Silk Suture Embolization for Sealing Distal Coronary Artery Perforation: Report of Two Cases
Yue Li, MD,1 Guotao Wang, MD,2 Li Sheng, MD,1 Jingyi Xue, MD,1 Danghui Sun, MM,1 Yongtai Gong, MD,1
1Cardiovascular Department, the First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, China; 2Cardiovascular Department, Daqing People's Hospital, Daqing, Heilongjiang Province, China
Coronary artery perforation (CAP) is an infrequent yet potentially life-threatening complication of percutaneous coronary intervention. We report, for the first time, two cases of successful closure of guidewire-induced distal CAP with silk suture embolization using a microcatheter. This technique appears to be safe, simple, and effective for the treatment of distal guidewire perforations, even in refractory cases.
[Rev Cardiovasc Med. 2015;16(2): 165-169 doi: 10.3909/ricm0768]
© 2015 MedReviews®, LLC
Silk Suture Embolization for Sealing Distal Coronary Artery Perforation: Report of Two Cases
Yue Li, MD,1 Guotao Wang, MD,2 Li Sheng, MD,1 Jingyi Xue, MD,1 Danghui Sun, MM,1 Yongtai Gong, MD,1
1Cardiovascular Department, the First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, China; 2Cardiovascular Department, Daqing People's Hospital, Daqing, Heilongjiang Province, China
Coronary artery perforation (CAP) is an infrequent yet potentially life-threatening complication of percutaneous coronary intervention. We report, for the first time, two cases of successful closure of guidewire-induced distal CAP with silk suture embolization using a microcatheter. This technique appears to be safe, simple, and effective for the treatment of distal guidewire perforations, even in refractory cases.
[Rev Cardiovasc Med. 2015;16(2): 165-169 doi: 10.3909/ricm0768]
© 2015 MedReviews®, LLC
Silk Suture Embolization for Sealing Distal Coronary Artery Perforation: Report of Two Cases
Yue Li, MD,1 Guotao Wang, MD,2 Li Sheng, MD,1 Jingyi Xue, MD,1 Danghui Sun, MM,1 Yongtai Gong, MD,1
1Cardiovascular Department, the First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang Province, China; 2Cardiovascular Department, Daqing People's Hospital, Daqing, Heilongjiang Province, China
Coronary artery perforation (CAP) is an infrequent yet potentially life-threatening complication of percutaneous coronary intervention. We report, for the first time, two cases of successful closure of guidewire-induced distal CAP with silk suture embolization using a microcatheter. This technique appears to be safe, simple, and effective for the treatment of distal guidewire perforations, even in refractory cases.
[Rev Cardiovasc Med. 2015;16(2): 165-169 doi: 10.3909/ricm0768]
© 2015 MedReviews®, LLC
KEY WORDS
Perforation • Coronary • Guidewire • Silk suture • Complication
KEY WORDS
Perforation • Coronary • Guidewire • Silk suture • Complication
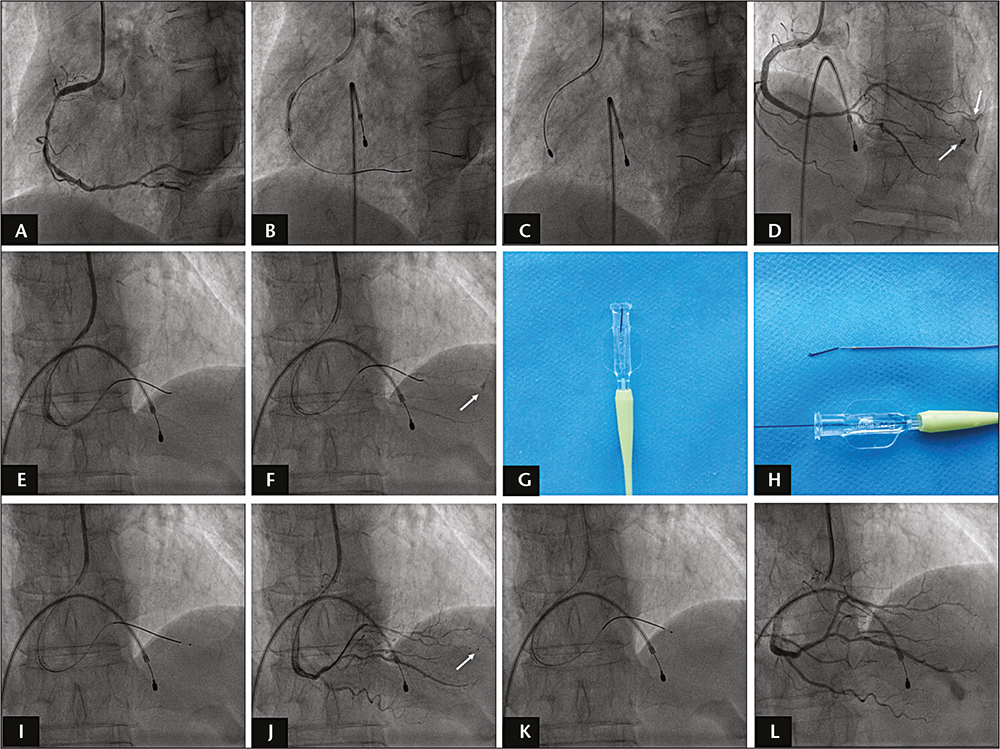
Figure 1. (A) Coronary angiography showed a long, heavily calcified and critical stenosis in the middle segment of the right coronary artery. (B) A 2.5 x 15-mm noncompliant balloon was dilated to 20 atm with a severe “dog-boning” effect at the lesion site. (C) Rotational atherectomy was performed. (D) Two distal coronary perforations (white arrows) were found after revascularization. (E) A small balloon was inflated to seal the perforations. (F) Repeat coronary angiography showed one of the perforations was closed, but the other perforation persisted (white arrow). (G) A piece of 3-0 silk suture was prepared and placed vertically into the tail of the microcatheter. (H) The silk suture was pushed into the vessel slowly using the guidewire. (I) The first sealing with silk suture was performed. (J) Angiography demonstrated the perforation became smaller after the silk suture sealing (white arrow). (K) Further sealing was performed again in the same fashion. (L) Repeat angiography demonstrated that the perforation was closed completely.
… coronary angiography conducted after postdilation revealed leakage of contrast media from two different distal small vessels corresponding to Ellis grade II and Ellis grade III coronary perforation…
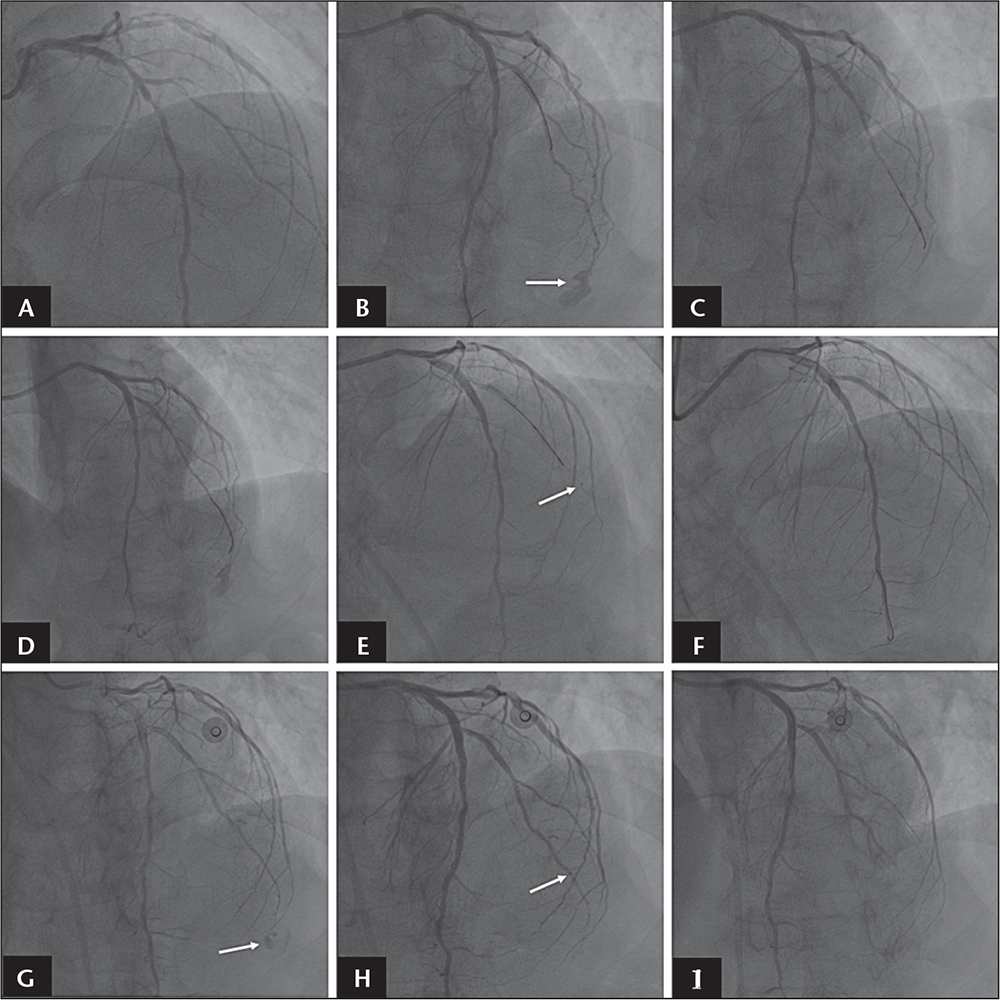
Figure 2. (A) Coronary angiography showed critical stenosis in the left anterior descending artery and its first diagonal branch (D1). (B) After target lesion revascularization, repeat coronary angiography revealed an Ellis grade III perforation at the distal end of D1 (white arrow). (C) Prolonged balloon inflation was performed to try to seal the perforation. (D) Two prolonged balloon inflations failed to seal the perforation. (E) Intracoronary thrombin injection via a microcatheter was performed to close the perforation (white arrow indicates the tip of the microcatheter). (F) After two injections of thrombin, the perforation was repaired. (G) Angiography the next day revealed leakage of contrast media from the distal perforation site of D1 (white arrow indicates the perforation). (H) A silk suture embolization technique was conducted to seal the perforation (white arrow indicates the tip of the microcatheter). (I) Successful closure of the perforation was achieved.
… two prolonged balloon inflations failed to seal the perforation.
The advantages of using silk suture as an embolization material include the possibility of use at any time, short preparation time, low cost, and the absence of immunoreaction.
Main Points
• Coronary artery perforation (CAP) is a rare but potentially life-threatening complication that may cause cardiac tamponade during percutaneous coronary intervention (PCI). Guidewire-induced perforation appears to be the most frequent cause of CAP.
• Prolonged balloon inflation and reversal of anticoagulation with protamine sulfate are generally used to seal the distal CAP. If the prolonged balloon inflation cannot stop the leakage, the most common methods are embolization of the vessel with use of metal coils, gel foam, thrombin, or other embolic materials. However, each of these procedures has limitations.
• The advantages of using silk suture as an embolization material include the possibility of use at any time, short preparation time, low cost, and the absence of immunoreaction. The silk suture can be easily advanced to the perforation site through a microcatheter with a guidewire rather than by injection with a syringe, thus avoiding the risk of perforation extension.
• This technique may also provide an optimal method for sealing the collateral perforations during retrograde chronic total occlusion PCI.
Main Points
• Coronary artery perforation (CAP) is a rare but potentially life-threatening complication that may cause cardiac tamponade during percutaneous coronary intervention (PCI). Guidewire-induced perforation appears to be the most frequent cause of CAP.
• Prolonged balloon inflation and reversal of anticoagulation with protamine sulfate are generally used to seal the distal CAP. If the prolonged balloon inflation cannot stop the leakage, the most common methods are embolization of the vessel with use of metal coils, gel foam, thrombin, or other embolic materials. However, each of these procedures has limitations.
• The advantages of using silk suture as an embolization material include the possibility of use at any time, short preparation time, low cost, and the absence of immunoreaction. The silk suture can be easily advanced to the perforation site through a microcatheter with a guidewire rather than by injection with a syringe, thus avoiding the risk of perforation extension.
• This technique may also provide an optimal method for sealing the collateral perforations during retrograde chronic total occlusion PCI.
Coronary artery perforation (CAP) is a rare (0.1%-3.0% of the general interventional population) but potentially life-threatening complication that may cause cardiac tamponade during percutaneous coronary intervention (PCI).1 Guidewire-induced perforation appears to be the most frequent cause of CAP,1 and approximately 36% of guidewire-induced perforations occur in distal coronary arteries.2 This case study reports, for the first time, two cases of successful closure of guidewire-induced distal CAP with silk suture embolization.
Case Report
Case 1
A 61-year-old woman presented with typical angina during exercise for a 6-month period. Elective coronary angiography showed a long, heavily calcified, and critical stenosis in the middle segment of the right coronary artery (RCA) (Figure 1A) and nonsignificant lesions in the left coronary system. A 6-Fr Judkins left 3.5 guiding catheter (Terumo, Tokyo, Japan) was advanced to the RCA ostium via routine right radial access. Two Runthrough NS™ guidewires (Terumo) were passed through the lesion and placed into the distal branch, respectively. A 2.5 × 15-mm noncom-pliant balloon was dilated to 20 atm, with a severe “dog-boning” effect at the lesion site (Figure 1B). We performed rotational atherectomy using 1.5-mm and 1.75-mm burrs of a Rotablator™ device (Boston Scientific, Marlborough, MA) (Figure 1C). The lesion was fully predilated with the same balloon, and then implanted with Excel™ 2.75 mm × 28 mm (Jiwei, Weihai, China) and Nano™ 3.0 mm × 15 mm (Lepu, Beijing, China) drug-eluting stents. Postdilatation was performed using a Sapphire™ NC 3.0 mm × 12 mm balloon (OrbusNeich, Wanchai, Hong Kong) at 18 to 20 atm. However, coronary angiography conducted after postdilation revealed leakage of contrast media from two different distal small vessels corresponding to Ellis grade II and Ellis grade III coronary perforation (contrast extravasation into the left ventricle), respectively (Figure 1D). A Ryujin™ 1.5 × 15-mm balloon (Terumo) was advanced to the distal posterior left ventricular branch and inflated to 3 atm for 30 minutes to seal the perforations (Figure 1E). Repeat coronary angiography revealed that the Ellis grade III perforation was closed, but the Ellis grade II perforation persisted (Figure 1F). A Finecross™ microcatheter (Terumo) was advanced over a Runthrough NS guidewire into the vessel with the coronary perforation. A piece of 3-0 silk suture (∼ 10 mm in length) was prepared and placed vertically into the tail of the microcatheter (Figure 1G), and was then pushed into the vessel slowly using the guidewire (Figure 1H). After the first sealing (Figure 1I), angiography demonstrated a minimal but persistent leak (Figure 1J); further sealing was performed (Figure 1K). The microcatheter was then withdrawn, and repeat angiography demonstrated that the perforation was closed completely (Figure 1L). The patient tolerated the procedure very well and returned in a stable condition to the ward. The patient recovered successfully and was discharged from the hospital 3 days later.
Case 2
A 74-year-old man presented with a 7-year history of stable angina. Elective coronary angiography showed critical stenosis in the proximal and mid portion of the left anterior descending artery (LAD) and in the mid segment of the first diagonal branch (Dl) (Figure 2A), and nonsignificant lesions in the RCA. Stenting of the target lesion was performed after balloon predilata-tion. An Excel 2.5 mm × 18-mm drug-eluting stent was implanted in the mid segment of the Dl, and Firebird2™ 2.75 mm × 18-mm (MicroPort Medical, Shanghai, China) and Firebird2 3.0 mm × 23-mm drug-eluting stents were deployed from the mid to the proximal LAD. However, coronary angiography showed an extravasation of contrast media from the distal site of the Dl corresponding to Ellis grade III coronary perforation (contrast extravasation into the pericardium) (Figure 2B). A 2.0-mm diameter balloon was immediately advanced to the distal D1 and inflated to 3 atm for 30 minutes to seal the perforation (Figure 2C); this was combined with intravenous protamine administration (60 mg). However, two prolonged balloon inflations failed to seal the perforation (Figure 2D). Echocardiographic examination revealed a moderate pericardial effusion; therefore, percutaneous pericardial drainage was performed. Intracoronary thrombin injections (200 U of thrombin solution were injected each time) via a Finecross microcatheter into the distal Dl after inflating the balloon proximally to the perforation site (Figure 2E). After two injections, the perforation was successfully repaired (Figure 2F). Serial angiography over the next 30 minutes demonstrated no further contrast extravasation. The patient returned to the ward in a stable condition. However, bloody pericardial fluid was still draining out after 12 hours. Repeat coronary angiography showed persistent contrast media extravasation from the distal perforation site of the D1 (Figure 2G). We used a silk suture embolization technique to seal the perforation (Figure 2H). The successful closure of the perforation was achieved in a similar fashion to that described in Case 1, above, and serial angiography over the subsequent 30 minutes confirmed no further contrast extravasation (Figure 2I). Serial echocardiography showed no further reaccumulation of pericardial fluid, and the pericardial drainage catheter was withdrawn 10 hours later. The patient recovered successfully and was discharged from the hospital 3 days later without pericardial effusion.
Discussion
CAP is a rare but potentially fatal complication of PCI that can result in life-threatening cardiac tampon-ade.1 In the contemporary interventional era, guidewire-induced perforations cause the majority of CAPs1; approximately 36% of the guidewire-induced perforations occur in distal coronary arteries,2 which sometimes progress to cardiac tamponade even without contrast extravasations during the procedure.3 Perforations can be attributed not only to stiff or hydrophilic guidewires, but also to workhorse wires such as the Balance (Abbott Vascular, Abbott Park, IL) and BMW (Abbott Vascular), especially when placed in a small distal branch.3
Prolonged balloon inflation and reversal of anticoagulation with protamine sulfate are generally used to seal the distal CAP. If the prolonged balloon inflation cannot stop the leakage, as was the case in our two patients, the most common methods are embolization of the vessel with use of metal coils, gel foam, thrombin, or other embolic materials, such as autologous blood clot, collagen, or subcutaneous tissues, as was reviewed by Al-Mukhaini and colleagues.4 However, each of the above procedures has its own limitations. For example, the cost of microcoils is higher, whereas the preparation time of autologous blood clot is longer. Histologic examination has revealed that both absorbable gelatin sponge and microcoil embolization can cause foreign body granulomatous change.5 Moreover, these embolic materials are primarily injected into the distal coronary artery with a syringe via a microcatheter, which may increase the risk of perforation expansion or rupture. Another hindrance in the use of the above-metioned procedures is lack of operator expertise, as they involve complex hardware and maneuvers.
We describe a novel method of sealing distal CAP using silk suture. The advantages of using silk suture as an embolization material include the possibility of use at any time, short preparation time, low cost, and the absence of immunoreaction. The silk suture can be easily pushed to the site of perforation through a microcatheter with a guidewire instead of by injection with a syringe, avoiding the risk of perforation extension. Recent meta-analysis showed there was a higher rate (6.9%) of collateral perforation in retrograde coronary chronic total occlusions (CTO) PCI6; our present technique may also provide an optimal method for sealing the collateral perforations during retrograde CTO PCI.
Conclusions
We describe the treatment of distal coronary perforations using localized silk suture embolization with a microcatheter. This technique appears to be safe, simple, and effective for the treatment of distal CAPs resulting from PCI. ![]()
The authors report no real or apparent conflicts of interest.
References
- Shimony A, Zahger D, Van Straten M, et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol. 2009;104:1674-1677.
- Fukutomi T, Suzuki T, Popma JJ, et al. Early and late clinical outcomes following coronary perforation in patients undergoing percutaneous coronary intervention. Circ J. 2002;66:349-356.
- Stathopoulos IA, Kossidas K, Garratt KN. Delayed perforation after percutaneous coronary intervention: rare and potentially lethal. Catheter Cardiovasc Interv. 2014;83:E45-E50.
- Al-Mukhaini M, Panduranga P, Sulaiman K, et al. Coronary perforation and covered stents: an update and review. Heart Views. 2011;12:63-70.
- Kawano H, Arakawa S, Satoh O, et al. Foreign body granulomatous change from absorbable gelatin sponge and microcoil embolization after a guide wire-induced perforation in the distal coronary artery. Intern Med. 2010;49:1871-1874.
- El Sabbagh A, Patel VG, Jeroudi OM, et al. Angiographic success and procedural complications in patients undergoing retrograde percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 3,482 patients from 26 studies. Int J Cardiol. 2014;174:243-248.