Implementation of the 2013 American College of Cardiology/American Heart Association Blood Cholesterol Guideline Including Data From the Improved Reduction of Outcomes: Vytorin Efficacy International Trial
Boback Ziaeian, MD,1,2 John Dinkler, MD, MPH,1,2 Karol Watson, MD, PhD1,3
1Division of Cardiology, David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Jonathan and Karin Fielding School of Public Health at UCLA, Los Angeles, CA; 3UCLA Barbra Streisand Women's Heart Health Program, Los Angeles, CA
Atherosclerotic cardiovascular disease (ASCVD) is a leading cause of morbidity and mortality in developed countries. The management of blood cholesterol through use of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase inhibitors (statins) in at-risk patients is a pillar of medical therapy for the primary and secondary prevention of cardiovascular disease. The recent 2013 American College of Cardiology/American Heart Association guideline on managing blood cholesterol provides an important framework for the effective implementation of risk-reduction strategies. The guideline identifies four cohorts of patients with proven benefits from statin therapy and streamlines the dosing and monitoring recommendations based on evidence from published, randomized controlled trials. Primary care physicians and cardiologists play key roles in identifying populations at elevated ASCVD risk. In providing a practical management overview of the current blood cholesterol guideline, we facilitate more informed discussions on treatment options between healthcare providers and their patients.
[Rev Cardiovasc Med. 2015;16(2):125-130 doi: 10.3909/ricm0762]
© 2015 MedReviews®, LLC
Implementation of the 2013 American College of Cardiology/American Heart Association Blood Cholesterol Guideline Including Data From the Improved Reduction of Outcomes: Vytorin Efficacy International Trial
Boback Ziaeian, MD,1,2 John Dinkler, MD, MPH,1,2 Karol Watson, MD, PhD1,3
1Division of Cardiology, David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Jonathan and Karin Fielding School of Public Health at UCLA, Los Angeles, CA; 3UCLA Barbra Streisand Women's Heart Health Program, Los Angeles, CA
Atherosclerotic cardiovascular disease (ASCVD) is a leading cause of morbidity and mortality in developed countries. The management of blood cholesterol through use of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase inhibitors (statins) in at-risk patients is a pillar of medical therapy for the primary and secondary prevention of cardiovascular disease. The recent 2013 American College of Cardiology/American Heart Association guideline on managing blood cholesterol provides an important framework for the effective implementation of risk-reduction strategies. The guideline identifies four cohorts of patients with proven benefits from statin therapy and streamlines the dosing and monitoring recommendations based on evidence from published, randomized controlled trials. Primary care physicians and cardiologists play key roles in identifying populations at elevated ASCVD risk. In providing a practical management overview of the current blood cholesterol guideline, we facilitate more informed discussions on treatment options between healthcare providers and their patients.
[Rev Cardiovasc Med. 2015;16(2):125-130 doi: 10.3909/ricm0762]
© 2015 MedReviews®, LLC
Implementation of the 2013 American College of Cardiology/American Heart Association Blood Cholesterol Guideline Including Data From the Improved Reduction of Outcomes: Vytorin Efficacy International Trial
Boback Ziaeian, MD,1,2 John Dinkler, MD, MPH,1,2 Karol Watson, MD, PhD1,3
1Division of Cardiology, David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Jonathan and Karin Fielding School of Public Health at UCLA, Los Angeles, CA; 3UCLA Barbra Streisand Women's Heart Health Program, Los Angeles, CA
Atherosclerotic cardiovascular disease (ASCVD) is a leading cause of morbidity and mortality in developed countries. The management of blood cholesterol through use of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase inhibitors (statins) in at-risk patients is a pillar of medical therapy for the primary and secondary prevention of cardiovascular disease. The recent 2013 American College of Cardiology/American Heart Association guideline on managing blood cholesterol provides an important framework for the effective implementation of risk-reduction strategies. The guideline identifies four cohorts of patients with proven benefits from statin therapy and streamlines the dosing and monitoring recommendations based on evidence from published, randomized controlled trials. Primary care physicians and cardiologists play key roles in identifying populations at elevated ASCVD risk. In providing a practical management overview of the current blood cholesterol guideline, we facilitate more informed discussions on treatment options between healthcare providers and their patients.
[Rev Cardiovasc Med. 2015;16(2):125-130 doi: 10.3909/ricm0762]
© 2015 MedReviews®, LLC
KEY WORDS
Atherosclerotic cardiovascular disease • Low-density lipoprotein cholesterol • High-density lipoprotein cholesterol • Risk reduction • Statin drugs • IMPROVE-IT
KEY WORDS
Atherosclerotic cardiovascular disease • Low-density lipoprotein cholesterol • High-density lipoprotein cholesterol • Risk reduction • Statin drugs • IMPROVE-IT
Statin therapy is the most efficacious medical therapy for the prevention of ASCVD events for at-risk populations.
The new ASCVD risk calculator recommended by the ACC/AHA guideline is based only on the pooled RCTs, with the aim of better modeling populations likely to benefit from statin therapy for primary prevention. Within this calculator, the risk factors that predict the 10-year risk of cardiovascular death, MI, and stroke include age, sex, African American ethnicity, total and HDL cholesterol levels, systolic blood pressure, use of antihypertensive therapy, diabetes, and current tobacco use.
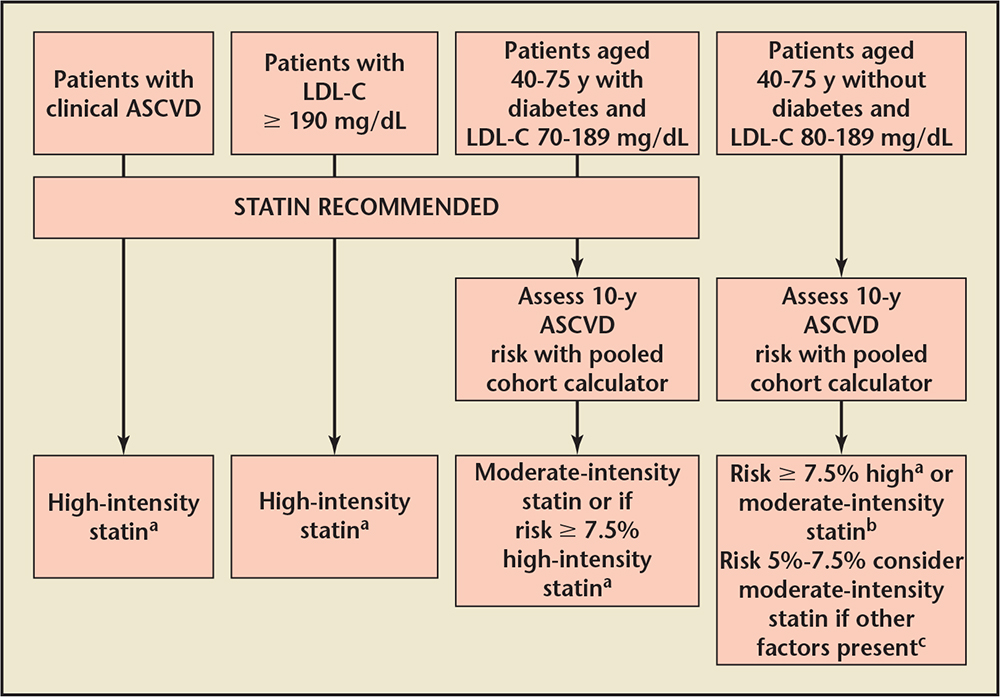
Figure 1. Patient groups and recommended intensity of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reduc-tase inhibitor (statin) therapy.
aHigh-intensity statins reduce LDL-C by ≥ 50%. Medication choices include atorvastatin, 40-80 mg or rosuv-astatin, 20-40 mg.
bModerate-intensity statins reduce LDL-C by 30%-50%. Medication choices include atorvastatin, 10-20 mg, rosuvastatin, 5-10 mg, simvastatin, 20-40 mg, pravastatin, 40-80 mg, lovastatin, 40 mg, fluvastatin XL, 80 mg, fluvastatin, 40 mg twice daily, or pitavastatin, 2-4 mg.
cIn these patients, clinicians should consider other factors that may modify risk for ASCVD such as family history of early ASCVD, high-sensitivity-CRP ≥ 2 mg/L, LDL-C ≥ 160 mg/dL, CAC score of ≥ 300 Agatston units or ≥ 75th percentile for age, sex, and ethnicity, and ABI < 0.9.
ABI, ankle-brachial index; ASCVD, atherosclerotic cardiovascular disease; CAC, coronary artery calcium; CRP, C-reactive protein; LDL-C, low-density lipoprotein cholesterol.
Beyond dietary recommendations, engaging patients in a discussion about physical activity is critical, as sustained moderate levels of activity are effective for the both the primary and secondary prevention of ASCVD.
For appropriately selected patients, the adverse event rates among statin users are low.
In [the IMPROVE-IT] trial, 18,144 patients with ST-segment elevation MI, non-ST-segment elevation MI, or unstable angina, were randomized to receive either ezetimibe, 10 mg + simvastatin, 40 mg or simvastatin, 40 mg alone.
Main Points
•Atherosclerotic cardiovascular disease (ASCVD) is a leading cause of morbidity and mortality in developed countries. The management of blood cholesterol through use of statins in at-risk patients is a pillar of medical therapy for the primary and secondary prevention of cardiovascular disease. Despite this, recent studies find evidence for significant undertreatment of high-risk patients..
•In late 2013, the American College of Cardiology/American Heart Association Task Force on Practice Guidelines provided updated recommendations on managing blood cholesterol with the goal of reducing the risk of ASCVD.
• Statin therapy is the single most efficacious medical therapy for the prevention of ASCVD events for at-risk populations. The guideline committee found no evidence from randomized controlled trials supporting the theory that nonstatin cholesterol-lowering therapies reduce ASCVD events, and concluded that using these agents in any patient population could not be recommended.
• Recently released data from the Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) will likely influence the guidelines, however, including upgrading the current recommendation for adding a nonstatin (specifically ezetimibe) to statin therapy to a higher level of evidence.
Main Points
• Hypertension remains a leading cause of major cardiovascular diseases worldwide. Renal denervation (RDN) using intra-arterial catheter-based radiofrequency (RF) ablation was developed to simulate surgical splanchnicectomy, which had a high rate of significant complications.
• Different technologies have been developed to achieve RDN. The device should be able to achieve a maximal and irreversible destruction of the renal nerves, in a predictable pattern, while minimizing injury to the renal artery. The two technologies that have been used in humans thus far are RF ablation-based RDN and ultrasound energy-based RDN.
• Although many registries have found RDN to be an effective and safe procedure to control blood pressure in patients with resistant hypertension, SYMPLICITY HTN-3, the first blinded sham-controlled trial, failed to reach its primary efficacy endpoint, defined as a change in office systolic blood pressure at 6 months.
• Although SYMPLICITY HTN-3 successfully addressed many issues that might have biased the previously published data, incomplete denervation along with differences in the study design and population may have accounted for the discordance with prior studies. These factors should direct future renal denervation studies.
• Studies are underway to examine the effects of RDN on other conditions other than hypertension, such as insulin resistance, left ventricular hypertrophy, and atrial fibrillation.
In 2010, coronary heart disease alone resulted in 1 of every 6 deaths and 620,000 myocardial infarctions (MIs). Additionally, 800,000 Americans had an acute stroke and 8.5 million lived with peripheral arterial disease. The estimated combined direct and indirect cost of cardiovascular disease and stroke was $315.4 billion in 2010.1 Despite this, recent studies find evidence for significant under-treatment of high-risk patients. An estimated 58.2% of individuals with coronary heart disease and 52.0% of people older than 40 years with diabetes used 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase inhibitors (statins) in 2010.2
In late 2013, the American College of Cardiology/American Heart Association (ACC/AHA) Task Force on Practice Guidelines provided updated recommendations on managing blood cholesterol with the goal of reducing the risk of atherosclerotic cardiovascular disease (ASCVD).3 Atherosclerosis is the pathologic process in which fat and cholesterol-laden plaques infiltrate arterial walls, leading to progressive stenosis and risk for acute coronary syndrome and stroke.4 Foremost, clinicians should prioritize lifestyle modifications through diet, exercise, weight maintenance, and smoking cessation to reduce cardiovascular risk in all populations. The foundation of cardiovascular prevention consists of cost-effective and safe lifestyle modifications.5 The updated 2013 cholesterol guideline specifically reviewed randomized controlled trials (RCTs), systemic reviews, and meta-analyses of RCTs reporting the hard outcomes of cardiovascular death, MIs, and stroke. Statin therapy is the most efficacious medical therapy for the prevention of ASCVD events for at-risk populations.6 The guideline committee found no RCT evidence supporting the theory that nonstatin cholesterol-lowering therapies reduce ASCVD events, and concluded that using these agents in any patient population could not be recommended.
What's New in the Guideline
Identifying populations at risk of ASCVD is more important than treating to target cholesterol levels, as the previous guidelines had recommended.7 Prior research has modeled the problems with a treat-to-target strategy, including inefficiencies of cost, as well as over- and undertreatment of patients.8,9 A separate guideline committee undertook the challenge of identifying the best risk calculator for detecting patients likely to benefit from primary prevention with statin therapy.
Since the pioneering and continuous Framingham Heart Study in 1948, cardiovascular researchers have identified predisposing factors of ASCVD. Some of the risk factors studied in various multivariate models include age, sex, ethnicity, family history, elevated total and low-density lipoprotein (LDL) cholesterol level, low high-density lipoprotein (HDL) cholesterol level, systolic blood pressure, hypertension, diabetes, tobacco use, body mass index, high-sensitivity C-reactive protein (hs-CRP) level, chronic kidney disease, and computed tomography (CT) coronary artery calcium scoring.10-13 The new ASCVD risk calculator recommended by the ACC/AHA guideline is based only on the pooled RCTs, with the aim of better modeling populations likely to benefit from statin therapy for primary prevention.14 Within this calculator, the risk factors that predict the 10-year risk of cardiovascular death, MI, and stroke include age, sex, African American ethnicity, total and HDL cholesterol levels, systolic blood pressure, use of antihypertensive therapy, diabetes, and current tobacco use. Individuals between the ages of 40 and 79 years with a 10-year risk of at least 7.5% for an ASCVD event are considered likely to benefit from statin therapy. For patients with a 10-year risk between 5.0% and 7.5%, consideration may be given to statin therapy. Several additional factors not included in the risk calculator can be considered in revising a patient's risk upward: family history of early ASCVD in a first-degree relative, hs-CRP, CT coronary artery calcium scoring, and ankle-brachial index.14 However, the cost effectiveness of some of the more advanced laboratory tests and imaging modalities have not been well validated for the general population.15 Based on the new guidelines, researchers estimate that the number of adults in the United States who are eligible for statin therapy would increase to approximately 56 million.16 That increase of 13 million newly eligible adults primarily includes adults without ASCVD but at increased 10-year risk based on the pooled risk calculator.
Another innovative change in the new cholesterol guideline is direction on the recommended intensity of statin therapy. High-intensity statins that reduce LDL cholesterol levels by more than 50% on average are recommended for individuals with clinical ASCVD, those with LDL cholesterol ≥ 190 md/dL, high-risk patients with diabetes, and those with a 10-year risk of ASCVD events ≥ 7.5% (Figure 1). Moderate-intensity statins that lower LDL cholesterol by 30% to 50% are recommended for lower-risk diabetic patients. Moderate-intensity statins may be used in those who cannot tolerate higher-dose statins for primary prevention, or patients over the age of 75 years. The addition of nonstatin lipid-lowering therapies is not recommended, as there is insufficient evidence of the long-term patient benefits.
Additional Emphasis: A Patient-centered Approach to Management and Risk Assessment
Lifestyle management continues to be a cornerstone of cardiovascular risk reduction that physicians should emphasize prior to and during cholesterol-lowering drug therapy. Encouraging intake of vegetables, fruits, and whole grains, as suggested by the Dietary Approaches to Stop Hypertension (DASH) diet, is associated with lower cardiovascular risk. Decreasing sodium intake to no more than 2400 mg/d is associated with lower blood pressure, especially when combined with a DASH-style diet. Beyond dietary recommendations, engaging patients in a discussion about physical activity is critical, as sustained moderate levels of activity are effective for the both the primary and secondary prevention of ASCVD.5 The American College of Sports Medicine guidelines on physical activity recommend 150 minutes of moderate-intensity activity each week for maximum cardiovascular benefits. This can be achieved either through 5 30-minute sessions of moderate activity, or shorter sessions (eg, 20 min) of vigorous activity approximately 3 days per week.17 Observational studies have shown that these levels of physical activity reduce cardiovascular disease, all-cause mortality, blood pressure, and type 2 diabetes, in addition to improving CRP level, lipid levels, and insulin sensitivity.5,17-21 In a large observational cohort, men with five healthy habits—healthy diet, moderate alcohol consumption, not smoking, being physical active, and having low abdominal adiposity— compared with men without any of the five healthy habits had an 86% lower risk of MI.22
Another critical element of the new cholesterol guideline is engaging patients in a discussion about their long-term risk for ASCVD. To assist physicians in this task the ASCVD risk calculator is a tool that should be integrated into such discussions. In addition, the guideline committee emphasizes that a patient's preferences and treatment options, including lifestyle modification, should be part of the complete conversation. Prior to using medication to modify risk, physicians need to consider the potential for adverse events, drug-drug interactions, and overall benefit of therapy. For appropriately selected patients, the adverse event rates among statin users are low. Moderate-intensity statins may lead to 1 excess case of diabetes in 1000 statin users per year and 3 excess cases per 1000 in high-intensity statin users. Importantly, the harm from excess diabetes is unlikely to be equivalent to the benefits of preventing cardiovascular death, MI, and stroke. The rates of excess myopathy and hemorrhagic strokes are approximately 1 in 10,000.23
Managing Atherosclerotic Risk
After carefully discussing the benefits of statin therapy with a patient, a shared decision should be made regarding the initiation of therapy. Next, a baseline fasting lipid panel should be obtained. In 1 to 3 months of treatment, a lipid panel may be repeated to assess adherence and response to therapy (high-intensity statins should lower LDL cholesterol by ≥50% and moderate-intensity statins should lower LDL cholesterol by 30% to 50%). If response is inadequate, clinicians may need to emphasize further lifestyle modification, intensify statin therapy (for those on moderate-intensity statins), or encourage the importance of adherence. Changes in dose or switching to alternate statins should be reassessed in 1 to 3 months to evaluate treatment response and monitor side effects.
Incorporation of New Data Into the Guideline
The guideline represents the best available evidence at the time of its publication. Since then, however, data from at least one clinical trial have been released that, after publication of the peer-reviewed manuscript, will likely influence the guideline. The Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) results were first reported at the AHA 2014 Scientific Sessions.22 In this multinational trial, 18,144 patients with ST-segment elevation MI, non-ST-segment elevation MI, or unstable angina (UA) were randomized to receive either ezetimibe, 10 mg + simvastatin, 40 mg or simvastatin, 40 mg alone. Baseline LDL cholesterol levels were 95 mg/dL in both arms; the median follow-up LDL cholesterol level was 53.7 mg/dL in the ezetimibe + simvastatin arm versus 69.5 mg/dL in the simvastatin-only arm. The primary endpoint of cardiovascular death/ MI/UA/coronary revascularization was significantly lower in the ezetimibe + simvastatin arm compared with the simvastatin-only arm (32.7% vs 34.7%, hazard ratio 0.94, 95% confidence interval, 0.89-0.99; P = .016). This corresponded to a number needed to treat of 50 patients to prevent 1 event. The guidelines currently state that addition of a nonstatin agent may be considered under certain clinical situations and that preference should be given to nonstatin cholesterol-lowering drugs shown to reduce ASCVD events in RCTs. However, with IMPROVE-IT, possible updates to the guidelines, include the following:
- Upgrading the current recommendation for adding a nonstatin (specifically ezetimibe) to statin therapy from a IIB recommendation, level of evidence (LOE) C, to a IIa (or higher) recommendation, LOE: B
- The current guidelines state that “in patients in whom there is a less than anticipated therapeutic response” addition of a nonstatin agent can be considered. IMPROVE-IT, however, suggests that even patients who have the anticipated therapeutic response to high-intensity statins may still derive benefit from addition of ezetimibe.
- Finally, the following evidence statement is no longer accurate: “There is insufficient data to evaluate the additional efficacy and safety of ezetimibe in combination with a statin compared with a statin alone.”
The guidelines writing committee is dedicated to incorporating new evidence into the guidelines when available. As soon as the peer-reviewed publication of IMPROVE-IT is available, we anticipate the incorporation of these data into the guidelines.
Conclusions
The recent ACC/AHA blood cholesterol guideline provides a robust synthesis of the evidence base for primary and secondary prevention of ASCVD. This is an American guideline, and guidelines from other countries may differ. The ACC/AHA guideline derives from a compilation of the best available evidence regarding which strategies are most effective for reducing ASCVD events and mortality. These newer guidelines emphasize reducing hard outcomes such as death, MI, and stroke. Previous iterations of the cholesterol guidelines integrated studies showing reductions in surrogate markers, which increasingly may not correlate directly with patient outcomes. The new guideline provides a simplified approach to identifying patients with elevated cardiovascular risk and a high likelihood of benefit from statin therapy. A fixed-dose statin approach is now advocated over the prior treat-to-target method, which lacked sufficient evidence. Assessing cardiovascular risk is part of an ongoing conversation between patient and clinician. The ultimate decision to prescribe therapy should result from an informed consent, shared decision-making framework. Because ASCVD is the leading cause of morbidity and mortality in developed countries, effective lifestyle and medical therapies can reduce the global burden of cardiovascular disease. This updated cholesterol guideline promotes a patient-centered and efficient strategy to achieve this goal. ![]()
Drs. Ziaeian and Dinkler have no real or apparent conflicts of interest to disclose. Dr. Watson is a clinical trial adjudicator for Merck & Co (Whitehouse Station, NJ).
References
- Go AS, Mozaffarian D, Roger VL, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6-e245.
- Johansen ME, Green LA, Sen A, et al. Cardiovascular risk and statin use in the United States. Ann Fam Med. 2014;12:215-223.
- Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63(25 Pt B):2889-2934.
- Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368:2004-2013.
- Eckel RH, Jakicic JM, Ard JD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B): 2960-2984.
- Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD004816.
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421.
- Hayward RA, Krumholz HM, Zulman DM, et al. Optimizing statin treatment for primary prevention of coronary artery disease. Ann Intern Med. 2010;152:69-77.
- Hayward RA, Krumholz HM. Three reasons to abandon low-density lipoprotein targets: an open letter to the Adult Treatment Panel IV of the National Institutes of Health. Circ Cardiovasc Qual Outcomes. 2012;5:2-5.
- D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743-753.
- Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611-619.
- Ridker PM, Paynter NP, Rifai N, et al. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243-2251, 4p following 2251.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210-215.
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935-2959.
- Hlatky MA, Greenland P, Arnett DK, et al; American Heart Association Expert Panel on Subclinical Atherosclerotic Diseases and Emerging Risk Factors and the Stroke Council. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408-2416.
- Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422-1431.
- Garber CE, Blissmer B, Deschenes MR, et al; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334-1359.
- Sesso HD, Paffenbarger RS Jr, Lee IM. Physical activity and coronary heart disease in men: The Harvard Alumni Health Study. Circulation. 2000;102:975-980.
- Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716-725.
- Tanasescu M, Leitzmann MF, Rimm EB, et al. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288:1994-2000.
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Office of Disease Prevention and Health Promotion website. http://www.health.gov/paguidelines/Report/pdf/
CommitteeReport.pdf. Accessed May 12, 2015. - Akesson A, Larsson SC, Discacciati A, Wolk A. Lowrisk diet and lifestyle habits in the primary prevention of myocardial infarction in men: a populationbased prospective cohort study. J Am Coll Cardiol. 2014;64:1299-1306.
- Mihaylova B, Emberson J, Blackwell L, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: metaanalysis of individual data from 27 randomised trials. Lancet. 2012;380:581-590.