Adenomatoid Tumor of the Testis Arising From the Tunica Albuginea
Andrew Y. Sun, MD, A. Scott Polackwich, MD, Edmund S. Sabanegh, Jr, MD
Department of Urology, Glickman Urologic and Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH
Adenomatoid tumors are the most common paratesticular tumor. Although they primarily arise from the epididymis, they can rarely occur as an isolated intratesticular mass. These tumors are benign and surgical excision is curative. We present a case of a 36-year-old man diagnosed with an intratesticular adenomatoid tumor.
[Rev Urol. 2016;18(1):51-53 doi: 10.3909.riu0690]
© 2016 MedReviews®, LLC
Adenomatoid Tumor of the Testis Arising From the Tunica Albuginea
Andrew Y. Sun, MD, A. Scott Polackwich, MD, Edmund S. Sabanegh, Jr, MD
Department of Urology, Glickman Urologic and Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH
Adenomatoid tumors are the most common paratesticular tumor. Although they primarily arise from the epididymis, they can rarely occur as an isolated intratesticular mass. These tumors are benign and surgical excision is curative. We present a case of a 36-year-old man diagnosed with an intratesticular adenomatoid tumor.
[Rev Urol. 2016;18(1):51-53 doi: 10.3909.riu0690]
© 2016 MedReviews®, LLC
Adenomatoid Tumor of the Testis Arising From the Tunica Albuginea
Andrew Y. Sun, MD, A. Scott Polackwich, MD, Edmund S. Sabanegh, Jr, MD
Department of Urology, Glickman Urologic and Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH
Adenomatoid tumors are the most common paratesticular tumor. Although they primarily arise from the epididymis, they can rarely occur as an isolated intratesticular mass. These tumors are benign and surgical excision is curative. We present a case of a 36-year-old man diagnosed with an intratesticular adenomatoid tumor.
[Rev Urol. 2016;18(1):51-53 doi: 10.3909.riu0690]
© 2016 MedReviews®, LLC
Key words
Testicular neoplasm • Adenomatoid tumor
Key words
Testicular neoplasm • Adenomatoid tumor
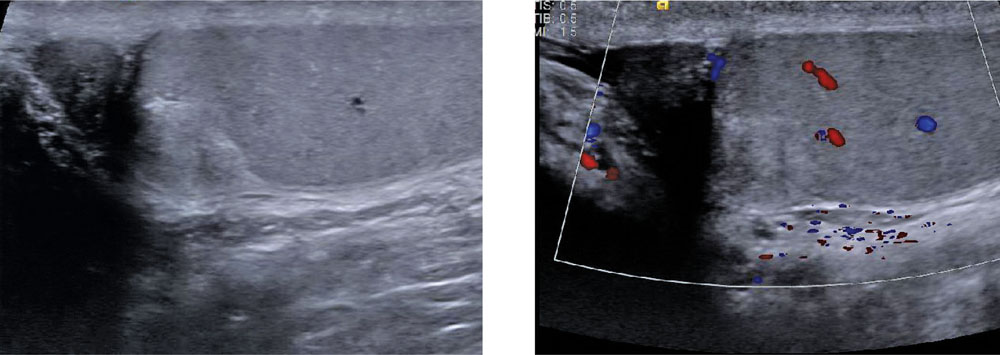
Figure 1. Scrotal ultrasound. Sagittal image of the left testis shows a 1.0 × 0.9 × 0.9 cm superior pole heterogeneous mass. Color Doppler demonstrates no vascular flow within this area.
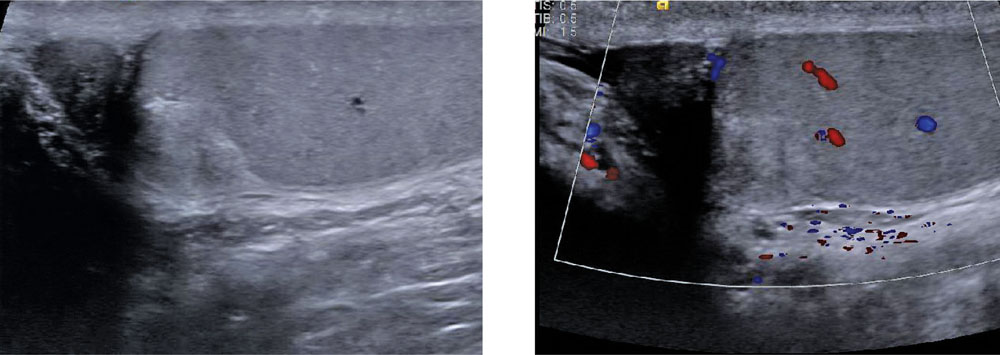
Figure 1. Scrotal ultrasound. Sagittal image of the left testis shows a 1.0 × 0.9 × 0.9 cm superior pole heterogeneous mass. Color Doppler demonstrates no vascular flow within this area.
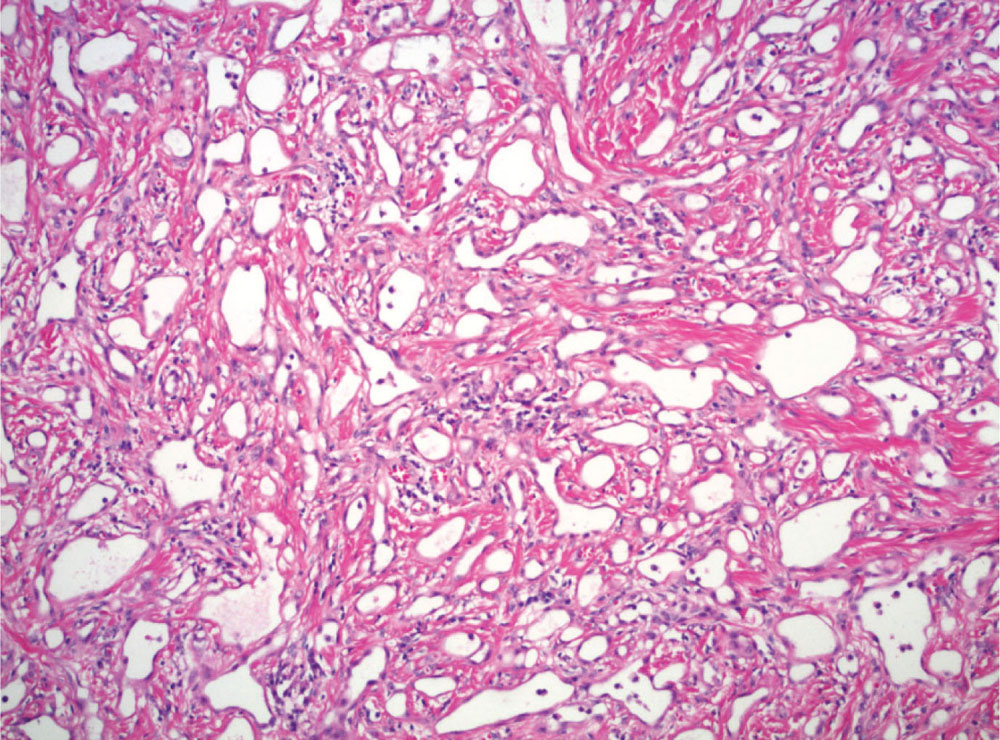
Figure 2. Pathology specimen. Adenomatoid tumor showing characteristic cells with pink cytoplasm, eccentric nuclei, vacuolization, and intervening hyalinization of stroma.
… there are no ultrasound features that can definitively differentiate an adenomatoid tumor from malignant testicular masses.
There has been some controversy regarding the histogenesis of these tumors, but recent evidence has supported a mesothelial origin.
Main Points
• Adenomatoid tumors are rare, benign tumors primarily found in the male and female genital tract. In men, they are the most frequent paratesticular tumor, accounting for approximately 30% of all paratesticular masses.
• Ultrasonography usually shows a well-defined and homogeneous mass of between 0.5 and 1.5 cm in size. Ultrasound can be useful in distinguishing a paratesticular mass from an intratesticular mass.
• Histology usually shows chords and nests of cuboidal cells with low nuclear-to-cytoplasmic ratio, vacuolated cytoplasm, and small nucleoli. There may be fibrous and hyalinized stroma and lymphoid aggregates.
• These tumors are benign and therefore inguinal exploration and surgical excision are both diagnostic and therapeutic, without need for further intervention. When combined with tumor markers, ultrasonography, and intraoperative frozen section analysis, testis-sparing surgery can be considered in the management of these tumors.
Main Points
• Adenomatoid tumors are rare, benign tumors primarily found in the male and female genital tract. In men, they are the most frequent paratesticular tumor, accounting for approximately 30% of all paratesticular masses.
• Ultrasonography usually shows a well-defined and homogeneous mass of between 0.5 and 1.5 cm in size. Ultrasound can be useful in distinguishing a paratesticular mass from an intratesticular mass.
• Histology usually shows chords and nests of cuboidal cells with low nuclear-to-cytoplasmic ratio, vacuolated cytoplasm, and small nucleoli. There may be fibrous and hyalinized stroma and lymphoid aggregates.
• These tumors are benign and therefore inguinal exploration and surgical excision are both diagnostic and therapeutic, without need for further intervention. When combined with tumor markers, ultrasonography, and intraoperative frozen section analysis, testis-sparing surgery can be considered in the management of these tumors.
A 36-year-old man presented with a 7-year history of a slowly growing left testis mass. A scrotal ultrasound was done when he first reported it 7 years ago, but a mass was not seen at that time. Prior to our evaluation, he had been seen for infertility and was found to have azoospermia. He also had a history of bilateral cryptorchidism for which he underwent bilateral orchidopexy as a child, and a childhood ocular tumor for which he underwent prior chemotherapy. There was no personal or family history of testicular cancer. On physical examination, he was a well-nourished, well-masculinized young man without gynecomastia. Testicular examination revealed normal 20 mL volume and consistency bilaterally, with a 1.5-cm firm mass of the left upper testicular pole, adjacent to or possibly involving the left epididymis. Testicular ultrasonography demonstrated a 10 × 9 × 9 mm nonvascular heterogeneous, well-demarcated mass within the left upper testis (Figure 1). The remainder of the ultrasound examination was unremarkable. Serum α fetoprotein and human chorionic gonadotropin levels were normal. Lactate dehydrogenase level was slightly elevated at 272 U/L (range, 100-220 U/L). Treatment options were discussed, including partial orchiectomy with frozen section versus radical orchiectomy. After this discussion the patient elected to undergo left radical orchiectomy. Operative exploration revealed a 1.2 × 1.0 × 0.7 cm white fibrous nodule of the left testis. Pathologic examination revealed that the intratesticular nodule was adjacent to the epididymis and involved the tunica albuginea and abutted the tunica vaginalis. A diagnosis of adenomatoid tumor was made based on histology (Figure 2). The patient also incidentally had Sertoli cell–only syndrome in the remaining testicular parenchyma, explaining his infertility. The postoperative course was unremarkable.
Discussion
Adenomatoid tumors are rare, benign tumors primarily found in the male and female genital tract.1 Rarely they can present in extragenital sites including the heart, pleura, adrenal, intestinal mesentery, and omentum.2,3 In men, they are the most frequent paratesticular tumor, accounting for approximately 30% of all paratesticular masses.3 Although they primarily arise from the epididymis, they can infrequently occur as an intratesticular mass originating from the tunica albuginea.4 Approximately 12 cases have been reported of involvement of the testicular parenchyma and may arise from the rete testis.2,3
Adenomatoid tumors most often present as an incidental finding or as a painless, firm, slow-growing scrotal mass of < 2 cm in diameter. Occasionally patients have presented with testicular pain.5 They can be seen in patients of all ages, though they most commonly present between age 30 and 50.5
Ultrasonography usually shows a well-defined and homogeneous mass of between 0.5 and 1.5 cm in size. Ultrasound can be useful in distinguishing a paratesticular mass from an intratesticular mass. They demonstrate variable flow on Doppler and may be increased, decreased, or normal. Unfortunately, there are no ultrasound features that can definitively differentiate an adenomatoid tumor from malignant testicular masses.6
Histology usually shows chords and nests of cuboidal cells with low nuclear-to-cytoplasmic ratio, vacuolated cytoplasm, and small nucleoli. There may be fibrous and hyalinized stroma and lymphoid aggregates. There has been some controversy regarding the histogenesis of these tumors, but recent evidence has supported a mesothelial origin.3,7 Immunohistochemistry shows positivity for WT1, calretinin, vimentin, and D2-40.3
These tumors are benign and therefore inguinal exploration and surgical excision are both diagnostic and therapeutic, without need for further intervention.8 None have ever been observed to recur or undergo malignant degeneration.1 Given this, it is important to consider these rare, benign tumors in the differential diagnosis of testicular masses. When combined with tumor markers, ultrasonography, and intraoperative frozen section analysis, testis-sparing surgery can be considered in the management of these tumors. ![]()
References
- Schwartz EJ, Longacre TA. Adenomatoid tumors of the female and male genital tracts express WT1. Int J Gynecol Pathol. 2004;23:123-128.
- Wojewoda CM, Wasman JK, MacLennan GT. Adenomatoid tumor of the adrenal gland. J Urol. 2008;180:1123.
- Delahunt B, Eble JN, King D, et al. Immunohistochemical evidence for mesothelial origin of paratesticular adenomatoid tumour. Histopathology. 2000;36:109-115.
- Oyama H, Ogawa M, Mikuriya H, et al. Adenomatoid tumor of testicular tunica albuginea: a case report [in Japanese]. Hinyokika Kiyo. 2001;47:661-663.
- Alam K, Maheshwari V, Varshney M, et al. Adenomatoid tumour of testis. BMJ Case Rep. 2011;2011:bcr0120113790. doi:10.1136/bcr.01.2011.3790.
- Tammela TL, Karttunen TJ, Mäkäräinen HP, et al. Intrascrotal adenomatoid tumors. J Urol. 1991;146:61-65.
- Stephenson TJ, Mills PM. Adenomatoid tumours: an immunohistochemical and ultrastructural appraisal of their histogenesis. J Pathol. 1986;148:327-335.
- Williams SB, Han M, Jones R, Andrawis R. Adenomatoid tumor of the testes. Urology. 2004;63:779-781.