Reassessing the Importance of Complete Versus Incomplete Coronary Revascularization
Dean J. Kereiakes, MD, FACC, FSCAI
The Lindner Research Center, The Christ Hospital Heart and Vascular Center, Cincinnati, OH
Coronary revascularization may be performed for relief of anginal symptoms or, in specific patient subgroups, to reduce the incidence of myocardial infarction and mortality. Achieving complete revascularization of all significantly obstructed coronary segments has been an established goal of coronary bypass graft surgery (CABG) and more recent data demonstrate a salutary effect of complete revascularization following percutaneous coronary intervention (PCI) on long-term clinical outcomes as well. Incomplete coronary revascularization is associated with increased mortality following both CABG and PCI, as well as with an increased incidence of myocardial infarction, repeat revascularization, and major adverse cardiovascular or cerebrovascular events following PCI. The relationship between completeness of revascularization and late adverse clinical outcomes is both qualitative and quantitative as reflected by the residual SYNTAX score (angiographic lesion complexity) following PCI. Thus, complete revascularization has evolved as an important objective for either CABG or PCI and the ability to achieve complete revascularization should enter into the decision algorithm for choice of revascularization modality.
[Rev Cardiovasc Med. 2014;15(1):24-30 doi: 10.3909/ricm0714]
© 2014 MedReviews®, LLC
Reassessing the Importance of Complete Versus Incomplete Coronary Revascularization
Dean J. Kereiakes, MD, FACC, FSCAI
The Lindner Research Center, The Christ Hospital Heart and Vascular Center, Cincinnati, OH
Coronary revascularization may be performed for relief of anginal symptoms or, in specific patient subgroups, to reduce the incidence of myocardial infarction and mortality. Achieving complete revascularization of all significantly obstructed coronary segments has been an established goal of coronary bypass graft surgery (CABG) and more recent data demonstrate a salutary effect of complete revascularization following percutaneous coronary intervention (PCI) on long-term clinical outcomes as well. Incomplete coronary revascularization is associated with increased mortality following both CABG and PCI, as well as with an increased incidence of myocardial infarction, repeat revascularization, and major adverse cardiovascular or cerebrovascular events following PCI. The relationship between completeness of revascularization and late adverse clinical outcomes is both qualitative and quantitative as reflected by the residual SYNTAX score (angiographic lesion complexity) following PCI. Thus, complete revascularization has evolved as an important objective for either CABG or PCI and the ability to achieve complete revascularization should enter into the decision algorithm for choice of revascularization modality.
[Rev Cardiovasc Med. 2014;15(1):24-30 doi: 10.3909/ricm0714]
© 2014 MedReviews®, LLC
Reassessing the Importance of Complete Versus Incomplete Coronary Revascularization
Dean J. Kereiakes, MD, FACC, FSCAI
The Lindner Research Center, The Christ Hospital Heart and Vascular Center, Cincinnati, OH
Coronary revascularization may be performed for relief of anginal symptoms or, in specific patient subgroups, to reduce the incidence of myocardial infarction and mortality. Achieving complete revascularization of all significantly obstructed coronary segments has been an established goal of coronary bypass graft surgery (CABG) and more recent data demonstrate a salutary effect of complete revascularization following percutaneous coronary intervention (PCI) on long-term clinical outcomes as well. Incomplete coronary revascularization is associated with increased mortality following both CABG and PCI, as well as with an increased incidence of myocardial infarction, repeat revascularization, and major adverse cardiovascular or cerebrovascular events following PCI. The relationship between completeness of revascularization and late adverse clinical outcomes is both qualitative and quantitative as reflected by the residual SYNTAX score (angiographic lesion complexity) following PCI. Thus, complete revascularization has evolved as an important objective for either CABG or PCI and the ability to achieve complete revascularization should enter into the decision algorithm for choice of revascularization modality.
[Rev Cardiovasc Med. 2014;15(1):24-30 doi: 10.3909/ricm0714]
© 2014 MedReviews®, LLC
KEY WORDS
Coronary revascularization • Incomplete revascularization • SYNTAX score
KEY WORDS
Coronary revascularization • Incomplete revascularization • SYNTAX score
The SYNTAX score has been validated and employed in a tertile distribution to describe relative risk for death, MI, stroke, and requirement for repeat revascularization following PCI.
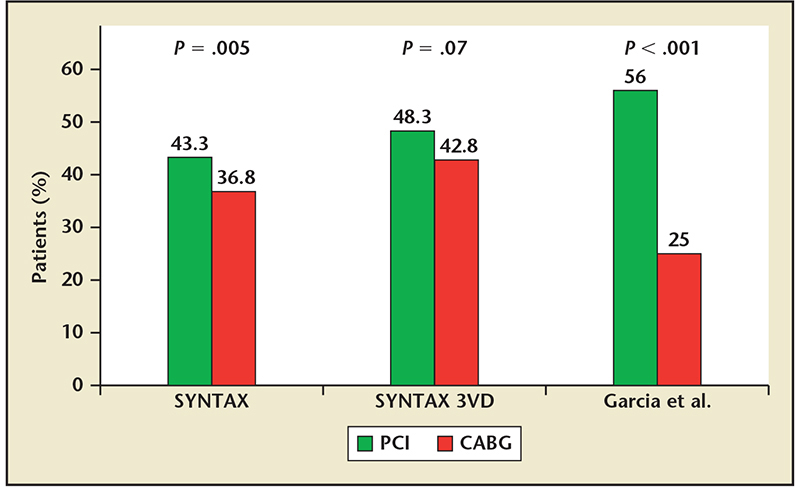
Figure 1. Incidence of incomplete revascularization by modality for the overall SYNTAX trial, SYNTAX 3 vessel disease (3VD) cohort only and from the meta-analysis reported by Garcia et al. Incomplete revascularization is more common following percutaneous coronary intervention (PCI) compared with coronary artery bypass graft (CABG) surgery. Adapted from Garcia S et al.7
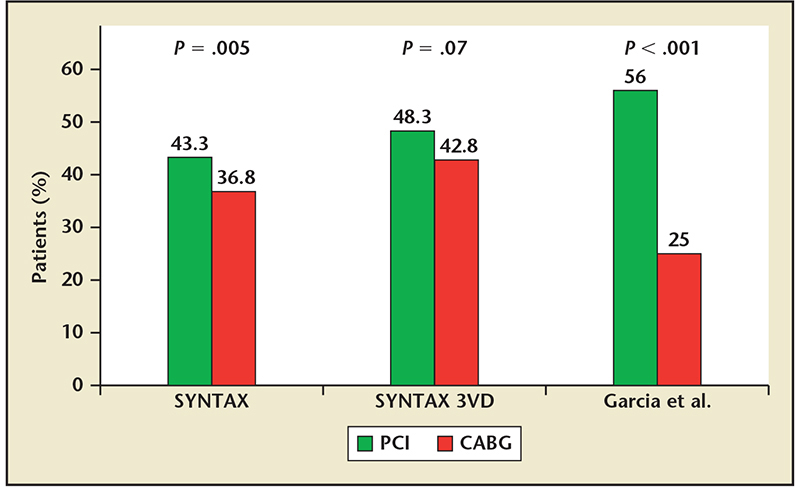
Figure 1. Incidence of incomplete revascularization by modality for the overall SYNTAX trial, SYNTAX 3 vessel disease (3VD) cohort only and from the meta-analysis reported by Garcia et al. Incomplete revascularization is more common following percutaneous coronary intervention (PCI) compared with coronary artery bypass graft (CABG) surgery. Adapted from Garcia S et al.7
… CR has been associated with significant reductions in long-term mortality, MI, and repeat revascularization procedures.
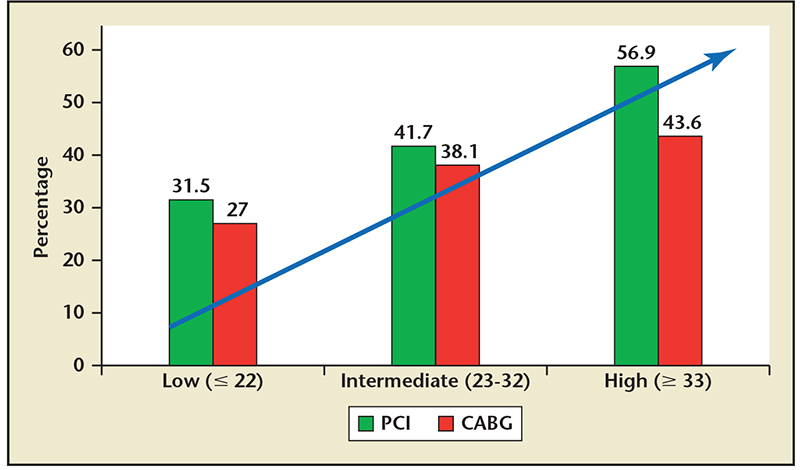
Figure 2. Incidence of incomplete revascularization by modality and tertile of baseline SYNTAX score in the SYNTAX trial. Incomplete revascularization increased in proportion to baseline angiographic complexity and a disproportionate relative increase is observed following percutaneous coronary intervention. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention. Adapted from Head SJ et al.17
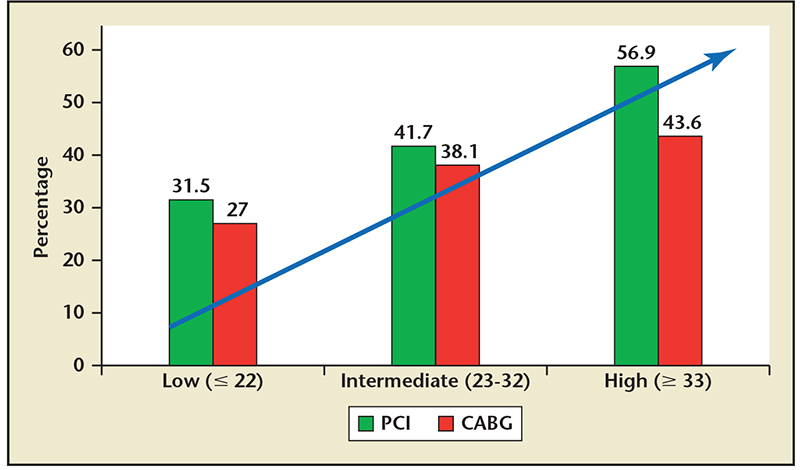
Figure 2. Incidence of incomplete revascularization by modality and tertile of baseline SYNTAX score in the SYNTAX trial. Incomplete revascularization increased in proportion to baseline angiographic complexity and a disproportionate relative increase is observed following percutaneous coronary intervention. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention. Adapted from Head SJ et al.17

Figure 3. Residual SYNTAX score predicts all-cause mortality following percutaneous coronary intervention regardless of baseline SYNTAX score tertile. Reprinted with permission from Farooq V et al.12
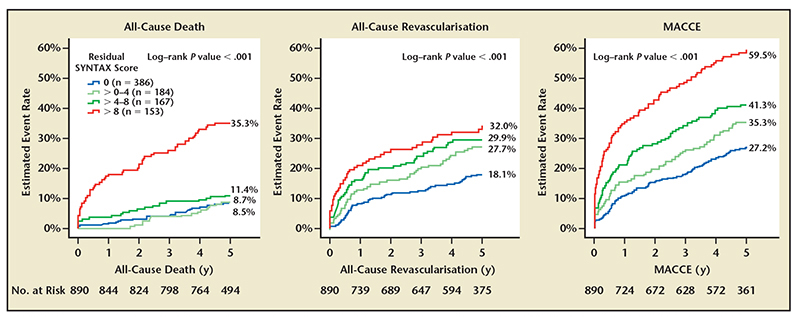
Figure 4. All-cause death, revascularization and major adverse cardiovascular and cerebrovascular events (MACCE) by tertile of residual SYNTAX score following percutaneous coronary intervention in the SYNTAX trial. Reprinted with permission from Farooq V et al.12


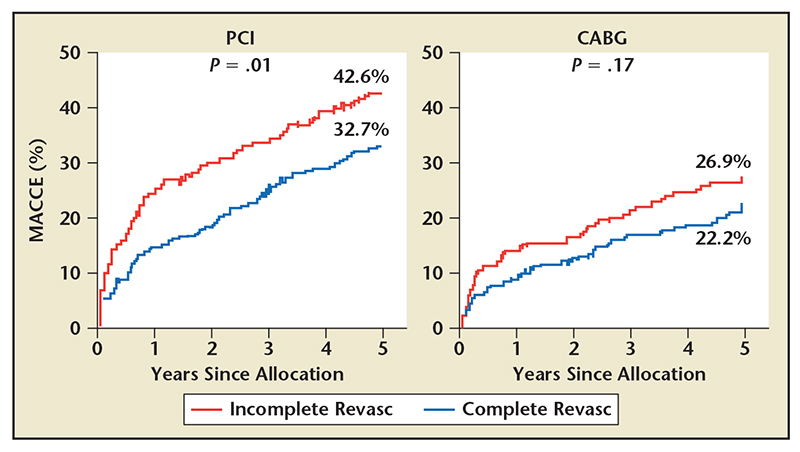
Figure 5. Major adverse cardiovascular and cerebrovascular events (MACCE) by revascularization modality and completeness of revascularization through 5-year follow-up in the SYNTAX trial. Incomplete revascularization following PCI is associated with a disproportionate increase in MACCE over time. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention. Data on file, Boston Scientific, Natick, MA.
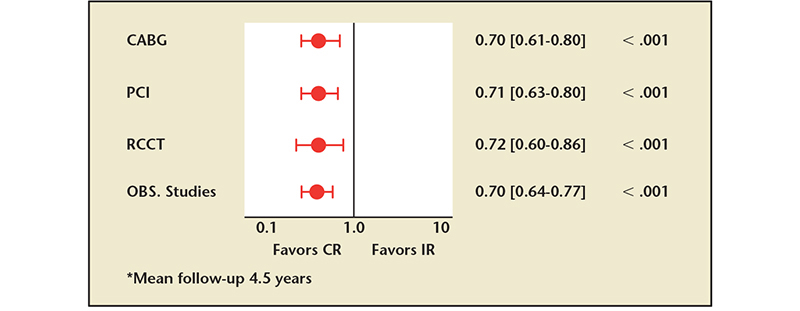
Figure 6. Completeness of revascularization and all-cause mortality through 4.5 years (mean) follow-up. By revascularization modality (CABG, PCI) and by study type (RCCT, OBS) as demonstrated in a meta-analysis of 35 studies involving 89,833 revascularized patients. Incomplete revascularization is associated with a similar mortality hazard regardless of modality or study type. CABG, coronary artery bypass graft; CR, complete revascularization; IR, incomplete revascularization; OBS, observational; PCI, percutaneous coronary intervention; RCCT, randomized controlled clinical trials. Adapted with permission from Garcia S et al.7
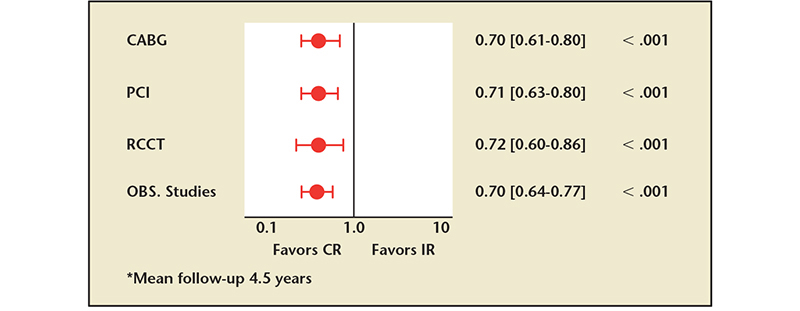
Figure 6. Completeness of revascularization and all-cause mortality through 4.5 years (mean) follow-up. By revascularization modality (CABG, PCI) and by study type (RCCT, OBS) as demonstrated in a meta-analysis of 35 studies involving 89,833 revascularized patients. Incomplete revascularization is associated with a similar mortality hazard regardless of modality or study type. CABG, coronary artery bypass graft; CR, complete revascularization; IR, incomplete revascularization; OBS, observational; PCI, percutaneous coronary intervention; RCCT, randomized controlled clinical trials. Adapted with permission from Garcia S et al.7
… the degree of revascularization completeness may not be as important in reducing MI or repeat procedures following CABG as long as the three major epicardial vessels are grafted.
Main Points
• Coronary revascularization may be performed for relief of anginal symptoms or to reduce the incidence of myocardial infarction and mortality. Achieving complete revascularization (CR) of all significantly obstructed coronary segments has been an established goal of coronary bypass graft surgery (CABG) and more recent data demonstrate a salutary effect of CR following percutaneous coronary intervention (PCI).
• CR following PCI is associated with significant improvement in important clinical outcomes, including survival, as well as reductions in the incidence of myocardial infarction and requirement for repeat revascularization procedures.
• CR should be the objective of revascularization for multivessel coronary artery disease, and the likelihood of achieving CR should inform the choice of revascularization modality (CABG vs PCI).
• Residual SYNTAX score provides a standardized, graded quantification of incomplete revascularization, and has been correlated with adverse clinical events, including mortality following PCI in patients presenting with acute coronary syndrome, multivessel stable ischemic heart disease, and unprotected left main coronary artery disease.
Main Points
• Coronary revascularization may be performed for relief of anginal symptoms or to reduce the incidence of myocardial infarction and mortality. Achieving complete revascularization (CR) of all significantly obstructed coronary segments has been an established goal of coronary bypass graft surgery (CABG) and more recent data demonstrate a salutary effect of CR following percutaneous coronary intervention (PCI).
• CR following PCI is associated with significant improvement in important clinical outcomes, including survival, as well as reductions in the incidence of myocardial infarction and requirement for repeat revascularization procedures.
• CR should be the objective of revascularization for multivessel coronary artery disease, and the likelihood of achieving CR should inform the choice of revascularization modality (CABG vs PCI).
• Residual SYNTAX score provides a standardized, graded quantification of incomplete revascularization, and has been correlated with adverse clinical events, including mortality following PCI in patients presenting with acute coronary syndrome, multivessel stable ischemic heart disease, and unprotected left main coronary artery disease.
Coronary revascularization may be performed for relief of angina symptoms and, in specific patient subgroups, to reduce the incidence of myocardial infarction (MI) and long-term mortality. Current US and European clinical practice guidelines recommend coronary bypass graft surgery (CABG) over percutaneous coronary intervention (PCI) for the treatment of multivessel coronary artery disease (MVCAD) and confer a class IIb (of uncertain benefit) recommendation to PCI for improvement in survival.1-3 Prior studies suggest that the magnitude of clinical benefit attributable to coronary revascularization is, at least in part, proportional to the completeness of revascularization achieved by either CABG or PCI.4-6 Although these studies suggest that incomplete revascularization (IR) is associated with persistent hazard for death, MI, or additional revascularization procedures, they are limited by their observational and retrospective study designs, lack of randomization, and reliance on the ascertainment of revascularization completeness by the treating physician. Furthermore, the lack of a uniform definition for complete revascularization (CR) or accepted metrics to quantify both the presence and magnitude of IR have contributed to conflicting reports on the clinical importance of complete revascularization from observational studies, and no large-scale randomized clinical trial has yet tested the hypothesis for superiority of CR (vs IR). In the context of recent information it is appropriate to review what is currently known regarding completeness of coronary revascularization, its impact on clinical outcomes, and its utility in the therapeutic decision algorithm for choosing an optimal revascularization strategy.
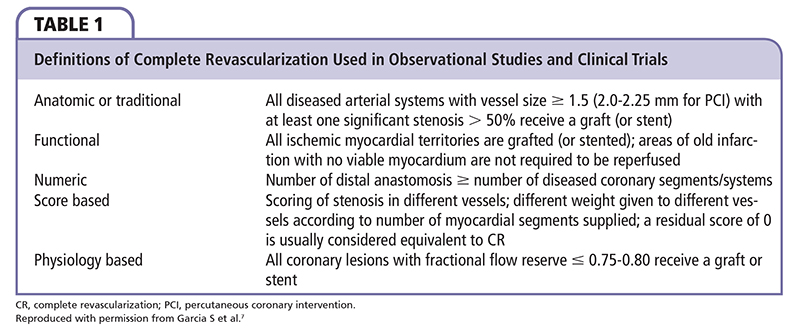
The Challenge of Definition
Numerous definitions have been used to describe the completeness of coronary revascularization and have included anatomic, functional, numerical, score-based, and physiology-based criteria (Table 1). These definitions vary with respect to target vessel size, target stenosis location, and the presence or absence of objectively documented ischemia. Although a recent large-scale meta-analysis7 demonstrated a differential, salutary effect of CR (vs IR) on survival (following PCI or CABG), as well as MI and repeat revascularization (following PCI) regardless of the definition (anatomic vs physiologic) for CR employed, much focus has currently been directed toward more accurate descriptive quantification regarding not only the presence, but also the magnitude of revascularization completeness. In this regard, the residual SYNTAX score appears to provide a standardized, graded quantification of IR and has been correlated with adverse clinical events, including mortality following PCI in patients presenting with acute coronary syndrome,8 multivessel stable is-chemic heart disease,9 and unprotected left main coronary artery disease (CAD).10 The baseline (pre-PCI) SYNTAX score, which describes angiographic lesion complexity using 12 readily available angiographic variables, has been correlated with the occurrence of major adverse cardiovascular and cerebrovascular events (MACCE) in follow-up through 5 years after PCI but not CABG,11 and has been incorporated into clinical practice guideline recommendations for selection of revascularization strategy. The SYNTAX score has been validated and employed in a tertile distribution to describe relative risk for death, MI, stroke, and requirement for repeat revascularization following PCI.8,12,13 More recently, both the residual SYNTAX score (calculated after PCI) and the ▵ SYNTAX score (difference between pre- and post-PCI scores) have been evaluated for prognostic discriminatory ability following PCI.8,12 Despite demonstrated colinearity of the baseline and residual SYNTAX scores,8,10,12 the residual SYNTAX score provides significant incremental predictive accuracy for late adverse clinical outcomes and appears to perform best when applied in a graded (tertile) quantitative fashion. Thus, the residual SYNTAX score appears to be the best currently available and validated descriptor of residual atherosclerotic burden following PCI revascularization. More recently, a universal definition of IR that integrates anatomic (coronary angiography) and physiologic (fractional flow reserve [FFR]) data has been proposed.14 This definition of IR is based on the inability to treat coronary segments with stenoses ≥ 50% to 70% severity with an FFR ≤ 0.80, or stenoses > 70% without FFR assessment, that supply a significant region of viable myocardium. Although the baseline SYNTAX score has relatively poor prognostic capacity after CABG revascularization, investigations are currently underway to determine the discriminatory predictive capacity of the residual SYNTAX score following CABG.
The Importance of Complete Revascularization
Recent randomized studies and meta-analyses suggest that CR is more often achieved with CABG than PCI (Figure 1).7,15,16 Furthermore, CR has been associated with significant reductions in long-term mortality, MI, and repeat revascularization procedures. Although the association between CR and reduced risk for cardiovascular events may be causal, through reduction or elimination of ischemia, important covariate imbalances exist between the CR and IR groups that have been compared based on the various determinants of IR, as well as the lack of randomized assignment to CR versus IR. Indeed, IR was more frequent in PCI-treated patients with chronic total coronary occlusion, bifurcation stenoses, and diffuse or small vessel coronary disease.17 Similarly, unstable angina presentation, diffuse or small vessel disease, and the total number of target coronary stenoses predicted IR following CABG.17 Thus, IR may be a surrogate marker for a greater baseline ischemic burden and more advanced CAD, which is less amenable to revascularization by either PCI or CABG. Although the baseline SYNTAX score prior to revascularization appears to be proportional to the likelihood of IR (Figure 2) following both PCI or CABG, this relationship is more marked for PCI.17 Indeed, for patients in the lowest tertile of baseline SYNTAX scores (≤ 22) rates of IR were similar for PCI and CABG (31% vs 27%, respectively). Conversely, patients in the highest tertile of SYNTAX scores (≥ 33) had a disproportionate increase in IR following PCI (57%) versus CABG (44%). Thus, both the incidence of IR and the relative advantage of CABG (vs PCI) for achieving CR are directly proportional to the complexity of CAD as reflected by baseline SYNTAX score tertile.
The Consequences of Incomplete Revascularization
IR by PCI is a powerful predictor of death or MI in follow-up even in the absence of a chronic total coronary occlusion.4,12,13,18 Similarly, IR by PCI has been correlated with an increased incidence of MI, repeat revascularization, and MACCE. Although IR has been analyzed using a binary (0 vs > 0) definition for residual SYNTAX score, further quantification as a tertile function appears to provide greater discriminatory accuracy. Using a residual score of 0 as the referent, increasing tertiles of residual SYNTAX score (> 0-4, > 4-8, and > 8) provided incremental predictive accuracy for all-cause death regardless of the baseline SYNTAX score tertile (Figure 3).12 In addition, a graded and direct relationship of residual SYNTAX score tertile was observed for the occurrence of all-cause revascularization and MACCE through 5-year follow-up after PCI (Figure 4). This relationship must be viewed in context and tempered by the highly significant trends in the complexity of both clinical and angiographic covariates by tertile of residual SYNTAX score (Table 2).
In the SYNTAX trial, MACCE through 5-year follow-up was statistically significantly increased following IR by PCI but not CABG (Figure 5). This observation suggests a differential impact of IR on clinical outcomes for PCI (vs CABG). As noted previously, both the incidence of IR following PCI, as well as the relative advantage of CABG over PCI for achieving CR, is proportional to coronary disease complexity as reflected by baseline SYNTAX score tertile. Those patients in the highest tertile of baseline SYNTAX scores have a disproportionate increase in the incidence of IR following PCI when compared with patients in the lowest tertile of SYNTAX scores. Although the comparable rates of IR following CABG were 44% and 27% (highest and lowest SYNTAX score tertiles, respectively), the incidence of MACCE to 5 years following CABG was similar for patients in both the lowest and highest SYNTAX score tertiles (26.8% and 24.1%, respectively) but was not similar following PCI (33.3% vs 41.9%, respectively). The relative and disproportionate contribution of IR following PCI (vs CABG) to the incremental incidence of MACCE across tertiles of SYNTAX score cannot be determined definitively but is no doubt a major contributor to the differential between PCI and CABG outcomes in patients with the most complex CAD. Thus, this difference in completeness of revascularization achieved by PCI (vs CABG) and the relative disproportionate weight of adverse events attributable to IR following PCI may, at least in part, contribute to the relative survival advantage attributed to CABG (vs PCI) in both randomized clinical trials of revascularization for MVCAD11,16 as well as observational studies.19 This disproportionate impact of IR (vs CR) for outcomes following PCI more so than CABG is supported by a recent meta-analysis of 35 studies involving 89,833 revascularized patients (of whom 50.5% achieved CR), which concluded that among patients treated with CABG, CR was not associated with a reduction in either MI (risk ratio [RR] 0.69; 95% confidence interval [CI], 0.44-1.10; P = .12) or repeat revascularization (RR 0.92; 95% CI, 0.67-1.28; P = .64) procedures.7 This observation suggests that the degree of revascularization completeness may not be as important in reducing MI or repeat procedures following CABG as long as the three major epicardial vessels are grafted. Conversely, a confounding effect due to the small number of studies which reported these specific outcomes following CABG could not be excluded. Importantly, a reduction in both MI (RR 0.8; 95% CI, 0.71-0.91; P = .001) and the requirement for repeat revascularization (RR 0.74; 95% CI, 0.65-0.83; P < .0001) was observed following CR (vs IR) by PCI.7 Most interesting, however, is the finding of a mortality benefit associated with CR (vs IR) through 4.5-year (mean) follow-up of similar magnitude (∼30%) following either PCI or CABG (Figure 6). This observation suggests that the specific revascularization modality (PCI vs CABG) used may not be as important as the objective of achieving complete revascularization.
Conclusions
CR should be the objective of revascularization for MVCAD and the likelihood of achieving CR should inform the choice of revascularization modality (CABG vs PCI). CR (vs IR) following PCI is associated with significant improvement in important clinical outcomes including survival, as well as reductions in the incidence of MI and requirement for repeat revascularization procedures. CR (vs IR) following CABG confers a survival advantage, but is not convincingly associated with reductions in MI or repeat revascularization. As CR appears to confer a survival advantage following either PCI or CABG, objective assessment of the completeness of revascularization should be incorporated into procedural quality and performance metrics, as well as criteria for appropriate utilization. ![]()
References
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/ AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44-e164.
- Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501- 2555.
- Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949-3003.
- Hannan EL, Wu C, Walford G, et al. Incomplete revascularization in the era of drug-eluting stents: impact on adverse outcomes. JACC Cardiovasc Interv. 2009;2:17-25.
- Kim YH, Park DW, Lee JY, et al. Impact of angiographic complete revascularization after drug-eluting stent implantation or coronary artery bypass graft surgery for multivessel coronary artery disease. Circulation. 2011;123:2373-2381.
- Gao Z, Xu B, Yang YJ, et al. Long-term outcomes of complete versus incomplete revascularization after drug-eluting stent implantation in patients with multivessel coronary disease. Catheter Cardiovasc Interv. 2013;82:343-349.
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. 2013;62:1421-1431.
- Généreux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol. 2012;59: 2165-2174.
- Malkin CJ, George V, Ghobrial MS, et al. Residual SYNTAX score after PCI for triple vessel coronary artery disease: quantifying the adverse effect of incomplete revascularisation. EuroIntervention. 2013;8:1286-1295.
- Capodanno D, Chisari A, Giacoppo D, et al. Objectifying the impact of incomplete revascularization by repeat angiographic risk assessment with the residual SYNTAX score after left main coronary artery percutaneous coronary intervention. Catheter Cardiovasc Interv. 2013;82:333-340.
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629-638.
- Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128:141-151.
- Farooq V, Serruys PW, Garcia-Garcia HM, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61: 282-294.
- Gossl M, Faxon DP, Bell MR, et al. Complete versus incomplete revascularization with coronary artery bypass graft or percutaneous intervention in stable coronary artery disease. Circ Cardiovasc Interv. 2012;5:597-604.
- Serruys PW, Morice MC, Kappetein AP, et al; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360: 961-972.
- Farkouh ME, Domanski M, Sleeper LA, et al; FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375-2384.
- Head SJ, Mack MJ, Holmes DR Jr, et al. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur J Cardiothorac Surg. 2012;41:535-541.
- Rosner GF, Kirtane AJ, Genereux P, et al. Impact of the presence and extent of incomplete angiographic revascularization after percutaneous coronary intervention in acute coronary syndromes: the acute catheterization and urgent intervention triage strategy (ACUITY) trial. Circulation. 2012;125:2613-2620.
- Weintraub WS, Grau-Sepulveda MV, Weiss JM, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467-1476.