program and personnel involved. Although attending showcases is not an absolute to being successful in obtaining a residency position, these events may be valuable.
Showcases come in all shapes and sizes and occur at different times of the year. Examples of residency showcases include local residency showcase or job fairs hosted by a college of pharmacy or local pharmacy association, state residency showcase or job fairs hosted by a state pharmacy association, and national residency showcase (eg, ASHP Midyear Clinical Meeting or APhA Annual Meeting).
To prepare for a residency showcase, applicants should consider the following:
- Have a business card ready to give to the site representative.
- Have a copy of a CV ready in case it is requested.
- Research a site prior to attending the showcase to demonstrate interest in the program and to prepare questions for discussion.
- Prepare an introductory statement (name, current level, college/school attending, reasons for interest in the residency program).
- Approach the site representative with a firm handshake, a smile, and professional attire.
What is PhORCAS?
PhORCAS is the Pharmacy Online Residency Centralized Application Service, which offers programs, applicants, and reference writers a Web site to facilitate the application process. Many, though not all, programs participate in PhORCAS, making it important for applicants to verify the application process of each program. Some programs may require a paper application or an alternative electronic submission system.19 Residency applicants may find it valuable to view instructional videos online for specific instructions on how to apply for programs using PhORCAS.20
What is PPS and how does it impact the application process?
The Personnel Placement Service (PPS) is a residency and job recruitment event that takes place each year at the ASHP Midyear Clinical Meeting. There is a charge for students to participate. Once registration is complete, participants will have access to the PPS position postings on the CareerPharm Web site. Interviewers and interviewees can then contact one another to schedule interview appointments during the ASHP Midyear Clinical Meeting.
PPS schedules approximately 30-minute interviews, which gives the applicant time to leave a more significant impression on the residency site than a shorter interaction at a residency showcase.
Participants should consider the following items for PPS:
- Upload an updated CV on the day the PPS registration opens.
- Contact interviewers as soon as possible, as slots may fill up quickly.
- Schedule interviews with sufficient time between them in case interviews run long and to allow time for reflection.
- Create a spreadsheet with the site, position information, interview time, booth number, and information about the interviewers.
- Bring plenty of CV copies and business cards.
- Follow-up with hand-written thank-you notes.
How many programs should a candidate consider when applying?
For the 2013-2014 residency year match cycle, applicants submitted an average of 7.9 applications. This may serve as a guideline for future applicants, but an individual’s specific circumstances may impact whether or not more applications are warranted.21 For instance, if an applicant is geographically limited and is only seriously considering 4 residencies, there may be little, if any value, in applying to other programs. Alternatively, if a candidate has no geographic restrictions and intends to apply to several highly competitive programs, there may be value in applying to more than 8 programs to increase the chance of getting several interview offers. In addition to the fees for registering in the Match, students should be aware of costs associated with registering with PhORCAS. The initial fees incurred through registration with PhORCAS include the submission of an application to 4 programs; each additional application incurs an additional charge. Other expenses may arise during the interview process, such as the cost of buying professional attire and transportation, meals, and lodging associated with travel to an interview.
What is generally required in an application?
Each residency program may ask for different application materials, so it is very important to consult each program’s information in the ASHP online directory and/or from the program’s Web site or marketing materials for specific instructions. Many programs have set requirements that include a cover letter or letter of intent, a CV, academic transcripts, and references. Some programs may require transcripts from all colleges attended, while others may only want pharmacy school transcripts. Applicants must request that official transcripts be mailed to the PhORCAS transcripts department using the transcript request form through PhORCAS; applicants do not upload transcripts themselves. It may take some institutions several weeks to process transcript orders, so transcript requests should be made well in advance of the application deadline. When using the PhORCAS system, the applicant is able to track reference letter requests and whether or not the reference was successfully submitted, but the applicant is not able to read the reference itself.
What makes a good letter of intent?
Crafting a good letter of intent is one way for a candidate to set himself or herself apart from the competitive group of applicants. The letter of intent serves as an introduction to the candidate’s application, highlights skills and abilities tied to information on the CV, states why the candidate is interested in the position, and provides or refers to any information specifically requested by the program.
Generally speaking, the following “rules” should be followed by the applicant when writing a letter of intent:
- Personalize each letter to the program and organization. The applicant should answer the following question in the letter of intent: “How does the residency program specifically help the applicant achieve his/her career goals.”
- Research the program in detail to tailor the letter appropriately.
- The applicant should make him/herself the subject of each sentence and use active descriptions
(eg, “On this rotation, I demonstrated excellent clinical decision-making skills by…”). - Proofread for spelling, grammar, and punctuation mistakes.
- Keep it concise (1-2 pages maximum).
- Save electronic documents in a pdf format.
In terms of the structure, a general outline follows:
- Paragraph 1: Introduction to the applicant, career goal, statement of interest for applying to the program, how the program will help the applicant achieve his/her career goal, and any special connections
to the program (eg, internships, rotation, etc). - Paragraph 2: An answer to the question of why the applicant is qualified. This paragraph should highlight the most relevant experiences and qualities as they relate to the position for which the applicant is applying.
- Paragraph 3: The closing in which the applicant will refer to the rest of the application (eg, CV, reference letters, transcripts), request an interview, and thank the reader for his/her time and consideration.
What factors do programs consider when reviewing a candidate application?
ASHP recommends that programs institute an objective scoring system to assess applicants, and some common themes are typically seen across programs. Factors such as grade point averages, quality of APPEs, previous work experience, past leadership experiences, and experiences conducting research and presenting at national meetings are seen in over 80% of programs responding to a recent survey.22 The letter of intent and letters of recommendation are generally included in these calculations, as well. Though most programs factor these elements into their selection criteria, processes and scoring can vary dramatically from one program to another.
How should recommendation letter writers be selected?
Applicants should choose writers who have worked closely with them and can speak positively about the experience. It is typically beneficial for applicants to include references who have seen different aspects of their abilities. While a clinical preceptor could comment on patient care skills, a faculty mentor may be better suited to comment on research skills and an employer could focus on communication skills and conflict management. To avoid negative or marginally positive letters, students should objectively review their experiences with a potential writer and determine whether there are any events that could lead to letter of lower quality. Students should ask writers if they would be willing to write a positive letter for them.
Should the residency applicant only look at accredited programs?
ASHP has developed standards of residency education in an effort to support residency programs in producing highly qualified pharmacy manpower.23 Such standards may convey benefit and protection to the resident, as the resident can have a clear expectation in advance of such things as duties and scope of the program, responsibilities of the resident and program, and reasonable duty hour maximums.6,24 As it may take several years for a program to go through the accreditation process, it is not uncommon to see a program that is not accredited by ASHP in a residency search. Although caution may be warranted for programs that are not yet ASHP accredited, not pursuing residencies based on lack of full accreditation may cause an applicant to miss what could be a great fit and opportunity. Due to the recent expansion of new residency programs, it is not uncommon for a student to come across several new programs during his/her residency search process.
Residency programs that are in the process of pursuing accreditation may be noted as having precandidate or candidate accreditation status.23 Furthermore, programs that have applied for accreditation during their first year may not become accredited until the first resident graduates, but future accreditation is retroactive to the date the program applied for candidate status.23 Candidates wishing to pursue board certification through the Board of Pharmacy Specialties and who have residency time counted toward certification must complete a residency that is either accredited by ASHP or that has been granted candidate status by ASHP.25 Although new programs that have not yet had a resident provide less reassurance than an ASHP-accredited program with a long track record, programs pursuing accreditation may still be a reasonable option.
What is a residency teaching certificate program?
Many residencies offer specific learning experiences dedicated to developing skills in teaching and precepting, with some resulting in issuance of a formal teaching certificate.26 These learning experiences may be in the form of a rotation, may be longitudinal, and may differ in content between PGY1 and PGY2 programs.26,27 One study noted that residents were more likely to participate in teaching experiences if their residency was affiliated with a college or school of pharmacy and that residents who eventually became faculty members were more likely to have been a primary preceptor or given lectures during their residency.28 Significant variability exists between programs, so it may be wise for a residency applicant to ask about specific learning experiences related to teaching and precepting within a residency if those experiences are of substantial interest.26,29
What should a candidate expect in an interview?
Interview settings and styles can vary dramatically from one program to another. Most programs will provide a detailed agenda in advance so that the candidate can prepare accordingly. In general, most interviews are conducted at the site hosting the residency, they last roughly a full day, and they are comprised of a series of meetings with various staff members and preceptors, including the program director, administrators, pharmacists, and other health care providers. Pre-interviews or scramble interviews may take place via telephone or video conferencing software, but these methods are rarely used in the typical interview.30 With the large number of students seeking a limited number of residency positions, group interviews are also becoming common. The inclusion of presentations, case work-ups, and other writing assignments are becoming more prevalent, as well. These components allow sites to assess the applicant’s performance under pressure, communication skills, and critical thinking in addition to the usual aspects of organizational fit, goals, and past experiences.
How should a candidate prepare for an interview?
Once a candidate has been accepted for an interview, proper preparation could be the difference between a match and the scramble. A number of publications are available that offer sample questions so applicants can practice their responses and avoid being caught off guard (see Tables 3 and 4). It is generally beneficial to rehearse answers, but students should avoid over-rehearsal (it typically results in robotic, contrived responses). The most memorable answers often include specific examples from the student’s experiences and avoid cliché, cookie-cutter responses that could come from any candidate. For example, instead of using the canned “I chose a career in pharmacy so I can help people” response, it is much more effective to describe an instance where a real patient interaction made the candidate realize the fulfillment that a career in pharmacy can provide.
Behavior-based questions are quickly becoming the norm among programs. These questions require responses that identify a specific instance from the student’s past that illustrate how he or she would handle a situation. Examples include, “Tell me about a time you made a significant intervention on behalf of a patient” or “How have you handled working with a difficult co-worker in the past?” Though these questions make it difficult to provide bland, cliché answers, it is still possible to provide uninspiring or damaging responses.
One of the most error-prone portions of an interview is the time allotted for the candidates to ask questions of their interviewers. Too often, candidates will ask questions about topics that could have been easily obtained in a cursory search of the program, or they fail to ask any questions. This makes the candidates appear to lack interest in the program or lack the initiative to properly prepare for the interview. Questions about hospital size, the presence of certain services, or the number of resident positions should be replaced with questions about the program’s culture, plans for expansion, or other topics less likely to be posted in easily accessed materials.
It is difficult for applicants to prepare for writing assignments and cases, as the topics covered are often not disclosed until the day of the interview. Because it is not feasible to review the entire academic curriculum, candidates should focus their attention on their ability to accurately and succinctly communicate their thoughts in these settings. Presentations are used as a surrogate for overall communication skills. If candidates are allowed to present on a topic of their own choosing, they should ensure the topic is appropriate for the audience.
How should a candidate rank institutions for the Match?
Applicants should carefully consider the order in which they intend to rank positions following their interviews. They may be temped to rank all programs in which they interviewed, but this is ill-advised. To register for the Match, applicants must commit to accepting an appointment for a program with which they match; therefore, applicants should not rank a program if they do not want to be a resident with that program.14
The best strategy for applicants ranking programs for the Match is to develop their rank lists based only on their own preferences. Applicants should not consider the potential rank order of the programs where they interviewed nor should they consider the likelihood of matching with one program over another.31,32 The Match algorithm is designed to be optimal for the applicant, and it provides the best possible outcome for the program 99.9% of the time.31 As registration for the Match requires applicants to not divulge their ranking intentions to programs or solicit ranking information from programs, applicants should not try to “beat” the Match by trying to use other information in rank ordering other than personal preferences for programs.14
What to do in the event of a scramble?
When entering the scramble, a student first must evaluate the list of remaining programs to see if one is available that meets his or her career goals.17,33 Once a program is identified, the same type of preparation used in the first round of interviews should be employed for the scramble. Applicants can begin applying to sites as early as the Monday following the Match. Phone interviews are common in the scramble, but many sites may still require an on-site interview before a final offer can be extended. It is important to note, however, that ASHP has requested programs to comply with a 1-week moratorium on offers after the post-Match process begins, allowing applicants and programs time to evaluate options. Though the moratorium is highly suggested, programs may choose to extend offers during this time period.17
What other resources might be helpful?
Table 3 provides a list of other resources that may be helpful in the residency search process.
CONCLUSION
Many changes to the residency search and application process have occurred in recent years. Although the process of obtaining a residency is complex, it is possible for faculty members to help students navigate the process successfully. Residency applicants, as well as those advising residency applicants, may find substantial value in understanding the search process, so as to maximize the chances of success in matching with a desirable program.
ACKNOWLEDGMENTS
The authors report no known conflicts of interest. Each author is currently serving or has recently served as a residency program director and/or preceptor.
REFERENCES
- American Association of Colleges of Pharmacy (AACP). Graduating student survey summary report – 2014. http://www.aacp.org/resources/research/institutionalresearch/Documents/2014_GSS_Final%20Summary%20Report_All%20Schools_117_for%20web.pdf. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Summary results of the match for positions beginning in 2014. https://natmatch.com/ashprmp/stats/2014applstats.html. Accessed November 7, 2014.
- American Association of Colleges of Pharmacy. Number of degrees conferred 1965-2013 by degree and gender. http://www.aacp.org/resources/research/institutionalresearch/Documents/Fall_13_DegsConferred.pdf. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Summary results of the match for positions beginning in 2014. https://natmatch.com/ashprmp/stats/2014progstats.html. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Summary results of the match for positions beginning in 2010. https://natmatch.com/ashprmp/stats/2010progstats.html. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. http://www.ashp.org/DocLibrary/Accreditation/ASD-PGY1-Standard.aspx. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Summary of programs and positions offered and filled for the 2014 Match. https://natmatch.com/ashprmp/stats/2014summpos.html. Accessed November 7, 2014.
- Murphy J, Nappi J, Bosso J, et al. American College of Clinical Pharmacy’s vision of the future: Postgraduate pharmacy residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;26:722-733.
- American Society of Health-System Pharmacists. Residency checklist. http://www.ashp.org/menu/PracticePolicy/ResourceCenters/Residency/PGY1-Residencies/WhyaResidency.aspx. Accessed November 7, 2014.
- Burns AL. Residencies offer exciting opportunities in community practice. J Am Pharm Assoc. 1999;39(6):748.
- Ulbrich T, Adams A, Bright D, et al. Differences in career paths and attributes of pharmacists completing a community pharmacy residency program (CPRP). Innov Pharm. 2014;Article 178.
- Bright DR, Adams AJ, Black CD, Powers MF. The mandatory residency dilemma: Parallels to historical transitions in pharmacy education. Ann Pharmacother. 2010;44:1793-1799.
- National Association of Boards of Pharmacy. California expands scope of pharmacy practice with new law. http://www.nabp.net/news/california-expands-scope-of-pharmacy-practice-with-new-law. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Applicant registration. https://www.natmatch.com/ashprmp/applregister.html
- American Society of Health-System Pharmacists. PhORCAS 3.0. http://www.ashp.org/DocLibrary/Accreditation/NPPC-on-WebAdMIT.pdf. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Information for programs. https://www.natmatch.com/ashprmp/proglanding.html. Accessed November 7, 2014.
- May JR, Chan J, Fuller PD, et al. Residency scramble: program directors’ experiences with the Pharmacy Online Residency Centralized Application Service. Am J Health Syst Pharm. 2014;71:e1-5.
- American Society of Health-System Pharmacists. Early commitment process for positions in PGY2 programs. https://www.natmatch.com/ashprmp/aboutecp.html. Accessed November 7, 2014.
- Pharmacy Online Residency Centralized Application Service. Portal. https://portal.phorcas.org/. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Pharmacy online residency centralized application service. http://www.ashp.org/phorcas. Accessed November 7, 2014.
- American Society of Health-System Pharmacists.
The Communiqué. http://www.ashp.org/DocLibrary/Accreditation/Communiqu-Newsletter/Spring2013.pdf. Accessed November 7, 2014. - Jellinek-Cohen SP, Cohen V, Bucher KL, et al. Factors used by pharmacy residency programs to select residents. Am J Health Syst Pharm. 2012;69:1105-1108.
- American Society of Health-System Pharmacists. ASHP regulations on accreditation of pharmacy residencies. http://www.ashp.org/DocLibrary/Accreditation/ASD-Accreditation-Regulations-Residencies.aspx. Accessed November 7, 2014.
- American Society of Health-System Pharmacists. Pharmacy specific duty hours requirements for the ASHP Accreditation Standards for Pharmacy Residencies. http://www.ashp.org/doclibrary/accreditation/regulations-standards/duty-hours.aspx. Accessed November 7, 2014.
- Board of Pharmacy Specialties. Fall 2014 candidate’s guide. http://bpsweb.org/pdfs/fall2014_CandidatesGuide.pdf. Accessed November 7, 2014.
- Manasco KB, Bradley AM, Gomez TA. Survey of learning opportunities in academia for pharmacy residents. Am J Health Syst Pharm. 2012;69:1410-1414.
- Medina MS, Herring HR. An advanced teaching certificate program for postgraduate year 2 residents. Am J Health Syst Pharm. 2011;68:2284-2286.
- McNatty D, Cox CD, Seifert CF. Assessment of teaching experiences completed during accredited pharmacy residency programs. Am J Pharm Educ. 2007;71(5):Article 88.
- Havrda DE, Engle JP, Anderson KC, et al. ACCP white paper: Guidelines for resident teaching experiences. Pharmacotherapy. 2013;33(7):e147-161.
- Temple ME, Lagzdins M. Streamlining the residency interview process using Web-based teleconferencing. Am J Health Syst Pharm. 2014;71:e32-35.
- Nagarkar PA, Janis JE. Fixing the “match”: How to play the game. J Grad Med Educ. 2012;4(2):142-147.
- American Society of Health-System Pharmacists. The matching algorithm. https://www.natmatch.com/ashprmp/aboutalg.html. Accessed November 7, 2014.
- May JR, Chan J, Choudhary K, et al. Coping with the residency scramble: The need for national guidelines. Am J Health Syst Pharm. 2012;69:253-255.

*Assistant Professor of Pharmacy, Ferris State University College of Pharmacy, Big Rapids, Michigan; †Vice President, Pharmacy Programs, National Association of Chain Drug Stores, Alexandria, Virginia; ‡Associate Dean for Workforce Development and Practice Advancement, Director of Pharmacy Resident Education, Associate Professor of Pharmacy Practice, Northeast Ohio Medical University, Rootstown, Ohio; §Assistant Professor of Pharmacy Practice, Northeast Ohio Medical University, Rootstown, Ohio; ¶Clinical Pharmacist, Internal Medicine, University Hospitals Geauga Medical Center, Rootstown, Ohio. Corresponding author: David R. Bright, PharmD, BCACP, Assistant Professor of Pharmacy, Ferris State University College of Pharmacy, 220 Ferris Drive, Big Rapids, MI 49307; phone: 231-591-2231; e-mail: davidbright@ferris.edu