Cancer Chemotherapy Update
Drug Monographs: Belinostat and Idelalisib
Whitney L. Piper, PharmD*; J. Aubrey Waddell, PharmD, FAPhA, BCOP;
and Dominic A. Solimando, Jr, MA, FAPhA, FASHP, BCOP
Cancer Chemotherapy Update
Drug Monographs: Belinostat and Idelalisib
Whitney L. Piper, PharmD*; J. Aubrey Waddell, PharmD, FAPhA, BCOP;
and Dominic A. Solimando, Jr, MA, FAPhA, FASHP, BCOP
Cancer Chemotherapy Update
Drug Monographs: Belinostat and Idelalisib
Whitney L. Piper, PharmD*; J. Aubrey Waddell, PharmD, FAPhA, BCOP;
and Dominic A. Solimando, Jr, MA, FAPhA, FASHP, BCOP
The complexity of cancer chemotherapy requires pharmacists be familiar with the complicated regimens and highly toxic agents used. This column reviews various issues related to preparation, dispensing, and administration of antineoplastic therapy, and the agents, both commercially available and investigational, used to treat malignant diseases. Questions or suggestions for topics should be addressed to Dominic A. Solimando, Jr, President, Oncology Pharmacy Services, Inc., 4201 Wilson Blvd #110-545, Arlington, VA 22203, e-mail: OncRxSvc@comcast.net; or J. Aubrey Waddell, Professor, University of Tennessee College of Pharmacy; Oncology Pharmacist, Pharmacy Department, Blount Memorial Hospital, 907 E. Lamar Alexander Parkway, Maryville, TN 37804, e-mail: waddfour@charter.net.
Name: Belinostat
Synonyms: Beleodaq, PXD101
The complexity of cancer chemotherapy requires pharmacists be familiar with the complicated regimens and highly toxic agents used. This column reviews various issues related to preparation, dispensing, and administration of antineoplastic therapy, and the agents, both commercially available and investigational, used to treat malignant diseases. Questions or suggestions for topics should be addressed to Dominic A. Solimando, Jr, President, Oncology Pharmacy Services, Inc., 4201 Wilson Blvd #110-545, Arlington, VA 22203, e-mail: OncRxSvc@comcast.net; or J. Aubrey Waddell, Professor, University of Tennessee College of Pharmacy; Oncology Pharmacist, Pharmacy Department, Blount Memorial Hospital, 907 E. Lamar Alexander Parkway, Maryville, TN 37804, e-mail: waddfour@charter.net.
Name: Belinostat
Synonyms: Beleodaq, PXD101
The complexity of cancer chemotherapy requires pharmacists be familiar with the complicated regimens and highly toxic agents used. This column reviews various issues related to preparation, dispensing, and administration of antineoplastic therapy, and the agents, both commercially available and investigational, used to treat malignant diseases. Questions or suggestions for topics should be addressed to Dominic A. Solimando, Jr, President, Oncology Pharmacy Services, Inc., 4201 Wilson Blvd #110-545, Arlington, VA 22203, e-mail: OncRxSvc@comcast.net; or J. Aubrey Waddell, Professor, University of Tennessee College of Pharmacy; Oncology Pharmacist, Pharmacy Department, Blount Memorial Hospital, 907 E. Lamar Alexander Parkway, Maryville, TN 37804, e-mail: waddfour@charter.net.
Name: Belinostat
Synonyms: Beleodaq, PXD101
Hosp Pharm 2014;49(11):1009–1013
2014 © Thomas Land Publishers, Inc.
doi: 10.1310/hpj4911-1009
MECHANISM OF ACTION
Belinostat is a low-molecular-weight inhibitor of histone deacetylase (HDAC).1-8 HDAC alters gene expression by removing acetyl groups from histones. Inhibition of HDAC suppresses transcription resulting in cell cycle arrest and apoptosis as well as inhibition of angiogenesis.3-8 Belinostat works at both the type 1 and type 2 isoforms specific to malignant cells.1,4,5
PHARMACOKINETICS
Following a 30-minute infusion of 900 mg/m2, the peak concentration (Cmax) is 31,308 ± 9,443 ng/mL. The mean area under the time versus concentration curve (AUC) is AUC0-5 hours 21,796 ± 5,490 h•ng/mL and AUC0-24 hours 22,267 ± 5,485 h•ng/mL with a clearance of 70.5 ± 17.9 L/h. The volume of distribution is 409 ± 76.7 L. The time to peak concentration (Tmax) occurs at 0.42 hours; the terminal half-life (t½) is 4.07 ± 0.39 hours.8
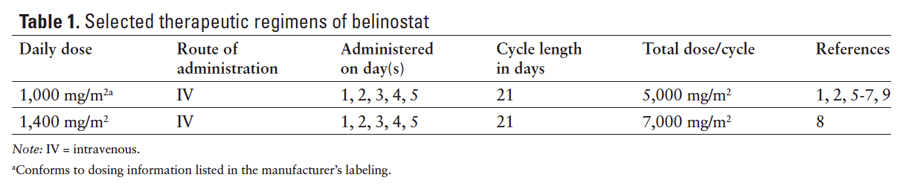
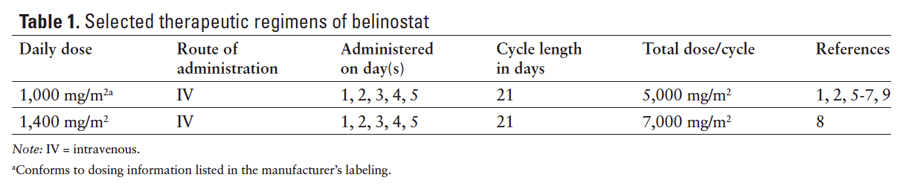
Following a 30-minute infusion of 1,000 mg/ m2, the peak concentration (Cmax) is 127.6 ± 43.5 µmol/L. The AUC is 102 ± 58.3 h•µmol/L. The steady state volume of distribution is 22.6 ± 9.7 L/m2 with a clearance of 41.1 ± 22.2 L/h/m2.4 In another report following a 30-minute infusion of 1,000 mg/m2, the peak concentration (Cmax) is 32,124 ± 9,128 ng/mL. The AUC is 9,990 ± 3,420 ng•h/mL.7 The steady state volume of distribution is 113.9 ± 60.9 L/m2 with a clearance of 110.5 ± 34.4 L/h/m2.7 The half-life (t½) is 1 ± 0.1 hour.4 Belinostat is metabolized in the liver, primarily through glucuronidation by UGT1A1 and, to a lesser extent, oxidation by CYP2A6, CYP2C9, and CYP3A4. About 40% of a dose is excreted renally, primarily as metabolites, with 0.2% to 2% excreted as the parent drug.7 Selected therapeutic regimens of belinostat appear in Table 1.
PREPARATION
A. Follow institutional policies for preparation of hazardous medications when preparing belinostat.
B. Reconstitute the drug with sterile water for injection to a concentration of 50 mg/mL.
C. Dilute the solution in 250 mL of 0.9% sodium chloride injection (NS) or 5% dextrose in water.
STABILITY
A. The reconstituted vial is stable up to 12 hours at controlled room temperature (15ºC-25ºC [59ºF-77ºF]).
B. Solutions diluted for infusion are stable at controlled room temperature (15ºC-25ºC [59ºF-77ºF]) for up to 36 hours.
ADMINISTRATION
A. Belinostat is given as a 30-minute intravenous (IV) infusion.1-8
B. Belinostat should be infused through a 0.22 micron filter.
TOXICITIES
A. Cardiovascular: Atrial fibrillation (all grades) 6%7; dehydration (grade 3) 5%8; edema, limb (grade 1 or 2) 17%,8 (grade 3) 2%8; flushing (grade 1) 10% to 25%,3,7 (grade 2) 20%3; QT prolongation (grade 1 or 2) 2%,8 (grade 2) 5% to 20%,1,2 (grade 3) 5% to 12%,2,8 (grade 3 or 4) 5%1; hemorrhage (grade 3) 5%8; hypotension (grade 2) 5% to 8%,2,6 (grade 3) 5%2; sinus bradycardia (grade 1 or 2) 19%5; supraventricular arrhythmia (grade 2) 15%, (grade 3) 8%6;thrombosis (grade 3 or 4) 9%5;vasculitis (grade 3) 10%.3
B. Central Nervous System: Confusion (grade 2) 5%1;dizziness (grade 1 or 2) 21%8; headache (grade 1 or 2) 16%,5 (grade 3 or 4) 5%1; insomnia (grade 1 or 2) 29%.8
C. Constitutional: Fatigue (grade 1) 10% to 13%,3,7 (grade 2) 2% to 19%,1,2,3,7 (grade 1 or 2) 11% to 69%,1,5,8 (grade 3) 15%,6 (grade 3 or 4) 10%1; fever (grade 1 or 2) 10%,8 (grade 2) 5%2; lethargy (grade 1) 17%,7 (grade 2) 4%7; pain (grade 2) 2% to 8%2,6; sweating (grade 2) 8%6; weight gain (grade 2) 2%.2
D. Dermatologic: Injection site reactions (grade 1 or 2) 48%,8 (grade 2) 10%2;rash (grade 1 or 2) 10%.8
E. Endocrine/Metabolic: Hyperglycemia (grade 2) 46%,6 hypoalbuminemia (grade 2) 5% to 8%,1,6 hypokalemia (grade 3) 10%,3 hyponatremia (grade 3) 10% to 23%,3,6 hypophosphatemia (grade 2) 2%.2
F. Gastrointestinal: Abdominal pain (grade 1 or 2) 29%,8 (grade 3) 7%,8 (grade 4) 2%8; anorexia (grade 1 or 2) 33%,8 (grade 2) 7% to 15%,2,6 (grade 3) 2%8; constipation (grade 1 or 2) 33%,8 (grade 1) 13%,7 (grade 2) 8% to 14%1,7; diarrhea (grade 1) 4% to 20%,3,7 (grade 2) 8% to 10%,1,7 (grade 1 or 2) 19% to 28%,5,8 (grade 3) 2%8; distension (grade 1 or 2) 12%,8 (grade 3) 5%8; dyspepsia (grade 2) 5%1;mucositis (grade 1 or 2) 12%8; nausea (grade 1) 30% to 42%,3,7 (grade 2) 7% to 25%,2,3,6,7 (grade 1 or 2) 33% to 59%,5,8 (grade 3) 2%8; taste alteration (grade 1 or 2) 10%8;vomiting (grade 1) 10% to 54%,3,7 (grade 2) 2% to 21%,2,3,7 (grade 1 or 2) 33% to 34%,5,8 (grade 3) 7%8; xerostomia (grade 3) 10%.3
G. Genitourinary: Urinary frequency (grade 1 or 2) 10%.8
H. Hematologic: Anemia (grade 1 or 2) 13%,5 (grade 2) 7% to 46%,1,2,6 (grade 3) 2%,8 (grade 4) 5%,8 (grade 3 or 4) 24%1; febrile neutropenia (grade 3 or 4) 5%1; leukopenia (grade 1 or 2) 6%,5 (grade 2) 7%2; lymphopenia (grade 2) 8% to 10%,2,6 (grade 3) 10%,2,3 (grade 4) 2%2; neutropenia (grade 2) 5% to 19%,1,2 (grade 3 or 4) 48%1; thrombocytopenia (grade 1) 19%,1 (grade 2) 2%, 2 (grade 3 or 4) 52%.1
I. Hepatic: Hyperbilirubinemia (grade 3) 10%8; increased alkaline phosphatase (grade 1 or 2) 3%,5 (grade 3 or 4) 3%5; increased aspartate aminotransferase (AST) (grade 3) 8% to 10%3,6; increased transaminases (grade 2) 2%.2
J. Hypersensitivity: (grade 1 or 2) 6% to 7%,5,8 (grade 2) 2% to 8%,2,6 (grade 3) 2%,8 (grade 3 or 4) 3%5; cytokine-release syndrome (grade 2) 10%.1
K. Infection: Infection (grade 2) 5% to 15%,2,6 (grade 3) 2%2; pneumonia (grade 2) 5%.1
L. Musculoskeletal: Myalgia (grade 2) 5%.1
M. Neurologic: Hyperesthesia (grade 2) 2%,2 paresthesia (grade 3) 10%,3 sensory peripheral neuropathy (grade 1 or 2) 16%.5
N. Pulmonary: Cough (grade 1 or 2) 10%8; dyspnea (grade 1 or 2) 10%,8 (grade 2) 10% to 23%,1,6 (grade 3) 8%,6 (grade 4) 8%6; hiccups (grade 2) 5%,1 (grade 1 or 2) 17%,8 (grade 3) 2%8;hypoxia (grade 4) 8%6;pneumonitis (grade 1 or 2) 6%.5
O. Renal: Serum creatinine (SCr) elevations (grade 2) 8%,6 (grade 3) 10%.3
Name: Idelalisib
Synonyms: Zydelig, GS-1101
MECHANISM OF ACTION
Idelalisib is an oral phosphatidylinositol-3- kinase (PI3-K) inhibitor that is highly specific for the δ isoform.10-14 The PI3-K δ pathway demonstrates a substantial role in B-cell receptor signaling as well as B-lymphocyte expression.10,11 B-cell malignancies have demonstrated an up-regulation of the PI3-K-δ kinase. Inhibition of the PI3-K pathway decreases cell proliferation, motility, and survival.11,13
PHARMCOKINETICS
Idelalisib displays linear pharmacokinetics.11 Twice daily dosing maintained a continuous plasma exposure when daily dosing did not.10 The Tmax occurs 1.5 hours after oral administration; the terminal elimination t½ is 8.2 hours.15 Steady state is achieved at day 8.10,11,14 Administration with a high-fat meal increases the AUC about 40%. Idelalisib is highly (>84%) bound to plasma proteins, with a steady-state volume of distribution (Vd) of 23 L and a clearance of 14.9 L/h. The drug is metabolized primarily by aldehyde oxidase and CYP3 to a major metabolite (GS-563117), with minor metabolism by UGT1A4. Idelalisib is eliminated 78% in the feces and 14% in the urine. GS-563117 is 49% excreted in the urine and 44% in the feces.15
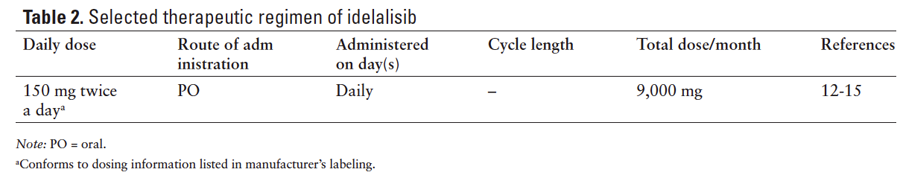
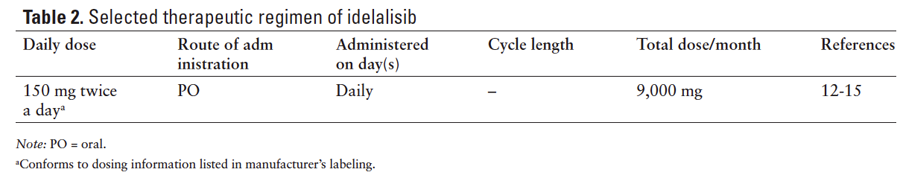
Selected therapeutic regimen of idelalisib is shown in Table 2.
PREPARATION
A. Follow institutional policies for preparation of hazardous medications when dispensing idelaisib.
B. Idelalisib is available as 100 mg and 150 mg tablets.
C. The manufacturer recommends the tablet should be swallowed whole.
D. The manufacturer recommends storing the drug in its original container.
STABILITY
Idelalisib can be stored at temperatures ranging from 68oF-86oF (20oC-30oC).
ADMINISTRATION
Idelalisib is taken twice a day orally with or without food.
TOXICITIES
A. Cardiovascular: Peripheral edema (all grades) 10% to 20%,11,13 (grade 3 or 4) 2%.13
B. Central Nervous System: Dizziness (all grades) 17%14; headache (all grades) 10% to 20%,13,14 (grade 3 or 4) 1%13; insomnia (all grades) 8% to 10%.11
C. Constitutional: Asthenia (all grades) 11% to 33%,13,14 (grade 3 or 4) 2%13; chills (all grades) 8% to 20%11; fatigue (all grades) 20% to 50%,11,13,14 (grade 3 or 4) 2%13; night sweats (all grades) 10% to 11%11,13; pyrexia (all grades) 17% to 50%,11,13,14 (grade 3 or 4) 2%13; weight loss (all grades) 14% to 17%.13,14
D. Dermatologic: Rash (all grades) 13% to 40%,11,13,14 (grade 3 or 4) 2% to 20%.13,14
E. Endocrine/Metabolic: Decreased glucose (all grades) 17% to 40%,11 (grade 3 or 4) 8%11; increased glucose (all grades) 20% to 50%,11,14 (grade 3 or 4) 8%.11
F. Gastrointestional: Abdominal pain (all grades) 16%,13 (grade 3 or 4) 2%13; anorexia (all grades) 17% to 18%,13,14 (grade 3 or 4) 1% to 17%13,14; constipation (all grades) 20% to 50%11, 14; diarrhea (all grades) 40% to 50%,11, 13,14 (grade 3 or 4) 8% to 17%11, 13,14; nausea (all grades) 10% to 50%,11,13,14 (grade 3 or 4) 2% to 17%13,14; vomiting (all grades) 15% to 17%,11,13 (grade 3 or 4) 2%.13
G. Hematologic: Anemia (grade 3 or 4) 2% to 17%,13,14 (all grades) 17% to 50%11,13,14; neutropenia (all grades) 20% to 56%,11,13,14 (grade 3 or 4) 10% to 33%11,13;thrombocytopenia (all grades) 10% to 42%,11,13,14 (grade 3 or 4) 6% to 17%.11,13,14
H. Hepatic: Gamma-glutamyl transpeptidase (GGTP) increased (all grades) 17% to 20%14;increased alkaline phosphatase (all grades) 20% to 50%,11,13,14 (grade 3 or 4) 10%11; increased alanine aminotransferase (ALT) (all grades) 25% to 70%,11, 13,14 (grade 3 or 4) 13% to 40%11,13,14; increased AST (all grades) 20% to 70%,11,13,14 (grade 3 or 4) 8% to 30%11,13; increased ALT/AST (grade 3 or 4) 13%13; increased bilirubin (all grades) 10% to 25%,11,13,14 (grade 3 or 4) 8% to 10%.11
I. Infection: Pneumonia (all grades) 11% to 25%,11,13,14 (grade 3 or 4) 7% to 25%11,13,14; upper respiratory tract infection (all grades) 14% to 40%.11,13,14
J. Pulmonary: Cough (all grades) 8% to 40%,11,13,14 (grade 3 or 4) 10%11; dyspnea (all grades) 18% to 50%,13,14 (grade 3 or 4) 3%.13
K. Renal: Blood urea nitrogen (BUN) increased (all grades) 17% to 20%,14 increased SCr (all grades) 20%.14
DOSAGE MODIFICATIONS
A. Hepatic
1. For ALT/AST elevations greater than 5 to 20 times the upper limit of normal (ULN), stop idelalisib and resume at 100 mg twice daily when ALT/AST levels return to ULN.15
2. For ALT/AST elevations greater than 20 times the ULN, discontinue idelalisib.15
B. Renal
1. No dose adjustment for creatinine clearance greater than or equal to 15 mL/min.15
REFERENCES
- Cashen A, Juckett M, Jumonville A, et al. Phase II study of the histone deacetylase inhibitor belinostat (PXD101) for the treatment of myelodysplastic syndrome (MDS). Ann Hematol. 2012;91(1):33-38.
- Giaccone G, Rajan A, Berman A, et al. Phase II study of belinostat in patients with recurrent or refractory advanced thymic epithelial tumors. J Clin Oncol. 2011;29(15):2052-2059.
- Gimsing P, Hansen M, Knudsen LM, et al. A phase I clinical trial of the histone deacetylase inhibitor belinostat in patients with advanced hematological neoplasia. Eur J Haematol. 2008;81(3):170-176.
- Lassen U, Molife LR, Sorensen M, et al. A phase I study of the safety and pharmacokinetics of the histone deacetylase inhibitor belinostat administered in combination with carboplatin and/or paclitaxel in patients with solid tumours. Br J Cancer. 2010;103(1):12-17.
- Mackay HJ, Hirte H, Colgan T, et al. Phase II trial of the histone deacetylase inhibitor belinostat in women with platinum resistant epithelial ovarian cancer and micropapillary (LMP) ovarian tumours. Eur J Cancer. 2010;46(9):1573-1579.
- Ramalingam SS, Belani CP, Ruel C, et al. Phase II study of belinostat (PXD101), a histone deacetylase inhibitor, for second line therapy of advanced malignant pleural mesothelioma. J Thorac Oncol. 2009;4(1):97-101.
- Steele NL, Plumb JA, Vidal L, et al. A phase 1 pharmacokinetic and pharmacodynamic study of the histone deacetylase inhibitor belinostat in patients with advanced solid tumors. Clin Cancer Res. 2008;14(3):804-810.
- Yeo W, Chung HC, Chan SL, et al. Epigenetic therapy using belinostat for patients with unresectable hepatocellular carcinoma: A multicenter phase I/II study with biomarker and pharmacokinetic analysis of tumors from patients in the Mayo Phase II Consortium and the Cancer Therapeutics Research Group. J Clin Oncol. 2012;30(27):3361-3367.
- Beleodaq [prescribing information]. Irvine, CA: Spectrum Pharmaceuticals, Inc. http://www.beleodaq.com/. Accessed August 14, 2014.
- Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123(22):3390-3397.
- Flinn IW, Kahl BS, Leonard JP, et al. Idelalisib, a selective inhibitor of phosphatidylinositol 3-kinase-δ, as therapy for previously treated indolent non-Hodgkin lymphoma. Blood. 2014;123(22):3406-3413.
- Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med. 2014;370(11):997-1007.
- Gopal AK, Kahl BS, de Vos S, et al. PI3Kδ inhibition by idelalisib in patients with relapsed indolent lymphoma. N Engl J Med. 2014;370(11):1008-1018.
- Kahl BS, Spurgeon SE, Furman RR, et al. A phase 1 study of the PI3Kδ inhibitor idelalisib in patients with relapsed/refractory mantle cell lymphoma (MCL). Blood. 2014;123(22):3398-3405.
- Zydelig [prescribing information]. Foster City, CA: Gilead Sciences, Inc. http://www.gilead.com/~/media/CF1E73FFB80B42E2A39F9F5758DB3001.ashx. Accessed August 14, 2014.

*Dr. Piper is a Pharmacy Practice (PGY1) Resident at Blount Memorial Hospital, Maryville, Tennessee.