Anesthetic Challenges in Robotic-assisted Urologic Surgery
Richard L. Hsu, MD,1 Alan D. Kaye, MD, PhD,2 Richard D. Urman, MD, MBA1
1Department of Anesthesia, Harvard Medical School, Brigham and Women’s Hospital, Boston MA; 2Department of Anesthesia, Louisiana State University, New Orleans, LA
Robotic-assisted surgery has evolved over the past two decades with constantly improving technology, assisting surgeons in multiple subspecialty disciplines. The surgical requirements of lithotomy and steep Trendelenburg positions, along with the creation of a pneumoperitoneum and limited access to the patient, all present anesthetic management challenges in urologic surgery. Patient positioning requirements can cause significant physiologic effects and may result in many complications. Good communication among team members and knowledge of the nuances of robotic surgery have the potential to improve patient outcomes, increase efficiency, and reduce surgical and anesthetic complications.
[ Rev Urol. 2013;15(4):178-184 doi: 10.3909/riu0589]
© 2014 MedReviews®, LLC
Key words
Robotic surgery • Urologic surgery • Anesthesia complications • Pneumoperitoneum • Peripheral nerve injury • Patient positioning
Patient positioning is the most critical part of any robotic-assisted surgery. Without proper patient positioning and port placement, robotic-assisted procedures are tedious to perform and the patient outcomes are compromised.
A multimodal approach to pain management has been shown to decrease length of stay and improve patient satisfaction. This includes epidural analgesia, which has been shown to be superior to patient-controlled local anesthetics in the management of postoperative pain.
The mere availability of robotic surgical capability cannot by itself guarantee a successful surgical program. Teamwork is essential for successful patient outcomes. The anesthesiologist must be ready to deal with the consequences of the steep learning curve, stressed surgeons, and the long duration of most procedures. .
The mere availability of robotic surgical capability cannot by itself guarantee a successful surgical program. Teamwork is essential for successful patient outcomes. The anesthesiologist must be ready to deal with the consequences of the steep learning curve, stressed surgeons, and the long duration of most procedures.
Main Points
• In two short decades, robotic surgery has grown into its own subspecialty. As with other procedures, urologic robotic-assisted procedures are associated with potentially serious complications as a result of steep Trendelenburg positioning, creation of pneumoperitoneum, and difficult access to the patient.
• Patient positioning is the most critical part of any robotic-assisted surgery. Without proper patient positioning and port placement, robotic-assisted procedures are tedious to perform and the patient outcomes are compromised. Obtaining the proper patient position is a dynamic process that requires the supervision of the surgeon.
• Use of robotic systems may increase the overall operating time—and, in turn, the anesthetic exposure time—for cases that have been traditionally performed under laparoscopy or laparotomy. Common complications include positioning injuries, upper body edema, cardiopulmonary compromise, subcutaneous emphysema, and hypothermia.
• A multimodal approach to pain management has been shown to decrease length of stay and improve patient satisfaction. This includes epidural analgesia, which has been shown to be superior to patient-controlled local anesthetics in the management of postoperative pain.
With recent advancements in surgical procedures, there is a greater emphasis on minimally invasive techniques with the goal of improving patient outcomes and satisfaction while decreasing surgical morbidity and mortality. Robotic-assisted surgery, the latest innovation in the field of minimally invasive surgeries, first came into medical practice in 1999.1 The basic principle behind this technology is that the robot “teleports” the surgeon to the operating site and enables operation on the patient from an ergonomic console using three-dimensional vision and autonomous control of wristed laparoscopic surgical instruments.2,3
There are numerous advantages to robotic-assisted surgery, such as improved precision and enhanced accuracy of the movements that can potentially improve patient outcomes.4,5 In particular, the advent of laparoscopic surgery in the late 1980s also highlighted certain limitations, such as loss of typical three-dimensional vision, reduced surgeon coordination, and greatly limited touch.1 The use of robotic technology overcame many of these new obstacles as technology improved over the years.6 The da Vinci® system (Intuitive Surgical, Sunnyvale, CA) mimics a human wrist and includes three distinct pieces: (1) a console; (2) a surgical cart with four arms that represent a surgeon’s left and right arms, an arm to hold and position the endoscope, and a fourth arm to perform other tasks; and (3) an optical three-dimensional tower that provides stereoscopic vision and runs software.1
Since the late 1990s, surgeons have performed a variety of robot-assisted surgical procedures, including cardiac, thoracic, general surgical, gynecologic, and urologic procedures.1 Since then, robotic-assisted techniques are being increasingly used for various urologic procedures, including prostatectomy, partial and total nephrectomy, and microsurgical procedures.7-9 Both the number and variety of urologic procedures performed with robotic assistance have increased significantly, with tens of thousands of cases performed per year in the United States alone.
This review specifically focuses on anesthetic considerations related to urologic surgery with robotic technology. The surgical requirements of the steep Trendelenburg position, along with creation of a pneumoperitoneum and limited physical access to the patient, present anesthetic management challenges in urologic surgery.
Robotic-assisted Urologic Surgery
Robotic-assisted surgeries are gaining popularity in urologic surgery due to the possibility of manipulation through the natural orifices. Wrist-like movements of a robot permit the surgeon to perform with accuracy at the surgical site from a distance. The robotic technique is thus most suitable for operations in a closed and confined space, similar to that of the pelvis.10
Compared with the conventional laparoscopy, robotic-assisted urologic surgeries help perform complicated procedures with ease such as radical cystectomies, prostatectomies, and pelvic lymphadenectomies.10,11 Active areas of research and development in robotic-assisted surgery include the fields of urologic oncology and laparoendoscopic single-site surgery.12,13 Studied outcome benefits of robotic surgery as compared with conventional laparoscopy have shown fewer conversions to laparotomy, likely owing to the technical difficulty of conventional laparoscopy, shorter length of hospitalization, and fewer blood transfusions required, particularly when compared with open laparotomy.10 Intra- and short-term perioperative results have been well described and studied in the literature for major urologic procedures, particularly prostatectomies and nephrectomies.4,14,15 Most important to the future of robotic-assisted urologic surgery is the oncologic outcome in the long term compared with that of conventional laparoscopy and laparotomy; these data are still being collected and analyzed.5,11
Central Issues for the Anesthesiologist
The anesthesiologist must be prepared to handle new challenges associated with proper patient selection and screening, as well as intraoperative care challenges.16,17
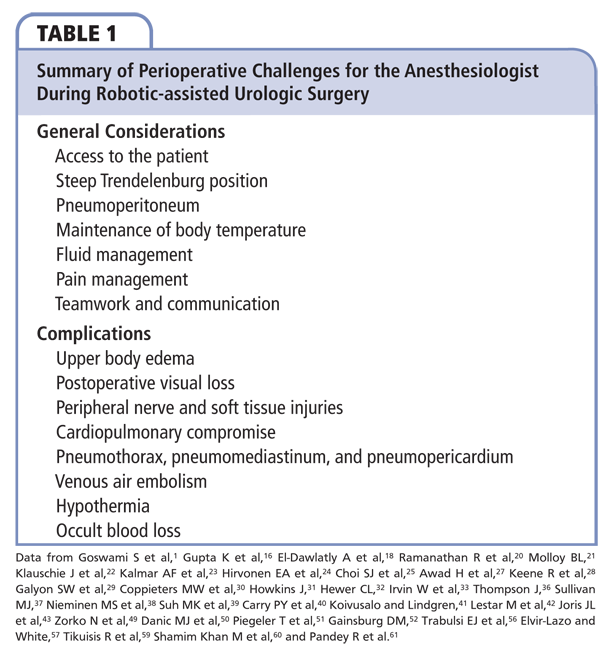
Critical issues for the anesthesiologist during the robotic procedure include steep Trendelenburg position, physiologic consequences of pneumoperitoneum and patient positioning, hypothermia, restricted access to the patient, venous gas embolism, and subcutaneous emphysema. Some of the physiologic changes and complications associated with robotic surgery are outlined in Table 1.
Patient Access
Immediately evident to any anesthesiologist involved with a robotic-assisted surgery is the amount of equipment and setup in the operating room. The robotic surgical system commonly consists of a master/surgeon console, the robotic surgical manipulator, and a computerized visualization tower. The operating room itself must be large enough not only to accommodate all the equipment and personnel involved, but also to provide adequate space for movement and storage of these components. Ensuring ready and adequate access to the patient becomes the anesthesiologist’s primary concern.18 The operating room table itself may be placed farther away from the anesthesia delivery machine to accommodate the robotic surgical manipulator, a bedside surgeon, and the assisting surgical technician next to the patient. Some cases may require that the table be turned 90°, further complicating adequate patient and/or airway access. Paradoxically, the amount of equipment and personnel in the operating room may serve to impinge upon the anesthesiologist’s workspace. As stated earlier, the operating room ideally should be large enough such that these concerns are minimized.
This matter of space in the room is particularly important in the event that emergency access to the patient is required. Cardiopulmonary resuscitation would be difficult, if not impossible, with the robot engaged. Once the robotic surgical manipulator is engaged, the position of the operating table cannot be adjusted unless the robot is disengaged and removed. Removal of the robot is a multistep process that, if done correctly, can be completed in no more than 1 minute. Surgical instruments and the camera are disengaged from the robot arms, the arms are unlatched from the trocars, and the entire robot apparatus is then backed away from the operating table.19
For these reasons, the anesthesiologist must exercise meticulous care when preparing the patient for robotic-assisted surgery. Access to the airway is not guaranteed to be immediate should an event occur, particularly if the robot is positioned over or near the head or upper body. The arms and body of the robot, despite working in the pelvic or abdominal areas, take up a large amount of physical space that can hinder or even interfere with an anesthesiologist’s duties. The endotracheal tube must be secured firmly due to the proximity of moving robot parts and the positioning of the patient. Light foam padding is frequently placed on and around the face to ensure that the robot, surgical devices, or any assistants near the surgical field do not come into contact with the endotracheal tube. It also helps prevent undue accidental pressure on the neck and face of the patient. Some institutions have found that foam padding also provides the benefit of encouraging surgeons to raise the robot arms away from the face; even if the robot arms come into contact, the padding provides enough force feedback that the operating surgeon would be able to move the arm away before any injury is caused.19 This padding, however, must be able to be removed quickly in case of an airway emergency, and thus should not be tightly secured to the patient.
Given the aforementioned concerns, additional intravenous (IV) access is often obtained after anesthetic induction and before—or even during—surgical setup. This is a relatively low-risk way to allow the anesthesiologist an additional avenue for the administration of medications and fluids. Surgeons vary in their preferences for whether both the patient’s arms are tucked or if one is secured to an arm-board and freely accessible to the anesthesiologist. Bilateral peripheral IV access is generally advised. Regardless, early IV access is highly recommended, especially before the robot is engaged and the surgery is underway. These additional IV catheters and arterial lines (if necessary and indicated) should be padded at pressure points and double-checked for adequate length, the absence of kinks or potential obstructions, and properly organized arrangement.
Patient Positioning
Patient positioning is the most critical part of any robotic-assisted surgery. Without proper patient positioning and port placement, robotic-assisted procedures are tedious to perform and the patient outcomes are compromised.20 As stated before, the patient cannot be moved to any other position during the entire robotic part of the procedure. Obtaining the proper patient position is a dynamic process that requires the supervision of the surgeon. Not only should the patient be protected from injuries, but the optimal position must allow for safe docking of the robot as well as access for the bedside surgeon to the surgical assistant ports.21
A steep Trendelenburg position is used so as to provide the optimal exposure of the pelvis and the lower abdomen.22 Placing the patient in this position for extended periods can lead to significant physiologic consequences. The downward movement of the diaphragm by abdominal contents and pneumoperitoneum can decrease pulmonary compliance, functional residual capacity, cause pulmonary edema, and exacerbate ventilation/perfusion mismatch.23-25 These effects may further complicate clinical management of patients with underlying chronic lung disease or the morbidly obese. By pushing the trachea cephalad, the Trendelenburg position can lead to displacement of the endotracheal tube by pushing it further in, resulting in mainstem intubation.26
Steep inclination, ranging from 25° to 45° for a prolonged period of time, can lead to upper airway and brain edema.1 It can also lead to an increase in the intracranial pressure and the cerebral blood flow. For the preservation of cerebrovascular homeostasis, maintenance of normocarbia is recommended. Previous studies have also shown that the steep Trendelenburg position for long hours during gynecologic procedures has led to postoperative vision loss.27 Also, facial engorgement and edema are quite substantial. These physiologic changes led Molloy21 to hypothesize that, under anesthesia in a steep Trendelenburg position, cerebrovascular and ophthalmic circulatory autoregulation do not prevent increases in intraocular pressure (IOP) and decreases in ocular perfusion pressure, which is mean arterial pressure minus IOP. This study showed that, even under anesthesia, the cerebrovascular and ophthalmic circulatory autoregulation do not prevent complications such as increased IOP.21
Shifting of the patient’s trunk is an important concern in that it often leads to suboptimal positioning of the extremities, increasing the risk of nerve injury from stretch and compression. Gluteal and lower extremity acute compartment syndrome requiring fasciotomy, and rhabdomyolysis resulting in renal failure as a result of prolonged intraoperative dorsal lithotomy position have been reported.28,29
Different groups around the world have suggested methods to prevent patient shifting during the steep Trendelenburg position, including braces, leg suspension, and iliac supports. But all of these may potentially result in nerve injury.30-33Also, the shoulder braces and straps that are used to prevent the patient from shifting cause neuropathic injury.34 During the robotic-assisted urologic surgeries, the trocars and instruments are fixed, and so the prevention of patient sliding becomes all the more important. The risk of stretching and tearing of the incisions, which may in turn increase the risk of an incisional hernia, is of concern. Klauschie and colleagues22 demonstrated for the first time the use of an anti-skid foam material for patient positioning. Although they observed small shifts, no clinical neurologic injuries were noted. Because any intraoperative movement can be catastrophic, muscle relaxation is critical for success.
In summary, the systems most vulnerable to the head-down extreme position are the cardiac, respiratory, and central nervous systems.35,36 Other complications include unrecognized surgical injury, occult blood loss, and risk of hypothermia.1,37
Pneumoperitoneum
The presence of air within the peritoneal cavity results in pneumoperitoneum. Generally, intraperitoneal insufflation with CO2 is performed in patients in the Trendelenburg position when the patient is at 15° to 20°. Lung compliance can decrease by more than 50%, and mean pulmonary arterial pressure and pulmonary capillary wedge pressure also decrease.38 In addition, there is an increase in peak inspiratory pressure, plateau pressure, and end-tidal carbon dioxide tension.39 The CO2 insufflation can result in increased postoperative complications in patients with underlying lung disease. For example, patients with conditions such as chronic obstructive pulmonary disease are less efficient in eliminating excessive CO2 even with increased minute volume of ventilation, leading to postoperative respiratory hypercarbia and acidosis requiring prolonged mechanical ventilation.40,41
The combination of the steep Trendelenburg position with pneumoperitoneum influences cardiopulmonary physiology in many ways.34 Pneumoperitoneum and 45° Trendelenburg position have been shown to cause two- to threefold increases in left ventricular filling pressures,42 and cardiac output may decrease.43 There is also an increase in the systemic vascular resistance and the mean arterial pressure, whereas the renal, splanchnic, and the portal flow decrease. There is activation of the renin-angiotensin system, thus increasing the levels of vasopressin.
Cardiopulmonary Effects and Complications
As discussed previously, combination of a pneumoperitoneum and steep Trendelenburg positioning causes pulmonary problems such as atelectasis and ventilation/perfusion mismatch.1 A decrease in the pulmonary compliance and functional residual capacity is observed, but the peak airway pressures increase. White and Eng44 demonstrated how subcutaneous emphysema occurs frequently with the steep Trendelenburg position, and this may contribute significantly to the total amount of CO2 absorbed in addition to the absorption of peritoneal CO2 insufflation. Ideally, hyperventilation is the solution to the hypercarbia and respiratory acidosis, but during the steep Trendelenburg position the hyperventilation is limited during robotic surgery by a higher ventilator inspired pressure. Plus, the abdominal CO2 insufflation also limits diaphragmatic excursion.25 For this setting, Oğurlu and associates observed lower peak airway pressure and plateau pressure with higher lung compliance with the use of pressure-controlled ventilation.45 This use of pressure-controlled ventilation allowing a larger tidal volume for the same inspired pressure might be particularly useful for patients who are more difficult to ventilate.46
Positive end-expiratory pressure (PEEP) can help decrease atelectasis. It has been known to improve intraoperative oxygenation and lung mechanics. PEEP impedes the venous blood return from the lower extremities and decreases cardiac output, but this effect is likely to be negated by the extreme Trendelenburg position. It is, therefore, suggested to limit the amount of CO2 insufflation causing increase venous congestion in the upper extremity, to avoid facial and airway edema.47
With creation of pneumoperitoneum, immediate gas embolism may occur and, in very rare cases, it can cause severe cardiovascular failure and death. It is presumed to occur from rapid insufflation of gas directly into the bloodstream.18 Certain measures to avoid and treat this complication include rapid removal of pneumoperitoneum, hyperventilation with oxygen, placing the patient in the left lateral decubitus and Trendelenburg positions, and potentially aspirating the embolus via a central venous catheter.18,48 During the procedure, CO2 should preferably be the gas used for insufflation (because of its high diffusion coefficient), thereby minimizing the risk of gas emboli.49 Measuring the CO2 levels at the end of exhalation allows the anesthesiologist to adjust the ventilator to remove excess CO2, to help prevent hypercarbia and acidosis. It is this time that needs extreme caution at the anesthesiologist’s end.
Fluid Management
Relatively long surgical times, steep Trendelenburg positioning, and pneumoperitoneum can make fluid management a complex issue. Complicating this matter is the fact that excessive urine output might obscure the operative field, as is the case in vesicourethral anastamosis.50,51 Facial, pharyngeal, and laryngeal edema may be worsened with prolonged steep Trendelenburg positioning and result in postextubation respiratory distress with the concern that the patient may require reintubation. For these reasons, some institutions have recommended keeping pre- and intraoperative fluids to a minimum, often, 2 L of crystalloid.27,50-52 However, the anesthesiologist must also be mindful of the postoperative effects of a restrictive intraoperative fluid management strategy. Even in conventional laparoscopic surgeries, renal plasma flow and glomerular filtration rate decrease concomitantly with urine output.53,54 Resultant postoperative oliguria has been noted in both laparoscopic and robot-assisted surgeries.3 The relative volume depletion of such patients postoperatively often requires fluid boluses to support not only urine output but also maintenance of normal hemodynamic parameters. Thus, a carefully designed fluid management strategy must include the postoperative period to ensure appropriate renal function and volume status for urologic patients.
Pain Management and Other Complications
Another major anesthetic consideration during robotic-assisted urologic surgeries is the prolonged anesthesia, which serves to accentuate the problems highlighted above by placing a longer challenge to the patient’s cardiorespiratory capacity.55 Regarding pain management, robot-assisted surgeries may be similar to conventional laparoscopy in that smaller incisions create less incisional pain for the patient, but deep pelvic pain from the surgery itself remains an issue. A multimodal approach to pain management has been shown to decrease length of stay and improve patient satisfaction.56,57 This includes epidural analgesia, which has been shown to be superior to patient-controlled local anesthetics in the management of postoperative pain.58 There are also other benefits to using epidural analgesia in addition to general anesthesia for urologic cancer surgeries, including reduced intraoperative blood loss and reduced need for blood transfusions, and so the anesthesiologist involved in the care of such patients needs to use clinical judgment and discretion to formulate an appropriate and tailored anesthetic plan.59
Teamwork and Communication
The mere availability of robotic surgical capability cannot by itself guarantee a successful surgical program. Teamwork is essential for successful patient outcomes. The anesthesiologist must be ready to deal with the consequences of the steep learning curve, stressed surgeons, and the long duration of most procedures. Given all of the technologic aspects of robotic surgery and the potential physiological consequences and risk of morbidity and mortality specific to urologic surgeries, the use of robotic surgery simulation programs may afford distinct advantages when preparing personnel for success in the operating room. Simulation has the potential to improve outcomes and reduce complications while enhancing teamwork.60 In addition, good communication among all members of the team, including surgeons, anesthesiologists, and nurses, is key to a safe, effective, and efficient environment. The addition of audio speakers to transmit the surgeon’s voice can also improve communication among team members.61
Conclusions
In two short decades, robotic surgery has grown into its own subspecialty. As with other procedures, urologic robotic-assisted procedures are associated with potentially serious complications as a result of steep Trendelenburg positioning, creation of pneumoperitoneum, and difficult access to the patient. In addition, the use of robotic systems may increase the overall operating time—and, in turn, the anesthetic exposure time—for cases that have been traditionally performed under laparoscopy or laparotomy. Common complications include positioning injuries, upper body edema, cardiopulmonary compromise, subcutaneous emphysema, and hypothermia. Teamwork and communication among surgeons, nurses, and anesthesiologists are essential to minimize complications, and improve surgical conditions and patient outcomes. ![]()
References
- Goswami S, Nishanian E, Mets B. Anesthesia for robotic surgery. In: Miller RD, ed. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Elsevier; 2010:1103, 2389-2395.
- Mendivil A, Holloway RW, Boggess JF. Emergence of robotic assisted surgery in gynecologic oncology: American perspective. Gynecol Oncol. 2009;114(suppl 2):S24-S31.
- Baltayian S. A brief review: anesthesia for robotic surgery. J Robotic Surg.2008;2:59-66.
- Aron M, Koenig P, Kaouk JH, et al. Robotic and laparoscopic partial nephrectomy: a matched-pair comparison from a high-volume centre. BJU Int. 2008;102:86-92.
- Novara G, Ficarra V. Robotic-assisted laparoscopic radical cystectomy: where do we stand? Int J Clin Pract. 2009;63:185-188.
- Tan SJ, Lin CK, Fu PT, et al. Robotic surgery in complicated gynecologic diseases: experience of Tri-Service General Hospital in Taiwan. Taiwanese J Obstet Gynecol. 2012;51:18-25.
- Schiff J, Li PS, Goldstein M. Robotic microsurgical vasovasostomy and vasoepididymostomy: a prospective randomized study in a rat model. J Urol. 2004;171:1720-1725.
- Fleming C. Robot-assisted vasovasostomy. Urol Clin North Am. 2004;31:769-772.
- Parekattil SJ, Cohen MS. Robotic surgery in male infertility and chronic orchialgia. Curr Opin Urol. 2010;20:75-79.
- Ontario Ministry of Health. Robotic-assisted minimally invasive surgery for gynecologic and urologic oncology: an evidence-based analysis. Ontario Health Technology Assessment Series. 2010;10:1-118.
- Challacombe BJ, Bochner BH, Dasgupta P, et al. The role of laparoscopic and robotic cystectomy in the management of muscle-invasive bladder cancer with special emphasis on cancer control and complications. Eur Urol. 2011;60:767-775.
- Tiu A, Kim KH, Shin TY, et al. Feasibility of robotic laparoendoscopic single-site partial nephrectomy for renal tumors >4 cm. Eur Urol. 2013;63:941-946.
- Autorino R, Kaouk JH, Stolzenburg JU, et al. Current status and future directions of robotic single-site surgery: a systematic review. Eur Urol. 2013;63:266-280.
- Haber GP, Crouzet S, Gill IS. Laparoscopic and robotic assisted radical cystectomy for bladder cancer: a critical analysis. Eur Urol. 2008;54:54-62.
- Rassweiler J, Hruza M, Teber D, Su LM. Laparoscopic and robotic assisted radical prostatectomy—critical analysis of the results. Eur Urol. 2006;49:612-624.
- Gupta K, Mehta Y, Sarin Jolly A, Khanna S. Anaesthesia for robotic gynaecological surgery. Anaesth Intensive Care. 2012;40:614-621.
- Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004;239:14-21.
- El-Dawlatly A, Khairy G, Al-Dohayan A, et al. Anesthetic considerations with telemanipulative robotic-assisted laparoscopic cholecystectomy using the Da Vinci System. Internet J Anaesthesiol. 2004;8:2-5.
- Parr KG, Talamini MA. Anesthetic implications of the addition of an operative robot for endoscopic surgery: a case report. J Clin Anesth. 2002;14:228-233.
- Ramanathan R, Carey RI, Lopez-Pujals A, Leveillee RJ. Patient positioning and trocar placement for robotic urologic procedures. In: Patel VR, ed. Robotic Urologic Surgery. 2nd ed. London, UK: Springer-Verlag; 2012:107-120.
- Molloy BL. Implications for postoperative visual loss: steep Trendelenburg position and effects on intraocular pressure. AANA J. 2011;79:115-121.
- Klauschie J, Wechter ME, Jacob K, et al. Use of anti-skid material and patient-positioning to prevent patient shifting during robotic-assisted gynecologic procedures. J Minim Invasive Gynecol. 2010;17:504-507.
- Kalmar AF, Foubert L, Hendrickx JF, et al. Influence of steep Trendelenburg position and CO(2) pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104:433-439.
- Hirvonen EA, Nuutinen LS, Kauko M. Hemodynamic changes due to Trendelenburg positioning and pneumoperitoneum during laparoscopic hysterectomy. Acta Anaesthesiol Scand. 1995;39:949-955.
- Choi SJ, Gwak MS, Ko JS, et al. The effects of the exaggerated lithotomy position for radical perineal prostatectomy on respiratory mechanics. Anaesthesia. 2006;61:439-443.
- Chang CH, Lee HK, Nam SH. The displacement of the tracheal tube during robot-assisted radical prostatectomy. Eur J Anaesthesiol. 2010;27:478-480.
- Awad H, Santilli S, Ohr M, et al. The effects of steep Trendelenburg positioning on intraocular pressure during robotic radical prostatectomy. Anesth Analg. 2009;109:473-478.
- Keene R, Froelich JM, Milbrandt JC, Idusuyi OB. Bilateral gluteal compartment syndrome following robotic-assisted prostatectomy. Orthopedics. 2010;33:852.
- Galyon SW, Richards KA, Pettus JA, Bodin SG. Three-limb compartment syndrome and rhabdomyolysis after robotic cystoprostatectomy. J Clin Anesth. 2011;23:75-78.
- Coppieters MW, Van de Velde M, Stappaerts KH. Positioning in anesthesiology: toward a better understanding of stretch-induced perioperative neuropathies. Anesthesiology. 2002;97:75-81.
- Howkins J. The Trendelenburg position. Lancet. 1952;2:759-760.
- Hewer CL. Maintenance of the Trendelenburg position by skin friction. Lancet. 1953;1:522-524.
- Irvin W, Andersen W, Taylor P, Rice L. Minimizing the risk of neurologic injury in gynecologic surgery. Obstet Gynecol. 2004;103:374-382.
- Barnett JC, Hurd WW, Rogers RM Jr, et al. Laparoscopic positioning and nerve injuries. J Minim Invasive Gynecol. 2007;14:664-672; quiz 73.
- Sener A, Chew BH, Duvdevani M, et al. Combined transurethral and laparoscopic partial cystectomy and robot-assisted bladder repair for the treatment of bladder endometrioma. J Minim Invasive Gynecol. 2006;13:245-248.
- Thompson J. Myocardial infarction and subsequent death in a patient undergoing robotic prostatectomy. AANA J. 2009;77:365-371.
- Sullivan MJ, Frost EA, Lew MW. Anesthetic care of the patient for robotic surgery. Middle East J Anesthesiol. 2008;19:967-982.
- Nieminen MS, Böhm M, Cowie MR, et al. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26:384-416.
- Suh MK, Seong KW, Jung SH, Kim SS. The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol. 2010;59:329-334.
- Carry PY, Gallet D, François Y, et al. Respiratory mechanics during laparoscopic cholecystectomy: the effects of the abdominal wall lift. Anesth Analg. 1998;87:1393-1397.
- Koivusalo AM, Lindgren L. Respiratory mechanics during laparoscopic cholecystectomy. Anesth Analg.1999;89:800.
- Lestar M, Gunnarsson L, Lagerstrand L, et al. Hemodynamic perturbations during robot-assisted laparoscopic radical prostatectomy in 45 degrees Trendelenburg position. Anesth Analg. 2011;113:1069-1075.
- Joris JL, Noirot DP, Legrand MJ, et al. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067-1071.
- White PF, Eng MR. Ambulatory (outpatient) anesthesia. In: Miller RD, ed. Miller’s Anesthesia. 6th ed. Philadelphia, PA: Churchill Livingstone; 2005:2288-2290.
- Oğurlu M, Küçük M, Bilgin F, et al. Pressure-controlled vs volume-controlled ventilation during laparoscopic gynecologic surgery. J Minim Invasive Gynecol. 2010;17:295-300.
- Stolzenburg JU, Aedtner B, Olthoff D, et al. Anaesthetic considerations for endoscopic extraperitoneal and laparoscopic transperitoneal radical prostatectomy. BJU Int. 2006;98:508-513.
- Weingarten TN, Whalen FX, Warner DO, et al. Comparison of two ventilatory strategies in elderly patients undergoing major abdominal surgery. Br J Anaesth. 2010;104:16-22.
- Sprung J, Whalley DG, Falcone T, et al. The impact of morbid obesity, pneumoperitoneum, and posture on respiratory system mechanics and oxygenation during laparoscopy. Anesthes Analg. 2002;94:1345-1350.
- Zorko N, Mekiš D, Kamenik M. The influence of the Trendelenburg position on haemodynamics: comparison of anaesthetized patients with ischaemic heart disease and healthy volunteers. J Intern Med Res. 2011;39:1084-1089.
- Danic MJ, Chow M, Alexander G, et al. Anesthesia considerations for robotic-assisted laparoscopic prostatectomy: a review of 1,500 cases. J Robotic Surg. 2007;1:119-123.
- Piegeler T, Dreessen P, Schläpfer M, et al. Impact of intraoperative fluid management on outcome in patients undergoing robotic-assisted laparoscopic prostatectomy—a retrospective analysis. Eur J Anaesth. 2011;28:81. Abstract 6AP1-6.
- Gainsburg DM. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012;78:596-604.
- Iwase K, Takenaka H, Ishizaka T, et al. Serial changes in renal function during laparoscopic cholecystectomy. Eur Surg Res. 1993;25:203-212.
- Chiu AW, Azadzoi KM, Hatzichristou DG, et al. Effects of intra-abdominal pressure on renal tissue perfusion during laparoscopy. J Endourol. 1994;8:99-103.
- Bird VG, Winfield HN. Laparoscopy in urology. In: Fallon B, ed. Hospital Physician, Urology Board Review. Wayne, PA: Turner White Communications, Inc.; 2002.
- Trabulsi EJ, Patel J, Viscusi ER, et al. Preemptive multimodal pain regimen reduces opioid analgesia for patients undergoing robotic-assisted laparoscopic radical prostatectomy. Urology. 2010;76:1122-1124.
- Elvir-Lazo OL, White PF. The role of multimodal analgesia in pain management after ambulatory surgery. Current Opin Anaesthesiol. 2010;23:697-703.
- Fant F, Axelsson K, Sandblom D, et al. Thoracic epidural analgesia or patient-controlled local analgesia for radical retropubic prostatectomy: a randomized, double-blind study. Br J Anaesth. 2011;107:782-789.
- Tikuisis R, Miliauskas P, Samalavicius NE, et al. Epidural and general anesthesia versus general anesthesia in radical prostatectomy. Medicina (Kaunas). 2009;45:772-777.
- Shamim Khan M, Ahmed K, Gavazzi A, et al. Development and implementation of centralized simulation training: evaluation of feasibility, acceptability and construct validity. BJU Int. 2013;111:518-523.
- Pandey R, Garg R, Darlong V, et al. Hemiparesis after robotic laparoscopic radical cystectomy and ileal conduit formation in steep Trendelenburg position. J Robotic Surg. 2012;6:269-271.