The Evolution of Coronary Revascularization Appropriateness Use Criteria: From Mandatory to Forgotten
Sudhakar Sattur, MD, MHSA,1 Sorin J. Brener, MD2
1Guthrie Clinic, Sayre, PA; 2New York Methodist Hospital, Brooklyn, NY
The appropriateness use criteria (AUC) for coronary revascularization have been formulated through the joint efforts of several professional societies. The goals of AUC were to aid in physician decision making and to objectively define the need and context for revascularization. These criteria, developed using a standardized approach, were widely promoted and adopted in many practices. Rigorous use in daily practice and public reporting of adherence to these criteria has exposed some of their deficiencies. Revisions to the original version were made to accommodate public and physician sentiments. Not surprisingly, the recent percutaneous coronary intervention performance measures developed by the same professional societies that have proposed AUC, have suggested that AUC should be used for internal quality improvement only at this time. Therefore, the present role and future application of AUC to cardiology practice is uncertain. The goals of this review are to describe methodology and development of the coronary revascularization AUC, to focus on the strengths and limitations of AUC, and to identify challenges related to application of these criteria in daily practice.
[ Rev Cardiovasc Med. 2015;16(4):235-243 doi: 10.3909/ricm0783 ]
© 2016 MedReviews®, LLC
The Evolution of Coronary Revascularization Appropriateness Use Criteria: From Mandatory to Forgotten
Sudhakar Sattur, MD, MHSA,1 Sorin J. Brener, MD2
1Guthrie Clinic, Sayre, PA; 2New York Methodist Hospital, Brooklyn, NY
The appropriateness use criteria (AUC) for coronary revascularization have been formulated through the joint efforts of several professional societies. The goals of AUC were to aid in physician decision making and to objectively define the need and context for revascularization. These criteria, developed using a standardized approach, were widely promoted and adopted in many practices. Rigorous use in daily practice and public reporting of adherence to these criteria has exposed some of their deficiencies. Revisions to the original version were made to accommodate public and physician sentiments. Not surprisingly, the recent percutaneous coronary intervention performance measures developed by the same professional societies that have proposed AUC, have suggested that AUC should be used for internal quality improvement only at this time. Therefore, the present role and future application of AUC to cardiology practice is uncertain. The goals of this review are to describe methodology and development of the coronary revascularization AUC, to focus on the strengths and limitations of AUC, and to identify challenges related to application of these criteria in daily practice.
[ Rev Cardiovasc Med. 2015;16(4):235-243 doi: 10.3909/ricm0783 ]
© 2016 MedReviews®, LLC
The Evolution of Coronary Revascularization Appropriateness Use Criteria: From Mandatory to Forgotten
Sudhakar Sattur, MD, MHSA,1 Sorin J. Brener, MD2
1Guthrie Clinic, Sayre, PA; 2New York Methodist Hospital, Brooklyn, NY
The appropriateness use criteria (AUC) for coronary revascularization have been formulated through the joint efforts of several professional societies. The goals of AUC were to aid in physician decision making and to objectively define the need and context for revascularization. These criteria, developed using a standardized approach, were widely promoted and adopted in many practices. Rigorous use in daily practice and public reporting of adherence to these criteria has exposed some of their deficiencies. Revisions to the original version were made to accommodate public and physician sentiments. Not surprisingly, the recent percutaneous coronary intervention performance measures developed by the same professional societies that have proposed AUC, have suggested that AUC should be used for internal quality improvement only at this time. Therefore, the present role and future application of AUC to cardiology practice is uncertain. The goals of this review are to describe methodology and development of the coronary revascularization AUC, to focus on the strengths and limitations of AUC, and to identify challenges related to application of these criteria in daily practice.
[ Rev Cardiovasc Med. 2015;16(4):235-243 doi: 10.3909/ricm0783 ]
© 2016 MedReviews®, LLC
KEY WORDS
Appropriateness use criteria • Coronary revascularization • Percutaneous coronary intervention
KEY WORDS
Appropriateness use criteria • Coronary revascularization • Percutaneous coronary intervention
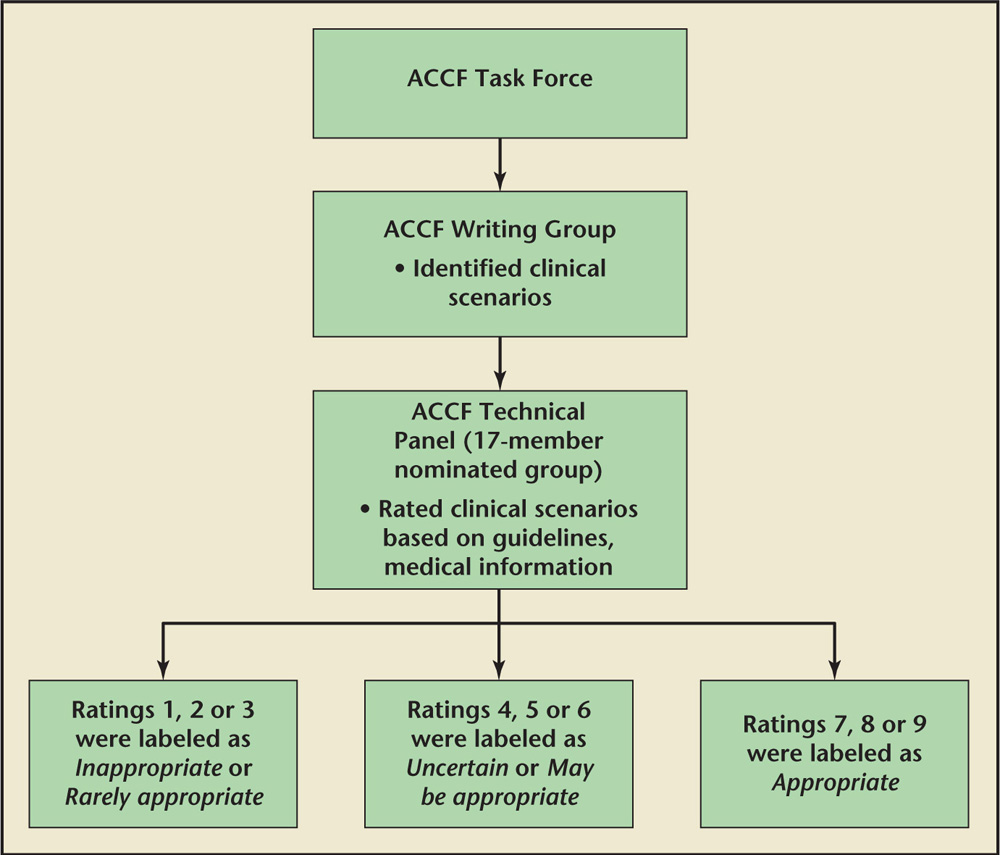
Figure 1. Flow chart describing the process of development of coronary revascularization appropriateness use criteria. ACCF, American College of Cardiology Foundation.
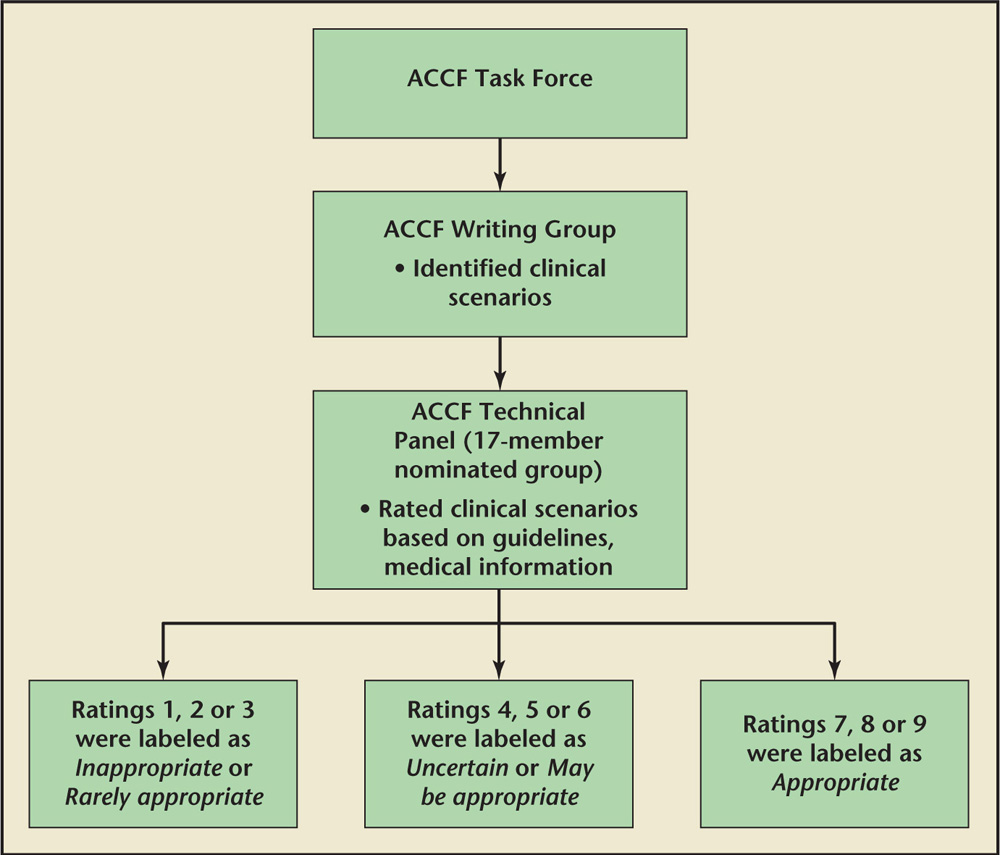
Figure 1. Flow chart describing the process of development of coronary revascularization appropriateness use criteria. ACCF, American College of Cardiology Foundation.
… prior to the introduction of AUC, significant variability in utilization of cardiovascular procedures was noted. There was no objective tool to measure this variability.
Even though the AUC document provides a good definition of the severity of ischemia noted on noninvasive testing, it fails to consider the fact that many cardiologists interpret stress test results without the quantitative assessment required to assign the AUC severity score.
Further analysis of PCIs deemed inappropriate for nonacute indications showed these procedures were more commonly performed in white men with private insurance receiving care in suburban hospitals.
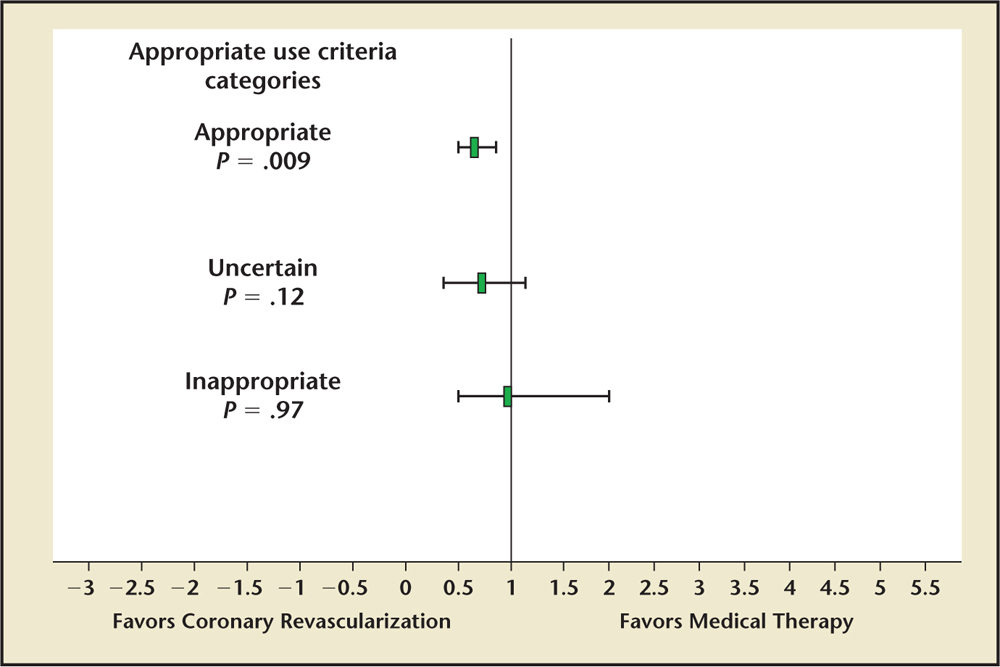
Figure 2. Comparison of 3-year clinical outcomes between coronary revascularization versus medical therapy in patients with stable coronary artery disease. Data from Ko DT et al.14
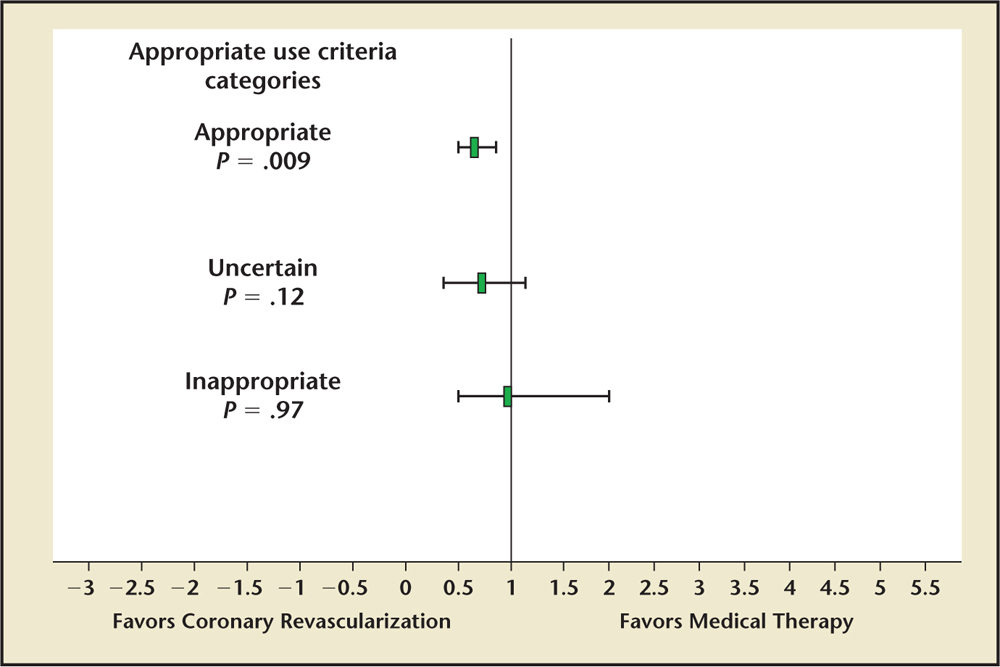
Figure 2. Comparison of 3-year clinical outcomes between coronary revascularization versus medical therapy in patients with stable coronary artery disease. Data from Ko DT et al.14
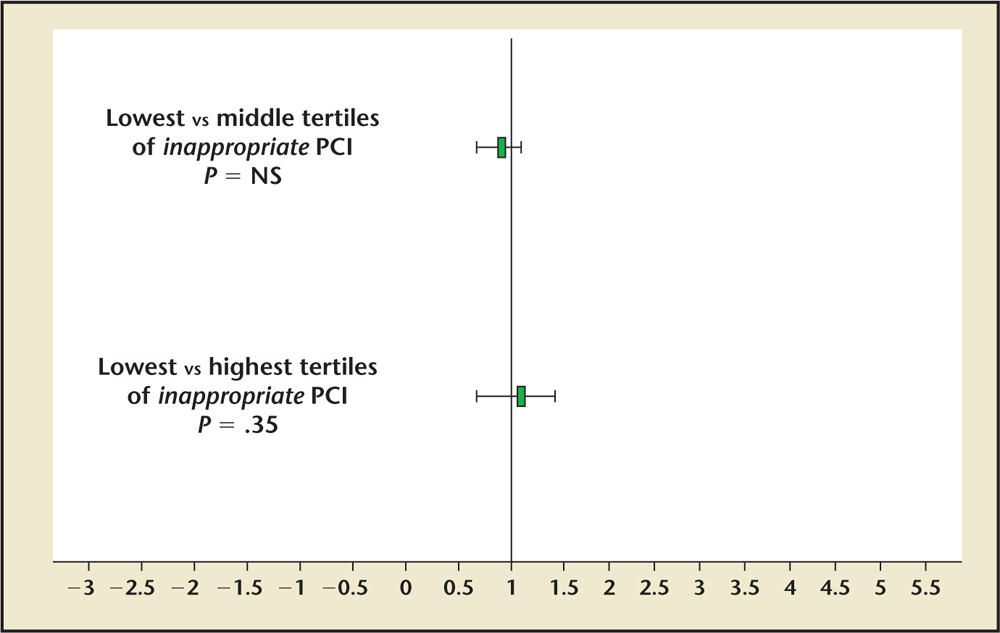
Figure 3. In-hospital clinical outcomes of inappropriate percutaneous coronary interventions (PCI) performed for nonacute indications. Data from Bradley SM et al.15
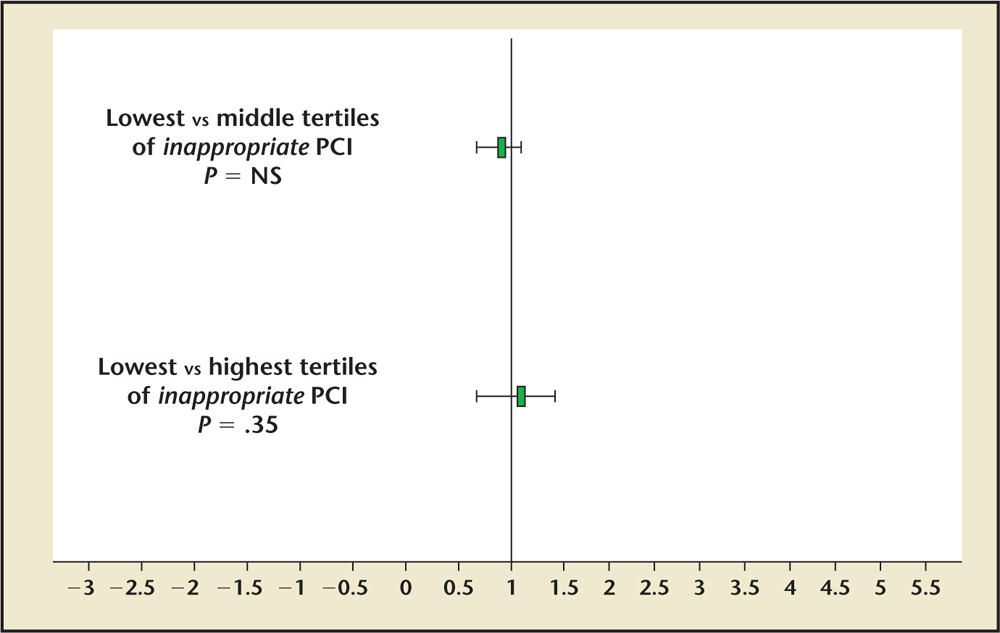
Figure 3. In-hospital clinical outcomes of inappropriate percutaneous coronary interventions (PCI) performed for nonacute indications. Data from Bradley SM et al.15
Main Points
• The appropriateness use criteria (AUC) for coronary revascularization were formulated through the joint efforts of several professional societies. The goals of AUC were to aid in physician decision making and to objectively define the need and context for revascularization. Rigorous use in daily practice and public reporting of adherence to these criteria have exposed some of their deficiencies. The latest percutaneous coronary intervention (PCI) performance measures have acknowledged these limitations and have proposed that AUC should be used for internal quality improvement only at this time.
• The AUC can be used to assist or substantiate clinical decision making. With increasing familiarity and use of AUC by physicians and hospitals, it was hoped that AUC could be prospectively incorporated into patient charts or be part of prior authorization requested from insurance providers.
• The majority of clinical scenarios in the AUC document pertain to stable angina, and the assessment of appropriateness is based on severity of symptoms, number of antianginal medications a patient is taking, extent of ischemia on stress testing, and angiographic complexity of coronary artery disease. Each of these variables is fraught with subjectivity and some of them lack precise definitions, which leads to variability in interpretation and application.
• With innovations in medical technology, ongoing developments in clinical evidence, and unforeseen challenges encountered with use of AUC in clinical practice, the AUC need to be frequently revised. With these adaptations, they may become more widely utilized.
Main Points
• The appropriateness use criteria (AUC) for coronary revascularization were formulated through the joint efforts of several professional societies. The goals of AUC were to aid in physician decision making and to objectively define the need and context for revascularization. Rigorous use in daily practice and public reporting of adherence to these criteria have exposed some of their deficiencies. The latest percutaneous coronary intervention (PCI) performance measures have acknowledged these limitations and have proposed that AUC should be used for internal quality improvement only at this time.
• The AUC can be used to assist or substantiate clinical decision making. With increasing familiarity and use of AUC by physicians and hospitals, it was hoped that AUC could be prospectively incorporated into patient charts or be part of prior authorization requested from insurance providers.
• The majority of clinical scenarios in the AUC document pertain to stable angina, and the assessment of appropriateness is based on severity of symptoms, number of antianginal medications a patient is taking, extent of ischemia on stress testing, and angiographic complexity of coronary artery disease. Each of these variables is fraught with subjectivity and some of them lack precise definitions, which leads to variability in interpretation and application.
• With innovations in medical technology, ongoing developments in clinical evidence, and unforeseen challenges encountered with use of AUC in clinical practice, the AUC need to be frequently revised. With these adaptations, they may become more widely utilized.
The American College of Cardiology Foundation (ACCF), in coordination with the Society for Cardiovascular Angiography and Interventions, the Society of Thoracic Surgeons, the American Association for Thoracic Surgery, the American Heart Association (AHA), the American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography, has published appropriateness use criteria (AUC) to promote evidence-based use of coronary revascularization procedures and deliver high-quality cardiovascular care.1,2 Initially, the AUC received great attention and were widely promoted. The adherence to these criteria has been closely monitored. In some states, individual operator and facility adherence to these criteria is publically reported. Recent studies have reported a wide variability in adherence to these criteria and exposed the inherent limitations of using AUC.3,4 This received great public attention and garnered national headlines. The latest percutaneous coronary intervention (PCI) performance measures have acknowledged these limitations and have proposed that AUC should be used for internal quality improvement only at this time.5 The current and future role of AUC remains uncertain. In this article, we outline the journey of coronary revascularization AUC from its much-publicized inception to its current position, focusing on its strengths, limitations, and challenges.
Development of Coronary Revascularization AUC
Multiple factors led to the development of coronary revascularization AUC. The number of PCI procedures has increased exponentially over the past three decades, as have the associated healthcare costs. Other factors that have contributed to development of AUC are inadequate documentation supporting the need for revascularization and continued advances in medical therapy, coronary imaging, and revascularization techniques (both percutaneous and surgical). The interplay of these factors exposed the large variability in utilization of revascularization strategies, with both overuse and underuse being reported. The AUC were thus developed as a result of a coordinated effort by ACCF and other professional societies to curtail this variability and to serve as an objective tool for clinicians, aid in decision making, and promote appropriate and efficient care.1,2,5
The development of AUC was rigorous and involved several steps (Figure 1), as elaborated below.6
1. Selection of a Technical Panel. The stakeholders from the respective societies were given the opportunity to participate in the AUC writing process by submitting nominees. From this list of nominees, the AUC Task Force and writing group selected the technical panel members. The 17-member technical panel included 4 interventional cardiologists, 4 cardiovascular surgeons, 8 members representing noninterventional cardiologists, other physicians who treat patients with cardiovascular disease and health outcome researchers, and 1 medical officer from a health plan.
2. Development of Clinical Scenarios. The AUC writing group (composed of practicing noninvasive cardiologists, interventional cardiologists, and cardiothoracic surgeons nominated by the leadership of their respective organizations) identified clinical scenarios that are sufficiently common in clinical practice to deserve a systematic approach. They were based on the premise that clinical presentation (acute coronary syndrome [ACS] vs stable coronary artery disease [CAD]), pertinent symptoms (severity of angina), intensity of medical therapy prior to revascularization (specific classes and dosages of anti-anginal medications), the results of a functional stress test, and coronary anatomy were known for each patient. These scenarios distinguished between patients with and without prior coronary artery bypass surgery (CABG). In all, 180 such scenarios were formulated.
3. Rating and Scoring of Scenarios. The technical panel evaluated the appropriateness of revascularization for each clinical scenario after reviewing relevant medical literature and practice guidelines, and rated the scenarios in two separate rounds. In the first round, they rated the scenarios independently. Subsequently, they participated in a group meeting to discuss each scenario, after which they again rated the scenarios. The technical panel scored each indication on a scale of 1 to 9. The scenario was graded as appropriate when it received a numeric score of 7 to 9, indicating that coronary revascularization is likely to improve a patient’s health outcome or survival. Scenarios with scores of 4 to 6 were defined as uncertain, meaning that revascularization use may be reasonable, and scenarios with scores of 1 to 3 were defined as inappropriate, meaning that revascularization is not generally acceptable, not reasonable, and unlikely to improve outcomes or survival. The level of agreement among panelists, as defined by RAND (Santa Monica, CA), was analyzed for each indication based on the BIOMED rule.7 Agreement was defined when four or fewer panelists’ ratings fell outside the 3-point region containing the median score. Disagreement was defined as a situation in which at least five panelists’ ratings fell in both the appropriate, uncertain, and inappropriatecategories. Because the technical panel had 17 representatives, which exceeded the 14- to 16-member requirement for the BIOMED rule, an additional level of agreement analysis was performed for those scenarios in which there was disagreement. This information was used by the moderator to guide the technical panel’s discussion by emphasizing areas of differences among the panelists. Thus, for each scenario, a grade of appropriate, uncertain, or inappropriate, depending on allocated individual and collective scores, was generated. In a recent update, the inappropriate and uncertain terminology was changed to rarely appropriate and may be appropriate, respectively. Also, for a selected number of scenarios, the panel rated the appropriateness of percutaneous versus surgical revascularization using a similar approach.2
Strengths of AUC
The American College of Cardiology (ACC)/AHA guidelines address many aspects of CAD diagnosis and therapy, including the role of revascularization. They are predominantly based on the results of randomized clinical trials and on observations from large national registries. Expert opinion is reserved for instances lacking empiric data. In contrast, AUC are predominantly based on expert opinion, informed by data, and complement practice guidelines by providing the granularity missing in some of these documents. Some of the applications of coronary revascularization AUC are listed below.
Clinical Decision Support Tool
The AUC can be used to assist or substantiate clinical decision making. With increasing familiarity and use of AUC by physicians and hospitals, it was hoped that AUC could be prospectively incorporated into patient charts or be part of prior authorization requested from insurance providers. Some of the electronic medical records have provisions to facilitate incorporation of AUC into patient charts. Furthermore, prior to the introduction of AUC, significant variability in utilization of cardiovascular procedures was noted. There was no objective tool to measure this variability. The AUC fill this void and can be used to quantify how often revascularization procedures are indicated. These efforts may lead to more equitable allocation of health resources, ultimately resulting in better patient outcomes.
Facility and Physician Performance Measure
Adherence to AUC can be used as a quality improvement measure. Physicians and facilities could use AUC prospectively, or retrospectively, to evaluate their performances. Comparing utilization patterns across large cohorts of patients can allow for an assessment of a provider’s or practice’s management strategies with those of its peers. The ACCF strongly believes that an ongoing review of a medical practice using AUC will help guide a more effective and efficient use of healthcare resources and lead to better patient outcomes. This approach also encourages more detailed documentation of the elements included in the AUC algorithm.
Reimbursement
It is expected that procedures will be reimbursed based on compliance with AUC. The appropriate and uncertain or may be appropriate procedures are expected to be reimbursed; however inappropriate or rarely appropriate procedures may be denied (full) reimbursement.
Educational Tool
AUC can be used as an important educational tool. As most of the algorithmic decisions are evidence based, routine use of AUC may promote a logical and consistent decision-making process among practitioners.
Limitations and Challenges
Development of AUC
The majority of the technical panel was composed of noninvasive cardiologists, researchers, other physicians who treat cardiovascular disease, and a representative from the health insurance industry. As these professionals do not perform these procedures, they may not be able to appropriately evaluate and rate the clinical scenarios with regard to their technical aspects, likelihood of success, and resource utilization. A typical example is revascularization of a totally occluded artery, for which assessment of likelihood of success is crucial to defining appropriateness.
Clinical Scenarios
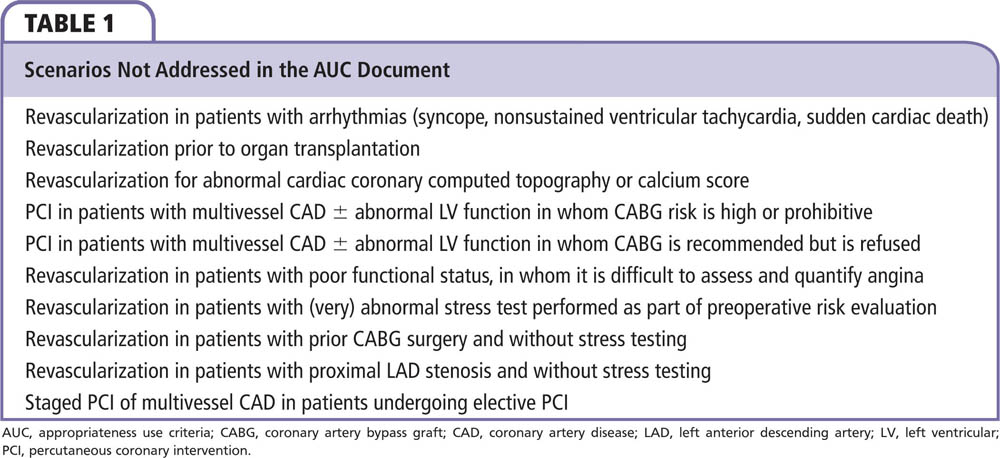
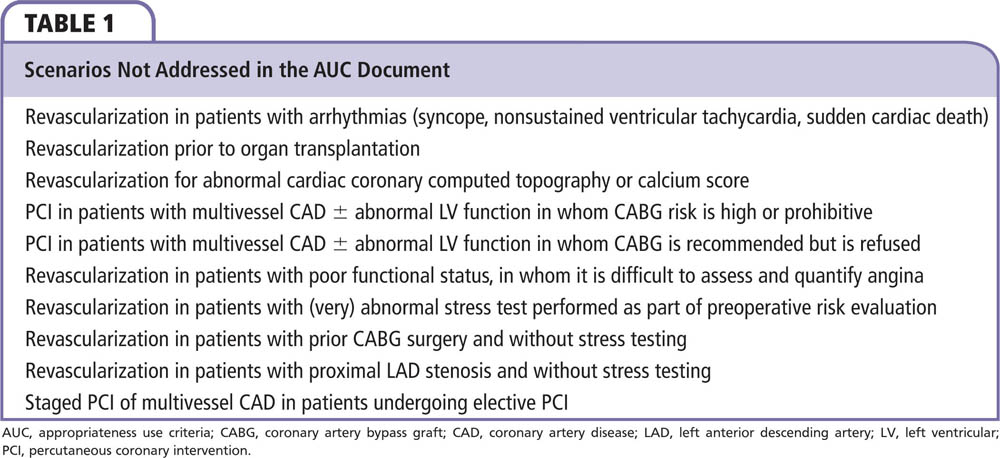
Even though the AUC address many relevant scenarios, not every clinical presentation is represented in the document. This is acknowledged by the writing group that was responsible for developing patient scenarios. Some of the clinical scenarios not listed in the document are presented in Table 1.
The majority of clinical scenarios in the AUC document pertain to stable angina, and the assessment of appropriateness is based on severity of symptoms, number of antianginal medications a patient is taking, extent of ischemia on stress testing, and angiographic complexity of CAD. Each of these variables is fraught with subjectivity and some of them lack precise definitions, which leads to variability in interpretation and application.
One of the common clinical scenarios not represented in the document is the one in which stress testing was performed but results were either unavailable or unclassifiable. This represents a large number of cases in the National Cardiovascular Data Registry (stress test was not available in the medical record for 50% of unclassifiable cases [8.5% of all PCIs] or the magnitude of ischemic risk was not communicated in 42% of unclassifiable cases [7.2% of all PCIs]).8 Even though the AUC document provides a good definition of the severity of ischemia noted on noninvasive testing, it fails to consider the fact that many cardiologists interpret stress test results without the quantitative assessment required to assign the AUC severity score. Moreover, some patients are unable to tolerate stress testing or have inconclusive stress test results because they cannot achieve the target heart rate. Patients with prior CABG surgery and without stress testing are also not addressed in the document.
The severity of angina considered in the AUC document is a subjective assessment performed by the physician. There is significant variability in how it is interpreted. This may lead to manipulation of data in order to improve compliance with AUC. No objective definition of duration of antianginal therapy is listed in the document, nor is the minimal dosage specified. Some patients may not tolerate antianginal therapy and some antianginal medications may be relatively contraindicated in some patients. These aspects of antianginal therapy are not addressed in the document.
Anatomic extent of CAD was classified into few categories in the document. However, this oversimplified classification fails to fully incorporate complexities associated with obstructive CAD, particularly with respect to compromise of major branches, functionality of bypass grafts, and viability of subtended territory. This generalization is particularly relevant to the ability of noninterventional cardiologists to evaluate the feasibility, risk, and benefits of revascularization procedures.
Variability in Implementation and Process of Care
Recent studies have reported wide variability in performance of revascularization procedures and a significant number of inappropriate procedures in patients with stable angina.3,4 Chan and colleagues4 evaluated the appropriateness of PCI in a large group of patients. Of 500,154 PCI procedures in 2009-2010, 71% were performed for ACS. The majority of these (98.6%) were deemed appropriate; among the rest, only 50.4% were appropriate. The remaining were either uncertain (38.0%) or inappropriate (11.6%). The leading causes for an inappropriate designation were lack of angina, low-risk findings on stress test, and insufficient medical treatment prior to PCI. Also noted was substantial variability in the proportion of procedures performed for stable CAD among the institutions (for inappropriate PCI, urban vs semiurban hospitals, adjusted odds ratio [OR] 1.10, 95% confidence interval [CI], 1.07-1.13; P < .001). Further analysis of PCIs deemed inappropriate for nonacute indications showed these procedures were more commonly performed in white men with private insurance receiving care in suburban hospitals.9 These results were widely publicized and called into question the clinical decision-making process and the potential conflict of interest related to reimbursement.
In another state registry analysis of appropriateness of revascularization for nonacute indications, 8168 patients undergoing CABG surgery and 33,970 PCI patients were studied.3 The majority of the CABG procedures were appropriate (90.0%; whereas 1.1% were inappropriate and 8.6% were uncertain) but a significant number of PCIs were categorized as uncertain and inappropriate (36.1% were appropriate, 14.3% were inappropriate, and 49.6% were uncertain). A substantial proportion of patients undergoing PCI classified as inappropriate had 1- or 2-vessel disease without proximal left anterior descending artery (LAD) disease involvement and had received no or minimal anti-ischemic medical therapy. A recently published analysis comparing the Japanese versus US AUC showed that PCI performed in nonacute stable angina patients was significantly more rated as inappropriate using the US AUC than the Japanese AUC.10 This was driven mainly by the scenario of asymptomatic, low- or intermediate-risk patients without lesion in the proximal LAD, which was deemed appropriate by the Japanese and not by the US criteria. Also suboptimal angina therapy was a significant predictor of inappropriate PCI by the US, but not Japanese criteria.
The AUC document expects providers or practices to responsibly document patient information related to clinical scenarios. However, inaccurate data entry may cause miscoding of procedures. Also, the information used to document AUC is not audited. Thus, AUC compliance relies entirely on unaudited data entry by physicians and other practitioners.
Patient Interests
Determinations of appropriateness by the AUC based on angina class fail to take into account the health perceptions and preferences of the patients. This is a fundamental drawback in the development of AUC. In daily clinical practice, the patient plays a critical role in decision making. However, it is fair to acknowledge that patient preferences may be based on incorrect perceptions and subjective factors, such as overestimation of the benefits of PCI, underestimation of its risks, and underestimation of the efficacy of medical therapy alone. Patients may discount benefits of one treatment over another. For example, in patients with complex three-vessel CAD, current literature suggests that CABG may be superior to PCI. However, patients may prefer PCI over CABG because of faster recovery and comfort.
Discordance With Clinical Practice Guidelines
Even though most of the recommendations in the AUC document are in accordance with the ACC/AHA or European Society of Cardiology (ESC) guidelines, some of the common practice scenarios show discordance between the AUC ratings and guidelines11,12:
- Proximal LAD stenosis > 50%. As listed in the ESC guidelines,12 any proximal LAD stenosis of > 50% with documented ischemia is an indication for revascularization in patients with stable angina or silent ischemia. This recommendation is to improve prognosis with revascularization in these patients and is irrespective of antianginal therapy. The corresponding scenarios related to proximal LAD stenosis in the AUC document have variable ratings, from uncertain to appropriate, depending on angina class, noninvasive test findings, and antianginal therapy. For example, a patient with class II stable angina, on one antianginal medication, with low-risk findings on stress testing, and 90% proximal LAD stenosis on coronary angiography would have a class IA recommendation to undergo revascularization according to the guidelines. However, this scenario is assigned a may be appropriate rating by the AUC document. These discordant recommendations may hinder the ability of the practicing physicians to manage their patients.
- Ischemia burden. For patients with > 10% LV ischemia or viability, revascularization is considered a class IIa recommendation in the professional guidelines. Moderate to severe ischemia on stress testing has been shown to be equivalent to ≥ 10% LV ischemia.13 For a patient with class III stable angina, on one antianginal medication, with intermediate risk findings on stress testing, and two-vessel CAD, involving the mid LAD and proximal left circumflex artery, revascularization is considered may be appropriate per the AUC. Unfortunately, quantification of ischemia is more challenging than qualitative assessment and is not routinely performed in clinical practice.
- Invasive assessment of lesion severity with fractional flow reserve is acceptable per the AUC instead of a stress test result showing at least moderate ischemia, even though the results of fractional flow reserve measurement (< or > a specified threshold) are not well correlated with actual size of territory at risk.
AUC and Clinical Outcomes
In a retrospective cohort analysis of 1625 patients with stable CAD who underwent coronary angiography, the association between the different categories of AUC and 3-year clinical outcomes was studied (Figure 1).14 In patients who had appropriate indications for revascularization, only 69% underwent either PCI or CABG, whereas 31% received medical therapy alone. Among patients who received coronary revascularization, 68% of all procedures were considered appropriate, 18% were considered uncertain, and 14% were considered inappropriate. Using the AUC, substantial under- and overutilization of coronary revascularization was noted. In patients who had an appropriate indication for coronary revascularization, the composite endpoint of death or recurrent ACS at 3 years occurred in 11.8% in the coronary revascularization group compared with 16.1% in the no revascularization group (adjusted hazard ratio [HR] 0.61 [0.42-0.88]; P = .009). Also at 3 years, mortality was 3.8% in the coronary revascularization group and 9.0% in the medical therapy group (P < .01); repeat ACS occurred in 9.4% of the coronary revascularization group and in 9.9% of the medical therapy group. However, no difference in clinical outcomes was noted between the revascularization and medical therapy groups at 3 years in patients with uncertain (HR 0.57 [0.28-1.16]; P = .12) or inappropriate(HR 0.99 [0.48-2.02]; P = .97) indications for revascularization. This study suggested that AUC can be used to guide clinical practice, particularly by identifying patients who clearly benefit from revascularization (Figure 2).
In a large registry analysis of 203,351 PCI patients, the association between patient appropriateness for PCI and postprocedural outcomes was studied (Figure 3).15 The hospitals were categorized according to tertiles of inappropriate PCI rates. The range of inappropriate PCI was 0.0% to 8.1% in the lowest tertile, 8.1% to 15.2% in the middle tertile, and 15.2% to 58.6% in the highest tertile. There was no significant difference in in-hospital mortality among the groups (lowest vs middle tertile groups, adjusted OR 0.93; 95% CI, 0.73-1.19; or lowest vs highest tertile groups, adjusted OR 1.12; 95% CI, 0.88-1.43; P = .35 for differences between tertiles). Brener and colleagues16 classified patients undergoing PCI for stable angina according to AUC and studied the relationship between this grading and 3-year mortality. Of 2134 patients included in the study, 80% of procedures were appropriate, 19.4% were uncertain, and only 0.6% were inappropriate. The 3-year mortality was significantly higher in the inappropriate group compared with the other two groups (estimated 3-year survival rates were 92.6%, 91.3%, and 66.9%, respectively; P = .014). However, after adjusting for baseline characteristics, appropriateness level was not an independent predictor of 3-year mortality (P = .26) in a multivariable regression model. In a single-center study of 3817 patients undergoing PCI for stable angina, the prognostic impact of AUC grade on in-hospital and 1-year outcomes was studied.17 There was no difference in 30-day (3.2% vs 7% vs 4.1%; P = .32) and 1-year outcomes (13.1% vs 11.8% vs 15.3%; P = .43) among the appropriate, uncertain, and inappropriate groups, respectively. Thus, the results of some of these studies call into question the role of coronary revascularization AUC as a useful quality assurance or prognostic tool.
Controversial Aspects of AUC
Even though public reporting of coronary revascularization AUC was intended to promote suitable resource utilization and to decrease the number of unnecessary procedures, it may have led to a few untoward consequences. Some patients who do not meet the clinical description of an appropriate procedure per the AUC document may not receive the necessary treatment. This segment of patients, although not currently well defined, will continue to grow as physicians learn to comply and adopt AUC in their practices. Physicians and hospitals do not want to be seen as outliers and be associated with unsuitable practices. Moreover, recent lay press articles (for example, a 2011 Wall Street Journal article18) have attracted national headlines by reporting incidents of inappropriate PCI patterns as equivalent to fraudulent and unethical practices. To circumvent this, the AUC writing group recently changed the terminology from inappropriate to rarely appropriate and from uncertain to may be appropriate.2
The original objective of AUC was to assist in the clinical decision-making process, but recent developments have unfortunately mandated physicians and practices to alter their practice patterns and sometimes modify the decision algorithm to suit the AUC. Currently the AUC are not being utilized to authorize or reimburse for procedures. However, it is projected that insurance companies and other payors will be using AUC to determine appropriateness of procedures in the near future.1,2 This may further alter practice patterns and impact clinical decision making.
Current Status of AUC
Soon after their inception, coronary revascularization AUC were widely publicized and recommended by several professional societies for incorporation into clinical practice. The initial document was fraught with several challenges and exposed the inherent limitations of AUC as too prescriptive and insufficiently granular to address individual patient needs. The document was further revised to address these limitations and also the terminology was changed to accommodate public and physician sentiments.2 The recent PCI performance measures accorded little attention to AUC, acknowledged that AUC are imperfect, and recommended to use them for internal quality improvement only at this time.
Future of AUC
The coronary revascularization AUC are based on a strong foundation of medical literature and clinical experience. However, with innovations in medical technology, ongoing developments in clinical evidence, and unforeseen challenges encountered with use of AUC in clinical practice, the AUC need to be frequently revised. With these adaptations, the AUC may become more widely utilized. Even though the current AUC are imperfect, rising healthcare costs, wide variability in utilization of revascularization procedures, and the current healthcare reform mandate objective measures such as AUC to promote equitable and suitable utilization of resources in order to deliver better patient care. ![]()
Dr. Sattur is the cofounder of AUCMonkey™ (https://aucmonkey.com/cms/), which is an information portal about appropriateness use criteria for cardiovascular procedures.
References
- Patel MR, Dehmer GJ, Hirshfeld JW, et al. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: a report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2009;53:530-553.
- Patel MR, Dehmer GJ, Hirshfeld JW, et al. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 Appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2012;59:857-881.
- Hannan EL, Cozzens K, Samadashvili Z, et al. Appropriateness of coronary revascularization for patients without acute coronary syndromes. J Am Coll Cardiol. 2012;59:1870-1876.
- Chan PS, Patel MR, Klein LW, et al. Appropriateness of percutaneous coronary intervention. JAMA. 2011;306:53-61.
- Nallamothu BK, Tommaso CL, Anderson HV, et al. ACC/AHA/SCAI/AMA-Convened PCPI/NCQA 2013 performance measures for adults undergoing percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures, the Society for Cardiovascular Angiography and Interventions, the American Medical Association-Convened Physician Consortium for Performance Improvement, and the National Committee for Quality Assurance. J Am Coll Cardiol. 2014;63:722-745.
- Patel MR, Spertus JA, Brindis RG, et al; American College of Cardiology Foundation. ACCF proposed method for evaluating the appropriateness of cardiovascular imaging. J Am Coll Cardiol. 2005;46:1606-1613.
- Fitch K, Bernstein SJ, Aguilar MD, et al, eds. The RAND/UCLA Appropriateness Method User’s Manual. Arlington, VA: RAND Corporation; 2001.
- Douglas P, Iskandrian AE, Krumholz HM, et al. Achieving quality in cardiovascular imaging: proceedings from the American College of Cardiology-Duke University Medical Center Think Tank on Quality in Cardiovascular Imaging. J Am Coll Cardiol. 2006;48:2141-2151.
- Chan PS, Rao SV, Bhatt DL, et al. Patient and hospital characteristics associated with inappropriate percutaneous coronary interventions. J Am Coll Cardiol. 2013;62:2274-2281.
- Inohara T, Kohsaka S, Miyata H, et al. Appropriateness of coronary interventions in Japan by the US and Japanese standards. Am Heart J. 2014;168:854.e11-861.e11.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013;82:E266-E355.
- Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501-2555.
- Hachamovitch R, Hayes SW, Friedman JD, et al. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900-2907.
- Ko DT, Guo H, Wijeysundera HC, et al; Cardiac Care Network (CCN) of Ontario Variations in Revascularization Practice in Ontario (VRPO) Working Group. Assessing the association of appropriateness of coronary revascularization and clinical outcomes for patients with stable coronary artery disease. J Am Coll Cardiol. 2012;60:1876-1884.
- Bradley SM, Chan PS, Spertus JA, et al. Hospital percutaneous coronary intervention appropriateness and in-hospital procedural outcomes: insights from the NCDR. Circ Cardiovasc Qual Outcomes. 2012;5:290-297.
- Brener SJ, Haq SA, Bose S, Sacchi TJ. Three-year survival after percutaneous coronary intervention according to appropriateness criteria for revascularization. J Invasive Cardiol. 2009; 21:554-557.
- Barbash IM, Dvir D, Torguson R, et al. Prognostic implications of percutaneous coronary interventions performed according to the appropriate use criteria for coronary revascularization. Cardiovasc Revasc Med. 2013;14:316-320.
- Winslow R, Carreyrou J. Heart treatments overused. Study finds doctors often too quick to try costly procedures to clear arteries. Wall Street Journal. July 6, 2011. http://www.wsj.com/articles/SB1000142405270
2304760604576428323005864648.