Takotsubo Cardiomyopathy: Clinical Characteristics and Outcomes
Sarika K. Desai, DO,1 Jerold Shinbane, MD, FACC,1 Jayanta R. Das, MD,2 James Mirocha, MS,3 Suhail Dohad, MD, FACC2
1Division of Cardiovascular Medicine/Cardiovascular Thoracic Institute, Keck School of Medicine at the University of Southern California, Los Angeles, CA; 2Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles CA, and Cardiovascular Research Foundation at CVMG of Southern California; 3Biostatistics Core, Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA
Takotsubo cardiomyopathy (TC) is a reversible characteristic of left ventricular (LV) ballooning on cardiac imaging without significant coronary artery disease that is precipitated by stress. We performed a retrospective analysis of consecutive patient records to analyze outcomes of patients with TC. Of 100 patients with TC (90% women, mean age 67.7 y, SD = 15.96), 44 patients presented to the emergency room with chest pain, biomarker elevation, and electrocardiographic changes (ST segment elevation in 47%; primary TC) and 56 patients subsequently developed TC after an alternative initial diagnosis (ST segment elevation 27%; secondary TC; P = 0.04). Inciting events differed in those with primary versus secondary TC, with 48% of primary TC patients describing emotional stress; most secondary TC (75%) manifested after a surgical procedure or infection. Average length of hospital stay for primary TC was 6.68 days (SD = 5.32, range 1-28 d) and 18.22 (SD = 20.76, range 3-129 d) for secondary TC (P < .0001). Time to resolution of LV function was equal in both groups. With regard to mortality, eight of nine deaths occurred in secondary TC patients, and all nine deaths were attributable to comorbid medical conditions. Primary TC is frequently related to emotional stress, and carries a benign prognosis. Secondary TC is associated with an acute medical condition and results in a higher death rate.
[ Rev Cardiovasc Med. 2015;16(4):244-252 doi: 10.3909/ricm0794 ]
© 2016 MedReviews®, LLC
Takotsubo Cardiomyopathy: Clinical Characteristics and Outcomes
Sarika K. Desai, DO,1 Jerold Shinbane, MD, FACC,1 Jayanta R. Das, MD,2 James Mirocha, MS,3 Suhail Dohad, MD, FACC2
1Division of Cardiovascular Medicine/Cardiovascular Thoracic Institute, Keck School of Medicine at the University of Southern California, Los Angeles, CA; 2Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles CA, and Cardiovascular Research Foundation at CVMG of Southern California; 3Biostatistics Core, Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA
Takotsubo cardiomyopathy (TC) is a reversible characteristic of left ventricular (LV) ballooning on cardiac imaging without significant coronary artery disease that is precipitated by stress. We performed a retrospective analysis of consecutive patient records to analyze outcomes of patients with TC. Of 100 patients with TC (90% women, mean age 67.7 y, SD = 15.96), 44 patients presented to the emergency room with chest pain, biomarker elevation, and electrocardiographic changes (ST segment elevation in 47%; primary TC) and 56 patients subsequently developed TC after an alternative initial diagnosis (ST segment elevation 27%; secondary TC; P = 0.04). Inciting events differed in those with primary versus secondary TC, with 48% of primary TC patients describing emotional stress; most secondary TC (75%) manifested after a surgical procedure or infection. Average length of hospital stay for primary TC was 6.68 days (SD = 5.32, range 1-28 d) and 18.22 (SD = 20.76, range 3-129 d) for secondary TC (P < .0001). Time to resolution of LV function was equal in both groups. With regard to mortality, eight of nine deaths occurred in secondary TC patients, and all nine deaths were attributable to comorbid medical conditions. Primary TC is frequently related to emotional stress, and carries a benign prognosis. Secondary TC is associated with an acute medical condition and results in a higher death rate.
[ Rev Cardiovasc Med. 2015;16(4):244-252 doi: 10.3909/ricm0794 ]
© 2016 MedReviews®, LLC
Takotsubo Cardiomyopathy: Clinical Characteristics and Outcomes
Sarika K. Desai, DO,1 Jerold Shinbane, MD, FACC,1 Jayanta R. Das, MD,2 James Mirocha, MS,3 Suhail Dohad, MD, FACC2
1Division of Cardiovascular Medicine/Cardiovascular Thoracic Institute, Keck School of Medicine at the University of Southern California, Los Angeles, CA; 2Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles CA, and Cardiovascular Research Foundation at CVMG of Southern California; 3Biostatistics Core, Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA
Takotsubo cardiomyopathy (TC) is a reversible characteristic of left ventricular (LV) ballooning on cardiac imaging without significant coronary artery disease that is precipitated by stress. We performed a retrospective analysis of consecutive patient records to analyze outcomes of patients with TC. Of 100 patients with TC (90% women, mean age 67.7 y, SD = 15.96), 44 patients presented to the emergency room with chest pain, biomarker elevation, and electrocardiographic changes (ST segment elevation in 47%; primary TC) and 56 patients subsequently developed TC after an alternative initial diagnosis (ST segment elevation 27%; secondary TC; P = 0.04). Inciting events differed in those with primary versus secondary TC, with 48% of primary TC patients describing emotional stress; most secondary TC (75%) manifested after a surgical procedure or infection. Average length of hospital stay for primary TC was 6.68 days (SD = 5.32, range 1-28 d) and 18.22 (SD = 20.76, range 3-129 d) for secondary TC (P < .0001). Time to resolution of LV function was equal in both groups. With regard to mortality, eight of nine deaths occurred in secondary TC patients, and all nine deaths were attributable to comorbid medical conditions. Primary TC is frequently related to emotional stress, and carries a benign prognosis. Secondary TC is associated with an acute medical condition and results in a higher death rate.
[ Rev Cardiovasc Med. 2015;16(4):244-252 doi: 10.3909/ricm0794 ]
© 2016 MedReviews®, LLC
KEY WORDS
Broken heart • Cardiomyopathy • Stress cardiomyopathy • Takotsubo
KEY WORDS
Broken heart • Cardiomyopathy • Stress cardiomyopathy • Takotsubo
The mechanism behind TC is not well understood. It has been suggested that myocardial stunning is triggered by a surge in catecholamines; however, an exact mechanism has not been elucidated.
We classified secondary TC as patients who presented with a major medical illness and then subsequently developed TC while hospitalized for that primary medical condition.
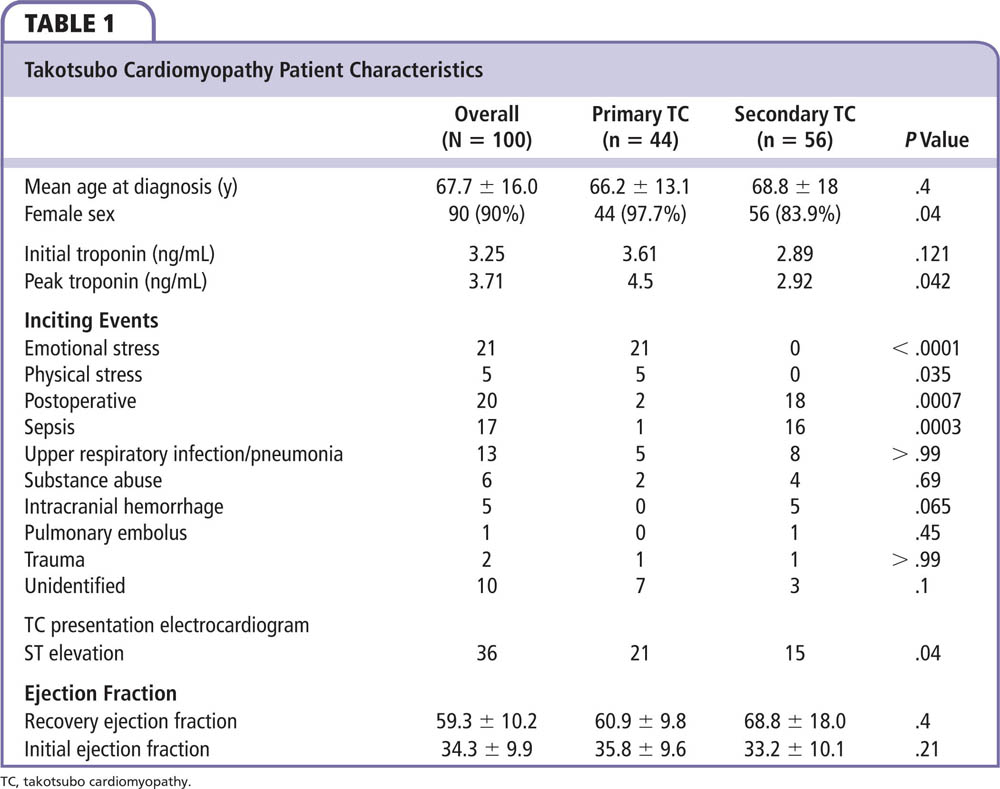
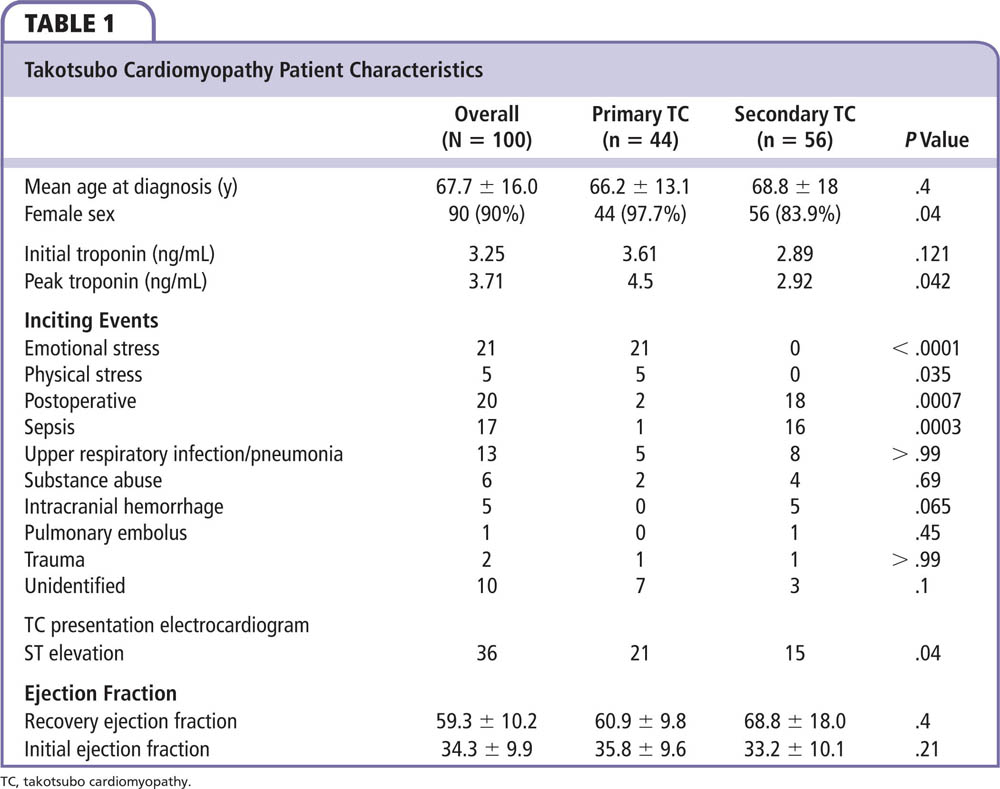
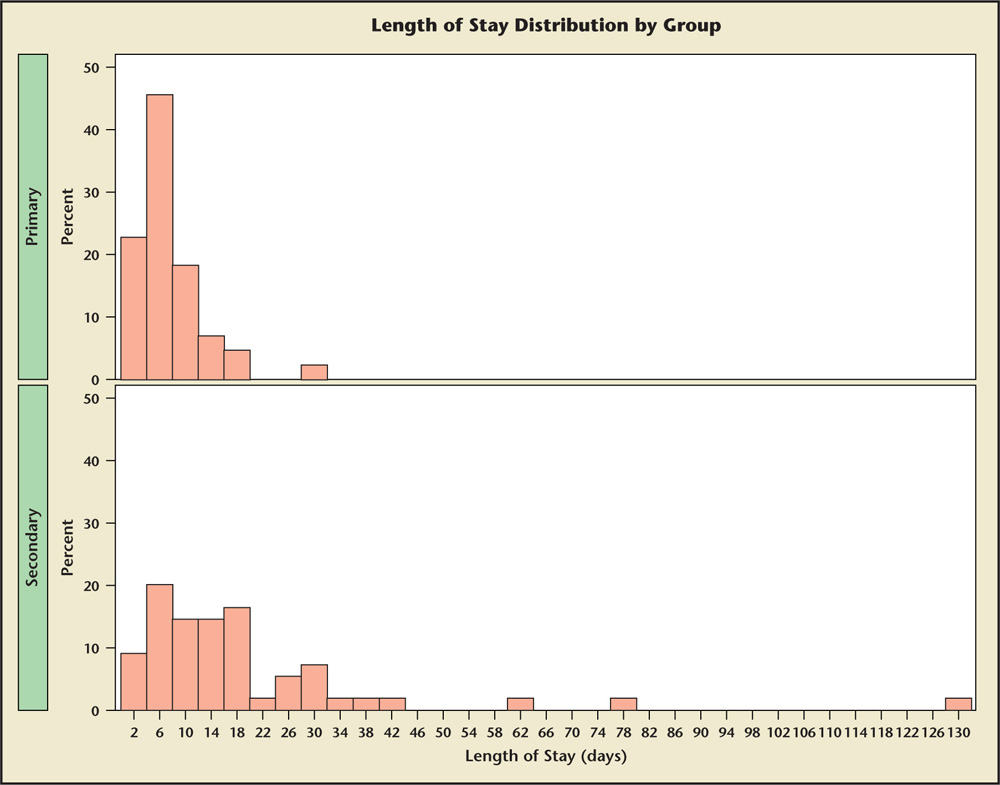
Figure 1. Length of hospital stay: primary and secondary takotsubo cardiomyopathy patients.
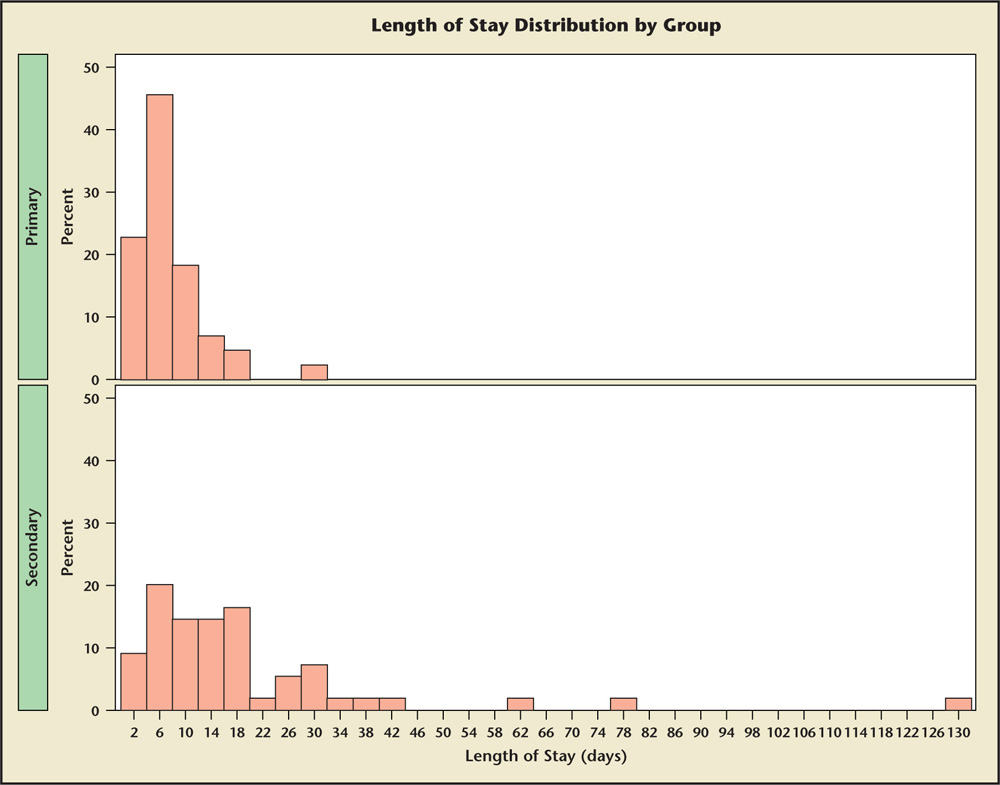
Figure 1. Length of hospital stay: primary and secondary takotsubo cardiomyopathy patients.
Patients may present to the emergency room with manifestations of TC or may develop them after hospital admission.
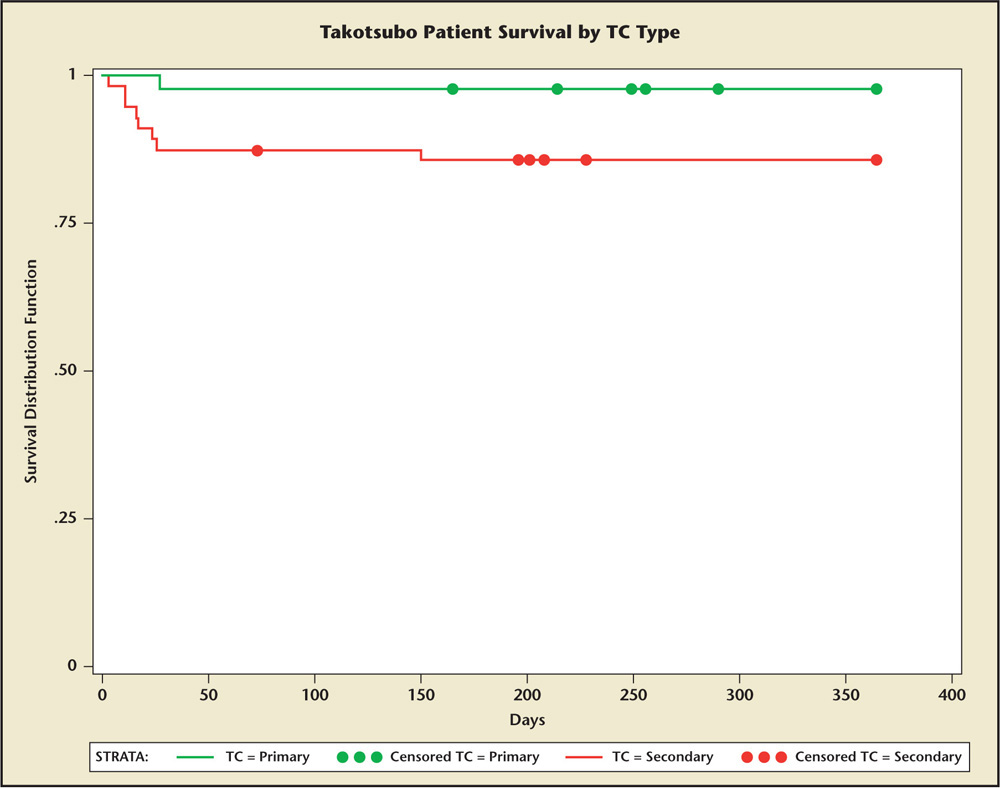
Figure 2. One-year survival (days on the time axis) by takotsubo cardiomyopathy (TC) type.
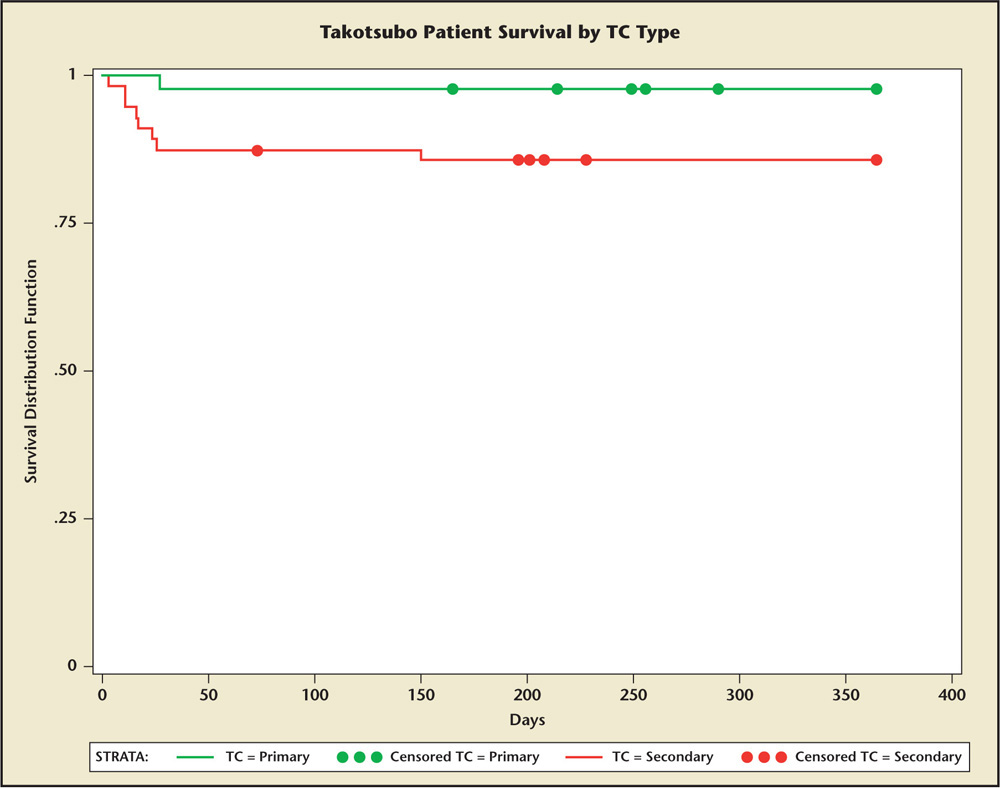
Figure 2. One-year survival (days on the time axis) by takotsubo cardiomyopathy (TC) type.
Main Points
• Takotsubo cardiomyopathy (TC) is a reversible characteristic of left ventricular (LV) ballooning that is on cardiac imaging without significant coronary artery disease and is precipitated by stress.
• Patients with primary TC presented to the emergency room with chest pain, troponin elevation, and electrocardiographic (ECG) abnormalities, whereas those with secondary TC presented to the hospital with alternative diagnoses and subsequently developed TC.
• The average length of hospital stay for those with secondary TC was substantially longer than for patients with primary TC. This reflects the comorbidities of this population that has a more serious underlying disease process.
• The predominance of TC among postmenopausal women suggests that a lack of estrogens may increase susceptibility. In comparison, the lower incidence of TC in healthy men suggests that androgens may play a protective regulatory role.
Main Points
• Takotsubo cardiomyopathy (TC) is a reversible characteristic of left ventricular (LV) ballooning that is on cardiac imaging without significant coronary artery disease and is precipitated by stress.
• Patients with primary TC presented to the emergency room with chest pain, troponin elevation, and electrocardiographic (ECG) abnormalities, whereas those with secondary TC presented to the hospital with alternative diagnoses and subsequently developed TC.
• The average length of hospital stay for those with secondary TC was substantially longer than for patients with primary TC. This reflects the comorbidities of this population that has a more serious underlying disease process.
• The predominance of TC among postmenopausal women suggests that a lack of estrogens may increase susceptibility. In comparison, the lower incidence of TC in healthy men suggests that androgens may play a protective regulatory role.
Takotsubo cardiomyopathy (TC), also referred to as stress-mediated cardiomyopathy, is recognized by a characteristic left ventricular (LV) apical ballooning on cardiac imaging, usually precipitated by a profoundly stressful event. TC is typically characterized by mid and apical ventricular dysfunction found on LV imaging, although several variants have also been described.1 TC findings typically resolve within days to a few weeks after onset. Electrocardiographic (ECG) abnormalities and a rise in cardiac biomarkers mimic an acute myocardial infarction in the absence of any significant coronary artery disease (CAD) or chronic myocardial injury.2 The 2004 Mayo Clinic (Rochester, MN) diagnostic criteria for TC include (1) transient hypokinesis, akinesis, or dyskinesis in the LV mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and frequently, a stressful trigger; (2) the absence of obstructive CAD or angiographic evidence of acute plaque rupture; (3) new ECG abnormalities (ST segment elevation [STE] and/or T-wave inversion) or modest elevation in cardiac troponin; and (4) the absence of pheochromocytoma and myocarditis.3 The incidence of TC is estimated to be at least 1% to 2% of all cases of suspected acute coronary syndrome in the United States.2 The mechanism behind TC is not well understood. It has been suggested that myocardial stunning is triggered by a surge in catecholamines4; however, an exact mechanism has not been elucidated. Although TC is most commonly seen among postmenopausal women who have sudden emotional or physical stress (defined as an activity requiring physical exertion),5Sharkey and colleagues6 identified 9 out of 121 patients with postprocedural/surgical TC. Thus, there are different inciting events in patients with primary versus secondary TC.6
Methods
A retrospective analysis was performed of hospital records between 2005 and 2009 at Cedars-Sinai Medical Center (Los Angeles, CA), for patients identified with TC using electronic records (n = 80). All consecutive patients were identified and none excluded. A small number of patients were manually identified through cardiac catheterization and echocardiography laboratory records in Los Angeles County (n = 12) and University of Southern California Medical Centers (Los Angeles, CA; n = 8) and included in this cohort. No electronic medical records were available at these institutions. The institutional review boards of the participating hospitals approved this study. All cases were confirmed to have LV apical ballooning on LV function analysis with noncontributory CAD, although in some cases it was clinically unfeasible for further workup for CAD due to acuity and type of illness; 90 of the 100 patients underwent coronary angiography. Data including age, sex, clinical presentation to the hospital with TC versus development of TC during the hospital course, etiology of TC, troponin level, presenting ECG abnormalities (STE, tachyarrhythmias, bradycardia, conduction abnormalities), presenting cardiac and psychiatric medications, echocardiographic findings (ejection fraction [EF], wall motion abnormalities), survival to hospital discharge, and days to resolution of echocardiographic findings were reviewed. We classified primary TC as patients who presented with active chest pain, and were found to have dynamic ECG changes with elevation in cardiac biomarkers, and then were subsequently diagnosed with TC. We classified secondary TC as patients who presented with a major medical illness and then subsequently developed TC while hospitalized for that primary medical condition. A Fisher’s exact test was used to calculate P values to determine whether there was a significant difference in inciting events between the primary and secondary TC groups. A Wilcoxon rank-sum test was used to calculate P values among primary and secondary TC patients when analyzing their troponin values. A Kaplan-Meier analysis was performed to evaluate mortality curves.
Results
A total of 100 patients were identified with TC. Among these patients, 44% had primary TC, presenting to the emergency room with chest pain, troponin elevation, and ECG changes, whereas 56% presented to the hospital with alternative diagnoses and subsequently developed secondary TC (Table 1).
Age, Sex, and Ethnicity
The mean age of patients was 67.7 (SD = 15.96, range 23-91 y); 90% of the patients were women (Table 1). The mean age was similar in both subgroups of TC. Similar to the age of previously reported cohorts in the study by Sharkey and colleagues6 and in the initial Japanese population reported by Tsuchihashi and associates,7 our cohort of patients was predominantly postmenopausal women in their early to mid 60s. However, the age range of TC patients has been shown to vary from the first to ninth decade.7 Of the women in the cohort, 43 presented with primary TC and 47 were diagnosed with secondary TC. The majority of men in the study (n = 8, 90%) presented with secondary TC. We analyzed the ethnic distribution among our cohort of patients diagnosed with TC. White women comprised the majority of patients in both groups (71% primary TC, 66% secondary TC). Asians comprised 5% of the total patient population (2% primary TC, 7% secondary TC). African Americans comprised 10% of the patient population (7% primary TC, 13% secondary TC). Hispanics comprised 17% of the patient population (21% primary TC, 14% secondary TC; P = NS for all). It is noteworthy that more nonwhite patients had secondary TC than primary TC.
Inciting Events
Of the 44 patients with primary TC, emotional stress accounted for approximately half of the inciting events (47.7%), whereas upper respiratory infection (URI)/pneumonia (11.4%) and unidentified causes (16%) accounted for the majority of the remaining 50%. Of the 56 patients diagnosed with secondary TC, a postsurgical state (32%) and sepsis (28%) comprised a majority of the inciting events (Table 1).
ECG and Telemetry
Of 44 patients with primary TC, 21 (47%) presented with an ECG demonstrating STE and 23 (53%) presented without STE. In patients with STE (n = 21), only 11 patients described varying emotional stress, 1 described physical stress, 1 had sepsis, 3 had a URI, and 5 had unidentifiable inciting events. In patients without STE (n = 23), 10 described emotional stress, 4 described physical stress, 2 had surgical procedures, 2 had a URI, 2 presented with substance abuse, 1 presented with trauma, and 2 had unidentifiable inciting events (Table 1).
Of the 56 patients with secondary TC, only 15 (27%; P = .04) patients had STE at the time of presentation of TC and 41 (73%) had no STE. Of the 15 patients with STE, 6 presented with a URI, 1 had sepsis, 3 presented after surgical procedures, 3 had an acute intracranial hemorrhage, 1 had acute trauma, and 1 had an acute pulmonary embolus. Of the 41 patients without STE, 15 presented after surgical procedures, 15 with sepsis, 2 with a URI without sepsis, 4 with substance abuse, 2 with an intracranial hemorrhage, and 3 without an identifiable inciting event (Table 1).
Some TC patients were noted to present with arrhythmias; five had atrial fibrillation, one had supraventricular tachycardia, one had torsade de pointes, one had ventricular fibrillation, two had bradycardia, and two had new left bundle branch block. Time to resolution of all acute ECG changes ranged from 2 to 51 days (average 11.9 d). Aside from the difference in frequency of STE, no patterns were distinguishable between primary and secondary TC.
Length of Stay
The average length of hospital stay for primary TC patients was 6.68 days (SD = 5.32, range 1-28 d), whereas the average length of stay for secondary TC patients was 18.22 days (SD = 20.76, range 3-129 d). The result of the Wilcoxon rank-sum test was P < .0001 (Figure 1). This was explained by the comorbidity of the presenting syndrome that caused the secondary TC.
Time to Diagnosis
The average number of days required to diagnose secondary TC was 3.27 days (SD = 4.9, range 1-26 d) after initial admission for the primary comorbid illness. The primary illness can often complicate the clinical scenario and cause a delay in the ability to identify TC cases.
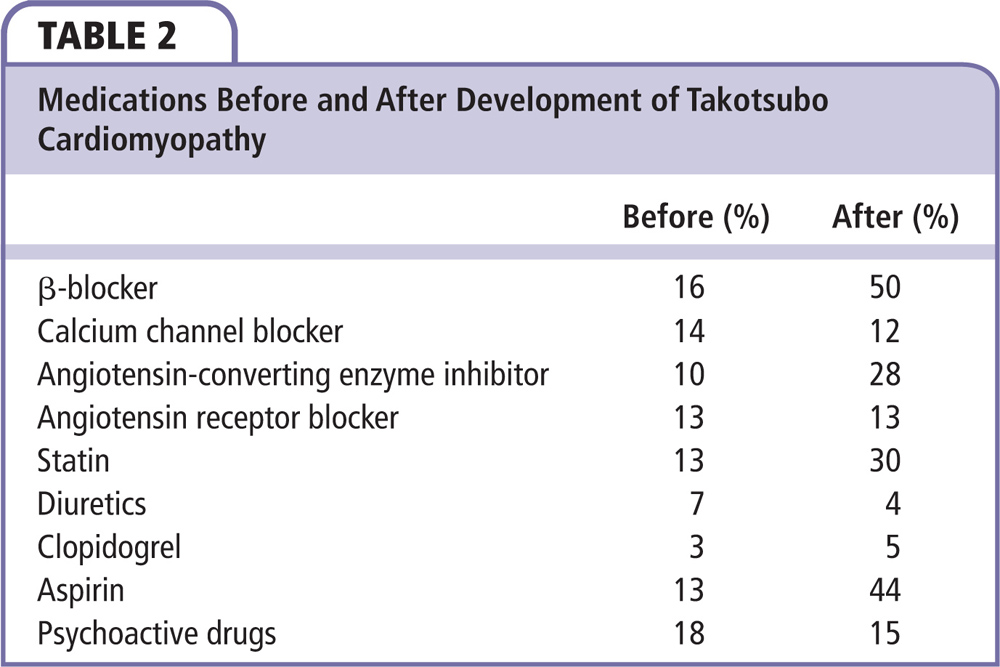
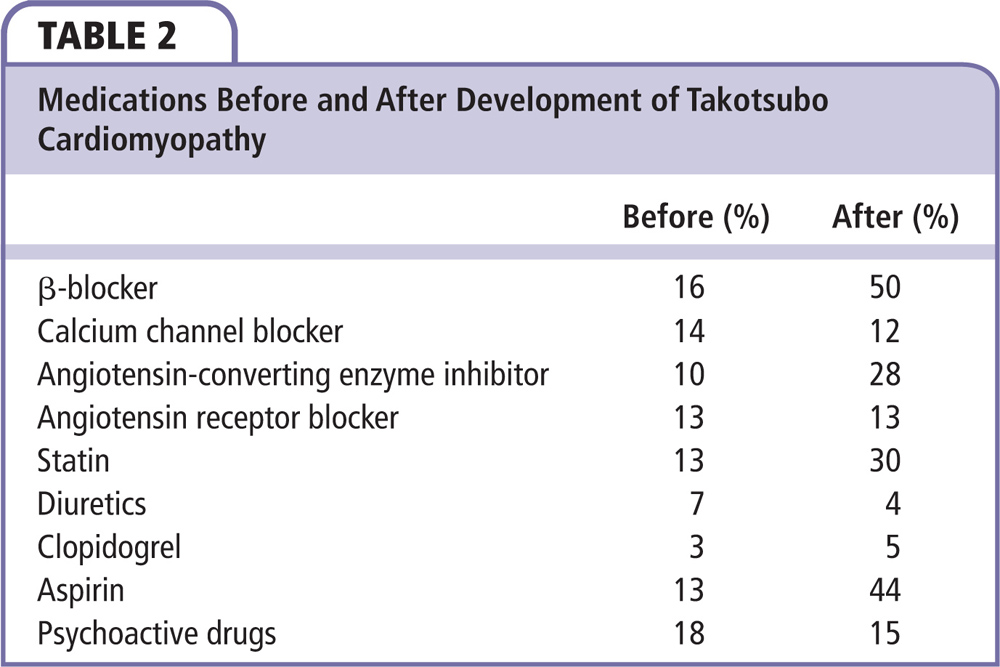
Medications at Time of Diagnosis of TC
At time of diagnosis of TC, a significant number of patients were on psychoactive medications (18%), as well as other cardiac medications, including β-blockers (16%), calcium channel blockers (14%), statins (13%), angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEIs/ARBs; 23%), and aspirin (13%). Upon discharge, as expected, more patients were on cardiovascular medications, including β-blockers (50%), calcium channel blockers (12%), aspirin (44%), statins (30%), and ACEIs/ARBs (41%). It is important to note that very few patients were discharged on a diuretic (Table 2). In general, patient psychoactive medications remained unchanged.
Biomarker Elevation
The mean initial troponin (cardiac troponin I) was 3.61 ng/mL (SD = 5.16, range 0.01-26.71 ng/mL) among primary TC patients and the mean initial troponin was 2.89 ng/mL (SD = 6.92, range 0.01-48.15 ng/mL) among secondary TC patients (P = .121; NS). The peak troponin was 4.5 ng/mL (SD = 6.07) in primary TC patients and it was 2.92 ng/mL (SD = 7.00) in secondary TC patients (P = .042).
LV Function
Total recovery of LV function was demonstrated in all patients studied except for four who died before repeat assessment could be completed. The mean EF recorded on echocardiogram or left ventriculogram on presentation was 34.3% (SD = 9.9, range 10%-60%), whereas the mean EF on follow-up echocardiogram was 59.3% (SD = 10.2, range 30%-84%; Table 1). The mean number of days to receiving a follow-up echocardiogram was 25.02. No difference was noted between the primary and secondary cohorts of TC.
Survival
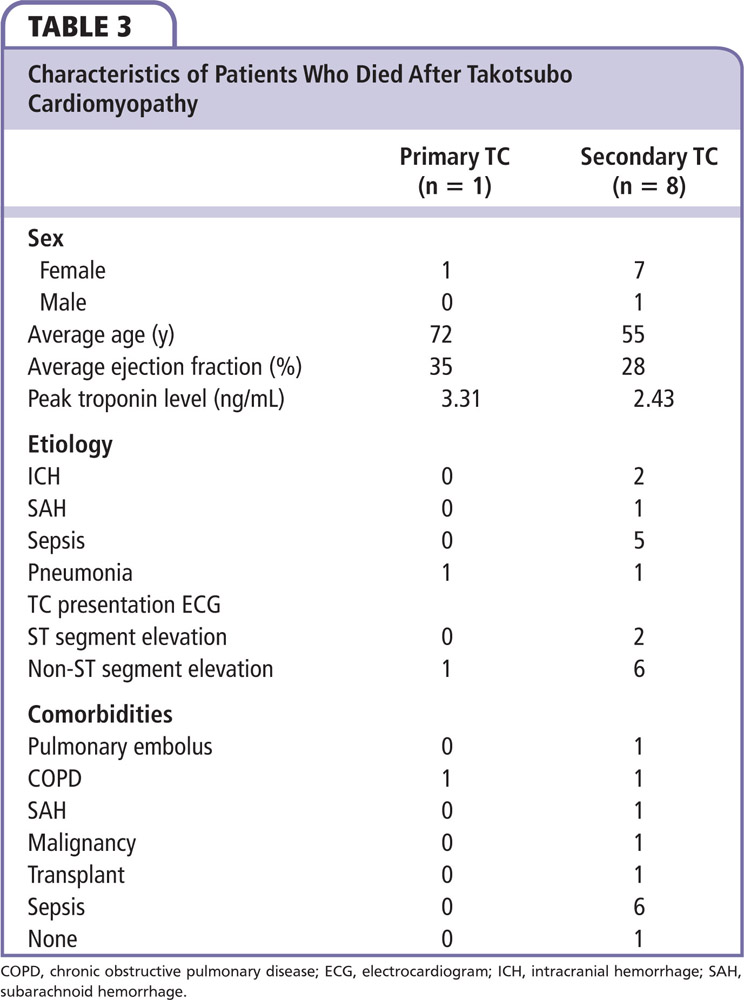
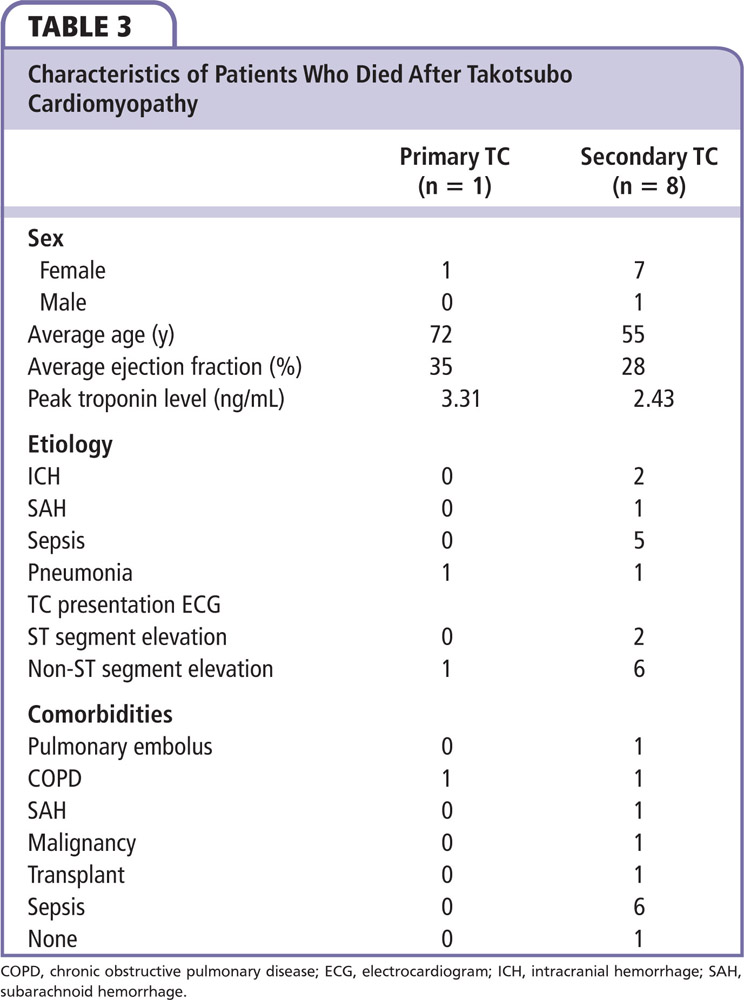
Of the 100 patients, 91 patients survived hospitalization and remained alive in 2011 (Figure 2), whereas nine patients had died (8 of 9 had secondary TC). Of those nine patients, one died of a pulmonary embolus, two died of an intracranial hemorrhage, and six died of septic shock (Table 3). All died as inpatients during the index hospitalization when TC occurred. Of the six septic patients, one patient had end-stage renal disease on hemodialysis and had Killip class III heart failure, two had severe chronic obstructive pulmonary disease with pneumonia, one had a concomitant malignancy and was undergoing chemotherapy (causing subsequent neutropenic fever), another received a liver and kidney transplant during the index hospitalization, and one had a massive pulmonary embolism. With regard to presenting ECG, seven of the nine who died had no STE on ECG at the time of TC diagnosis (1 primary and 6 secondary TC), whereas two of nine had STE on ECG at the time of TC diagnosis (both secondary TC). Of the nine patients who died, eight were women. The average age of this group of nine patients was 57.3 years (SD = 20.1, range 23-77 y) in comparison with 68.7 years (SD = 15.3, range 27-91 y) for the remaining 91 patients (P = .04). The average initial EF of the nine patients who died was 28.9%, compared with 34.3% for the patients who survived (P = .26). The mean time from initial hospitalization to death for this group was 30 days; one patient died on the third day after admission, two died on day 11, one died on day 16, one died on day 17, one died on day 23, one died on day 26, and one died on day 27. One of the nine patients died 150 days after the initial event, however, death was due to a prolonged intensive care unit stay associated with discharge difficulties related to social issues and therefore was excluded from the length-of-stay analysis. TC recurrence was not seen in any of our patients at the time of final follow up in 2011.
Discussion
TC can be precipitated by various causes, including stress, trauma, and medical illnesses with or without procedural interventions. Patients may present to the emergency room with manifestations of TC or may develop them after hospital admission. In previously described cohorts, all patients with TC have been grouped into a single category. We found this heterogeneous mixture unhelpful in understanding why these episodes strike so unexpectedly, resolve fairly rapidly, and occur predominantly in postmenopausal women.6 We find it unconvincing that a single pathophysiologic mechanism can explain this syndrome that generally leaves behind no trace and does not seem to recur in spite of recurrent emotional and medical stress in the same patient. Although there is a 10% reported chance of recurrence of TC in these patients,8 no recurrence was seen in our cohort at 1 year. These characteristics prompted the subdivision of these patients into two fundamentally different clinical presentations. We divided TC patients into those with primary and secondary TC based on either a direct presentation with TC and evaluation in the emergency room, or secondary development of TC during hospitalization for an unrelated cause. Primary TC patients presented to the emergency room with acute symptoms closely related to the inciting event. However, secondary TC was not predominantly diagnosed until the third day of hospitalization. Although TC may have been present at the time of admission, it is unlikely, as there was an acute change in the patient’s medical condition that then prompted further investigation, leading to the diagnosis of TC.
Sharkey and colleagues6 described TC precipitated by intensely stressful emotional events in 47% of patients, whereas in our study only 21% of the overall cohort of patients had an emotional stressor as an identifying trigger. It is possible that their cohort consisted of mostly primary TC patients, which could explain the difference. In their study, 6.6% of patients experienced TC after a medical or surgical procedure, whereas we observed that in 20% of our cohort. In the Japanese cohort studied by Tsuchihashi and associates,7 only 27% had either a severe emotional or physical stressor. In contrast, 75% of secondary TC patients present after a surgical procedure, infection, or sepsis. Secondary TC occurred most commonly in postsurgical patients; 43% of the Japanese cohort7 and 44% of the cohort studied by Sharkey and colleagues6 had a preceding acute medical condition prior to developing TC. In our population, different procedures precipitating secondary TC included recent ablation for atrial fibrillation, gangrenous cholecystitis, angioplasty, hip repair, liver transplantation, and flexible sigmoidoscopy. Similar procedures were also noted in other publications describing TC.6 In addition, secondary TC was commonly seen in patients with intracranial hemorrhage and septic shock. Therefore, physicians need to be vigilant in detecting TC in these settings. We surmise that the clinical profile of TC is broader, including presentation in the emergency department versus in those hospitalized for other medical conditions. As awareness of this syndrome has become increasingly more widespread within the medical community, the appropriate diagnosis is being made more frequently. This may have led to a proportionately higher incidence of diagnosis of secondary TC in our cohort.
The average length of hospital stay for those with secondary TC was substantially longer than for those with primary TC (18.2 vs 6.8 d). This certainly reflects the comorbidities of this population with a more serious underlying disease process. The average number of days required to diagnose TC in our group was approximately 3, with most cases diagnosed within the first 24 hours of admission, which also supports the idea that there is increasing understanding of this disease within the community.
Only 10% of TC cases occurred in men, mostly as secondary TC (90%). None of the previous studies have analyzed specific triggering events in men to make a comparison. It is unclear what protects this population from TC. The predominance of TC among postmenopausal women suggests that estrogens may adversely modulate sympathetic activity and therefore increase susceptibility.9 In comparison, the lower incidence of TC in healthy men suggests that androgens may play a protective regulatory role.9 Sharkey and colleagues6 also point out that TC occurred while 20% of their cohort was already taking β-blockers. Similarly, 16% of our cohort was already on β-blockers when TC was diagnosed. This may be relevant if catecholamines are the etiologic factor in TC; however, it remains unclear why β-blockers fail to protect some patients who develop TC while actively taking them.
The incidence of primary and secondary TC within four different ethnic groups—African Americans, Asians, whites, and Hispanics—was evaluated. Although whites form the majority of this cohort, the incidence of secondary TC was higher in the nonwhite population. It is difficult to draw any substantial conclusions given the small size of the overall cohort.
All patients who underwent serial echocardiography exhibited significant improvement in LV function over time. Average left ventricular ejection fraction (LVEF) at time of presentation was 34%, with a range of 10% to 50%. In the first Japanese population studied, average initial LVEF reported was 41% ± 11% and the average EF upon discharge ranged from 64% ± 10%.7 The LVEF improved by 30% on average in this cohort at time of recovery. A total of 73% of our cohort exhibited recovery of LVEF within the first 30 days of presentation and 92% exhibited complete recovery similar to the 95% of patients in the cohort studied by Sharkey and colleagues.6
Although the review by Hurst and coworkers8 suggests that mortality is rare with TC, our cohort had a mortality rate of 14%. The highest mortality occurred in patients with secondary TC (14%), and a majority of those deaths were related to intracranial pathology or sepsis. These deaths occurred in patients younger than the mean age of TC patients. All secondary TC patients died within a range of 3 to 27 days after admission (Figure 2). In the cohort studied by Sharkey and colleagues,6 there were three in-hospital deaths. The possibility of TC contributing to an already-serious clinical scenario perhaps increases the morbidity of these patients. In the study by Park and coworkers,10 the authors found LV apical ballooning in 28% of their medical intensive care unit patients. Sepsis was the only variable associated with its development. Similarly, sepsis was associated with six of the nine deaths among our secondary TC patients.
Upon reviewing the recent incidence of TC as reported by the International Classification of Diseases, Ninth Revision, Diagnosis Code 429.83, our incidence has remained constant at 34 to 37 patients per year. In comparison with other major institutions, this incidence does not substantially change.11
Limitations
There are several limitations to this study. First, it is a retrospective review of records and subject to the usual biases of such data evaluation. All efforts were made to review all records available and trace patients back to the offices of their primary physician to complete follow-up. All records at our institution are digital and electronic records were available for all the patients. Second, the follow-up echocardiogram occurred at variable times and does not provide an accurate temporal recovery profile of the LV function. Selection bias may have also influenced the study because patients with primary TC were primarily identified through the cardiac catheterization laboratory records. Furthermore, recall bias could have also influenced the study because the degree of emotional stress was self-reported. However, most patients reported to the emergency department within 12 hours of symptom onset, which should theoretically produce a salient description of the emotional trigger. To reduce recall bias, the description of the emotional trigger was analyzed from multiple reports, including the emergency room physician, the internist, and the cardiologist involved. Last, the nine patients who died during hospitalization with primary or secondary TC were too ill for coronary artery angiogram and follow-up echocardiograms demonstrating resolution of TC.
Conclusions
Primary TC related to emotional stress as the most common inciting event frequently presents with STE by ECG and carries a benign prognosis. There is a favorable 1-year outcome for patients with TC triggered by emotional stress. Secondary TC is usually associated with another acute medical condition, often presents without STE, and results in prolonged length of hospital stay and higher death rate. Further prospective studies in larger patient subsets are necessary to evaluate the differences between primary and secondary TC, clinical course, whether secondary TC is a marker or contributor to poor patient prognosis, and potential means to decrease mortality in patients with secondary TC.
Clinical Perspectives
We surmise that the clinical profile of TC is broader, including its presentation in the emergency department versus those hospitalized for other medical conditions. We feel strongly that our paper provides a new perspective on TC by categorizing the presentations in two distinct ways. Clinical competencies in medical knowledge and patient care will be strengthened with our results by enabling the cardiology community to recognize this disease entity earlier. This paper encourages physicians to be more vigilant in detecting TC in various settings. ![]()
The study was funded by Cardiovascular Research Foundation of Southern California. We are thankful to Dr. Noel Bairey-Merz, Dr. Barry Maron, and Dr. Scott Sharkey for their assistance in reviewing the manuscript.
References
- Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408-417.
- Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (takotsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132:809-816.
- Kawai S, Kitabatake A, Tomoike H; Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J. 2007;71: 990-992.
- Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539-548.
- Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118:2754-2762.
- Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (takotsubo) cardiomyopathy. J Am Coll Cardiol. 2010; 55:333-341.
- Tsuchihashi K, Ueshima K, Uchida T, et al; Angina pectoris-Myocardial Infarction Investigations in Japan. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J Am Coll Cardiol. 2001;38:11-18.
- Hurst TR, Prasad A, Askew JW 3rd, et al. Takotsubo cardiomyopathy: a unique cardiomyopathy with variable ventricular morphology. JACC Cardiovasc Imaging. 2010;3:641-649.
- Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352: 539-548.
- Park JH, Kang SJ, Song, JK, et al. Left ventricular apical ballooning due to severe physical stress in patients admitted to the medical ICU. Chest. 2005;128: 296-302.
- Cardiovascular Disease and Other Chronic Conditions in Women. Agency for Healthcare Research and Quality website. http://www.ahrq.gov/research/findings/
factsheets/women/womheart/index.html. Accessed November 7, 2015.