Director's Forum
Issues Facing Pharmacy Leaders in 2015: Suggestions for Pharmacy Strategic Planning
Robert J. Weber, PharmD, MS, BCPS, FASHP*
Director's Forum
Issues Facing Pharmacy Leaders in 2015: Suggestions for Pharmacy Strategic Planning
Robert J. Weber, PharmD, MS, BCPS, FASHP*
Director's Forum
Issues Facing Pharmacy Leaders in 2015: Suggestions for Pharmacy Strategic Planning
Robert J. Weber, PharmD, MS, BCPS, FASHP*
Issues facing pharmacy leaders in 2015 include practice model growth and the role of pharmacy students, clinical privileging of health-system pharmacists and provider status, medication error prevention, and specialty pharmacy services. The goal of this article is to provide practical approaches to 4 issues facing pharmacy leaders in 2015 to help them focus their department’s goals. This article will address (1) advances in the pharmacy practice model initiative and the role of pharmacy students, (2) the current thinking of pharmacists being granted clinical privileges in health systems, (3) updates on preventing harmful medication errors, and (4) the growth of specialty pharmacy services. The sample template of a strategic plan may be used by a pharmacy department in 2015 in an effort to continue developing patient-centered pharmacy services.
Issues facing pharmacy leaders in 2015 include practice model growth and the role of pharmacy students, clinical privileging of health-system pharmacists and provider status, medication error prevention, and specialty pharmacy services. The goal of this article is to provide practical approaches to 4 issues facing pharmacy leaders in 2015 to help them focus their department’s goals. This article will address (1) advances in the pharmacy practice model initiative and the role of pharmacy students, (2) the current thinking of pharmacists being granted clinical privileges in health systems, (3) updates on preventing harmful medication errors, and (4) the growth of specialty pharmacy services. The sample template of a strategic plan may be used by a pharmacy department in 2015 in an effort to continue developing patient-centered pharmacy services.
Issues facing pharmacy leaders in 2015 include practice model growth and the role of pharmacy students, clinical privileging of health-system pharmacists and provider status, medication error prevention, and specialty pharmacy services. The goal of this article is to provide practical approaches to 4 issues facing pharmacy leaders in 2015 to help them focus their department’s goals. This article will address (1) advances in the pharmacy practice model initiative and the role of pharmacy students, (2) the current thinking of pharmacists being granted clinical privileges in health systems, (3) updates on preventing harmful medication errors, and (4) the growth of specialty pharmacy services. The sample template of a strategic plan may be used by a pharmacy department in 2015 in an effort to continue developing patient-centered pharmacy services.
Hosp Pharm 2015;50(2):167–172
2015 © Thomas Land Publishers, Inc.
doi: 10.1310/hpj5002-167
The Patient Protection and Affordable Care Act (ACA) was fully enacted in 2014, with almost 20 million people obtaining health care coverage and uninsured Americans dropping from 18% to 13%.1 Medicaid coverage expansion is also required in patients with pre-existing conditions and requires the individual health insurance mandate.2 The increase in insured Americans will logically place more cost burden on an already costly system – with a major focus of most health care providers to ensure that care is of the highest quality with a minimum of cost. As pharmacy leaders, that means to “do more with less” by optimizing pharmacy practice models to focus on efficient medication distribution and effective monitoring of medication prescribing to prevent errors and unnecessary costs. The Ohio State University’s Wexner Medical Center sponsors a cost reduction and quality improvement campaign called Create the Future Now with the following slogan: Use less, Spend less, and Waste less.
Using a variety of strategic planning techniques (eg, SWOT [strengths, weakness, opportunities, and threats] analyses, environmental scans, etc) helps the pharmacy director set realistic and practical goals for the pharmacy. Strategic planning is critical for effective leadership in a department as it sets the “compass” for the direction of that department. However, to set these goals, the pharmacy director must understand the pertinent issues and prioritize these issues based on the impact they may have on the department’s progress and on how resources are allocated in a given year. Finally, key strategic goals that are directed yet simple will facilitate the buy-in and support from pharmacy staff, physicians, and the C-suite.
To determine issues affecting health-system pharmacy in 2015, I reviewed topics presented at professional society meetings; sought guidance from faculty in The Ohio State’s Colleges of Pharmacy, Medicine, and Public Health; and attended an educational session on the Pharmacy Forecast 2014-2018 at the American Society of Health-System Pharmacists (ASHP) Midyear Clinical Meeting in Anaheim, California, in December 2014.
Pharmacy Forecast 2014-2018 is published by the ASHP Research and Education Foundation’s Center for Health-System Pharmacy Leadership.3 This publication reviews a series of environmental scans in key areas affecting the growth of the pharmacy department. Examples of environmental scans include the areas of fiscal issues, quality and safety, pharmacy practice model, pharmacy operations, and ambulatory care. By reviewing this publication, a pharmacy director can become familiar with the important trends in health care and incorporate them into their strategic planning.
Based on the environmental scan, the issues for 2015 vary a bit from 2014; they focus on the areas of practice model growth and the role of pharmacy students, clinical privileging of health-system pharmacists and provider status, medication error prevention, and specialty pharmacy services. This article will address (1) advances in the pharmacy practice model initiative and the role of pharmacy students, (2) the current thinking of pharmacists being granted clinical privileges in health systems, (3) updates on preventing harmful medication errors, and (4) the growth of specialty pharmacy services. The information in this article may be used to develop a pharmacy department’s strategic plan for 2015 in an effort to continue providing patient-centered pharmacy services.
KEY ISSUES FACING PHARMACY LEADERS
ASHP’s Pharmacy Practice Model Initiative (PPMI) will continue to shape health-system pharmacy and drive innovations in pharmacy practice. Its goal is to expand pharmacy services through various initiatives such as broadening pharmacist roles across the continuum of care, optimizing the use of technology, and expanding technician responsibilities. These initiatives will require approaches that are in line with overall hospital goals, and they may entail changes to current state and national legislation.
Pharmacy Student Roles
A growing focus in the next year must be to continue to enhance the role of pharmacy students in the practice model. In 2009 and 2013, ASHP passed or expanded on policies that recognized the importance of pharmacy students in the practice model. Specifically ASHP supported re-engineering practice models to create accountable and integrated roles for students.4,5 Pharmacy schools rely on experiential programs that provide positive role models for students early in the curriculum and enhance their classroom learning. Leaders in this area include the Cleveland Clinic and the University of North Carolina, which have introduced the concept of the layered learner model (LLM) of pharmacy practice.
The LLM optimizes the role of advanced practice pharmacy experience (APPE) students during their final year of rotations.6 This model expands the ability of patients to receive individualized care from a pharmacy employee. Activities of pharmacy students in the LLM include documenting medication histories, screening for drug-related problems, providing patient education, performing medication reconciliation, and providing basic medication therapy management.
The Cleveland Clinic recently reported the results of their LLM, implemented in 2011.7 In one of their satellite hospitals, Cleveland Clinic Florida, the pharmacy leadership implemented the LLM and increased the number of APPE students from a baseline of 98 students in 2011 to 226 students in 2013. In addition, the hospital’s patient satisfaction scores on patients’ awareness of communication on medications rose from 58% to 70% over 18 months. During the same time period, the number of pharmacy interventions per patient increased (0.9 vs 1.4). The pharmacy department met all of the requirements by The Joint Commission related to medication reconciliation. Finally the participation of students in the discharge education program increased prescription capture of bedside-delivered medications by nearly 35%.
The Ohio State University Wexner Medical Center (OSUWMC) has set the goal to design the pharmacy student role as an integrated part of the pharmacy team. Working closely with staff and faculty from the College of Pharmacy, activities are being developed that involve students at every level of training in their pharmacy program. For example, students beginning their pharmacy schooling will participate in the following experiences at the medical center (introductory pharmacy practice experiences [IPPE]) under the supervision of a pharmacist: quality assurance checking of medications, medication packaging, emergency medication stocking, medication histories, and validating prescriptions. APPE activities will include medication reconciliation, anticoagulation management and education, participation in emergency responses, duplicate therapy monitoring, pharmacokinetic dosing, renal dose adjustments, and retail and specialty pharmacy activities.
Clinical Privileging and Credentialing
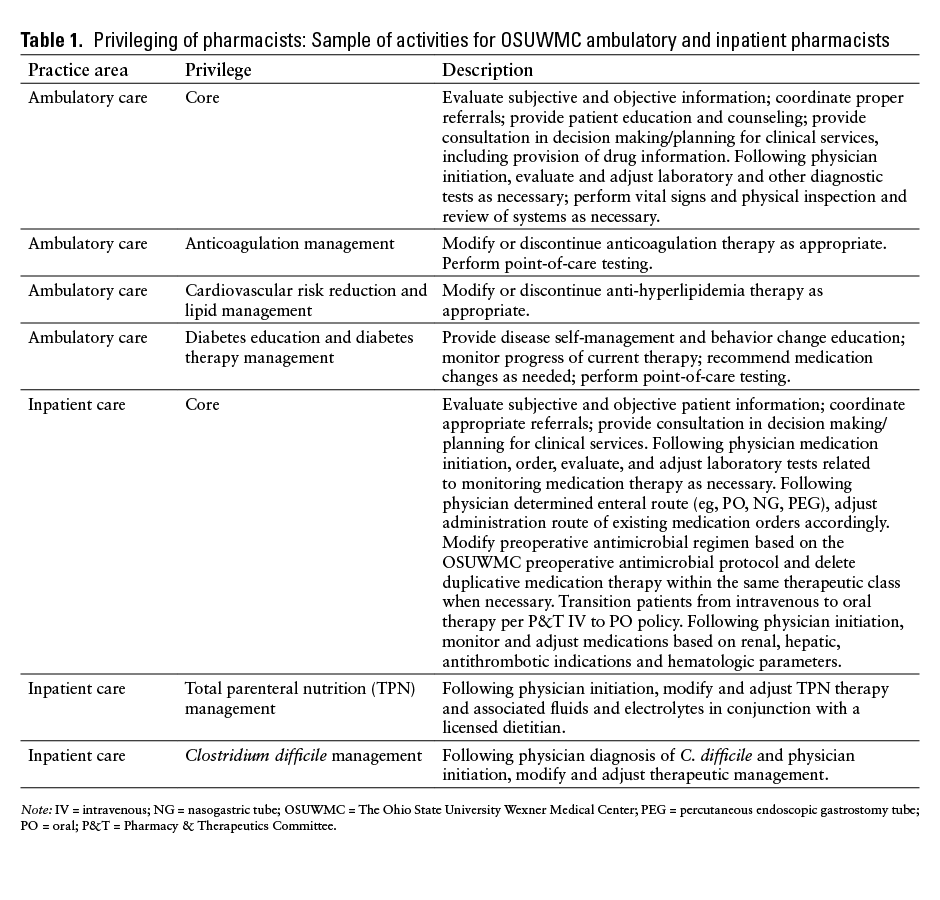
To address the issues of efficiency in patient care, OSUWMC began assigning clinical privileges to both acute care and ambulatory pharmacists. The department’s goal is to privilege all direct patient care pharmacists by the spring of 2015. Some privileged activities for the OSUWMC ambulatory and acute care pharmacy staff are listed in Table 1.
Founded in 1999, the Council on Credentialing in Pharmacy (CCP) is a coalition of 10 national pharmacy organizations committed to providing leadership, guidance, public information, and coordination for credentialing programs in or relevant to pharmacy.8 In 2010, the council defined credentialing as the process of granting and verifying pharmacists’ credentials. Examples of pharmacy credentials are the PharmD degree, state pharmacy license, residency certificate, and board of pharmacy specialties certification. Examples of pharmacy credentialing are the process of going to school, studying, and performing academically to earn a PharmD. Specific standards are set forth and must be met in order to receive a credential; for example, the American Council on Pharmacy Education (ACPE) sets standards for pharmacy education and ASHP sets standards for residency education.
Pharmacists may be granted additional clinical responsibilities beyond the previously expected functions of their job. Based on a proper credential, they may be authorized to provide clinical services within their scope of practice as a privilege of their employment – usually as members of a medical staff. Examples of privilege activities include dosing, monitoring, and adjusting vancomycin and aminogylcosides without physician verification. Physicians can delegate duties to pharmacists based on an approved protocol.9 It is important to note that these ways enhancing practice must be done within the scope of practice for the pharmacist’s license in a specific state. For example, pharmacists who are allowed the scope of managing anticoagulation cannot select the specific anticoagulant – that would be prescribing, which is prohibited by most state laws.
Multipronged Approach to Preventing Harmful Medication Errors
Preventing harm from medication errors is the goal of all medication safety programs. Continued focus on preventing harm from errors and sustaining gains in patient safety should continue to be strategic goals for any pharmacy department. OSUWMC used a multipronged approach to significantly reduce harmful medication errors. It used accepted harm scales to determine the impact of medication errors; between 2010 and 2011, harmful medication errors were tracked. These harmful errors involved drugs commonly known to cause harm, including insulin, antibiotics, anticoagulants, and opioids.
A needs assessment by OSUWMC leadership in response to these errors showed that no coordinated medication safety plan was approved by the hospital’s clinical and administrative leaders. In addition, there were insufficient resources for hiring pharmacists to focus on medication safety issues. Further error-preventing technology (barcode-assisted medication administration, IV infusion pump monitoring technology) was not implemented and the role of staff in medication error prevention was not clarified.
Strategic initiatives for medication safety were approved that dedicated 3 medication safety pharmacists to review and provide follow-up to errors involving anticoagulants, antibiotics, insulin, opioids, and sedative medications. An integrated electronic medical record (IHIS; Epic, Verona, Wisconsin) was implemented with barcode-assisted medication administration; medication error review teams were established on nursing units as part of their quality activities; and pharmacists’ activities were focused on medication reconciliation to prevent harmful medication errors.
These measures resulted in an increase in reported medication errors and a decrease in harmful errors from 2011 to 2013 (P < .001); a decrease in time to reported resolution of medication errors from 60 days in 2011 to less than 7 days in 2013; a decrease in medication administration errors by 73% (P < .01); a decrease in adverse drug events from sedation drugs by 90%; reconciliation of nearly 3,000 patient medication profiles; and a decrease in pharmacy turn-around time of nearly 80%. A coordinated plan and physician support and technology advances were essential for reducing significant harm from medication errors.
Growth of Specialty Pharmacy Services
Specialty pharmacy is another area of opportunity for health-system pharmacy. With the growing concern for costs and utilization of specialty drugs, every pharmacy director should have a strategy to address the impact of specialty pharmacy on their department. Specialty drugs are defined as those drugs used to treat complex chronic and/or life-threatening conditions; they are costly and usually require special storage, handling, and site-of-care administration and significant patient education, monitoring, and management. The growing use of specialty biologic molecules in key therapeutic areas such as oncology, muscular dystrophy, inflammatory conditions (eg, arthritis), infectious disease, and orphan (ie, rare) diseases is becoming a budgetary threat to health plans and employers who provide medical coverage. For example, it is predicted that if all eligible genotype 1 hepatitis C virus patients were treated with the newer NS5A and NS5B polymerase inhibitors (eg, ledipasvir and sofosbuvir), the cost would nearly bankrupt the health care system (Kevin A. Colgan, MA, RPh, Associate Vice President, Specialty Pharmacy for University Health System Consortium, personal communication, December 4, 2014).
OSUWMC has a unique opportunity to develop its own platform to effectively manage the specialty drug area. The department recently opened a specialty pharmacy business with plans to expand that business to hospital-based retail pharmacy operations. OSUWMC has a direct channel to physicians for the safe and effective prescribing of specialty drugs. In addition, the integration of patient prescription data from the insurance company along with access to an integrated electronic medical record provides better oversight and control of specialty drug regimens.
SUGGESTIONS FOR STRATEGIC PLANNING FOR 2015
Effective strategic planning focuses on 3 key elements: analysis, planning groups, and execution. These 3 areas, if given the proper attention, will result in an effective strategic plan that provides short-term and long-term results.
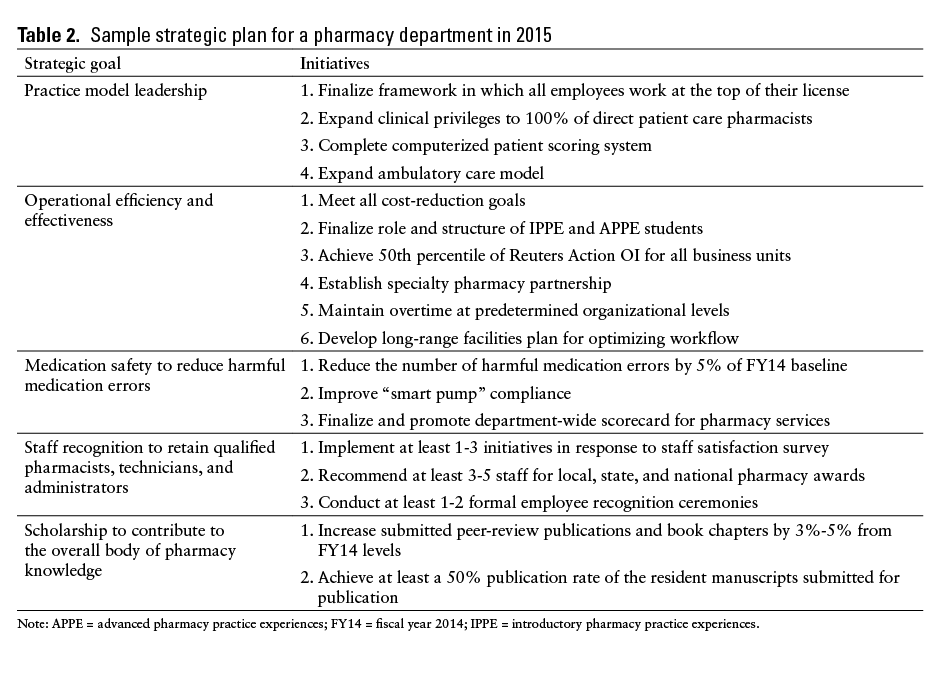
The sample strategic plan template in Table 2 is based on work at OSUWMC as a result of interviews with key stakeholders and an examination of essential department data on cost, quality, and performance. The analysis established the priorities for the pharmacy in 2015. These priorities also match well with the organization’s goals.
Execution of a strategic plan is critical. At OSUWMC, parameters for success include the pharmacy’s role and impact on reducing re-admissions, increasing patient satisfaction, and increasing the safety of the medication use process. Meaningful metrics for the success of a strategic plan include, but are not limited to, patient satisfaction scores, harmful medication errors, order processing times, re-admission rates, staff satisfaction, and financial performance.
A working strategic plan is a fundamental and required tool for departments that want to improve their overall performance. A good plan involves effective analysis, venues for employee input, execution of the plan, and the ability to track progress. Finally, patient-centered services in hospital pharmacy can only be successful through a well-designed and well-executed strategic plan.
CONCLUSION
Pharmacy department leaders must plan for and prioritize the issues facing the profession in the coming year. Several strategies discussed in this article align with the ASHP PPMI and Pharmacy Forecast 2014-2018. Imperatives for strategic plans that address key issues in 2015 include programs to address student roles in practice models and the further definition of the roles of the pharmacist provider status through privileging of staff. Important steps to be taken in 2015 to continue to improve medication safety include leveraging technology and involving staff at the front line with information to reduce harmful medication errors. Pharmacy directors must understand the impact that specialty drugs may have on their drug expenses and the medication needs of patients. Pharmacy directors should develop a strategic plan that considers these issues and their organization’s specific needs to meet the challenges of 2015 and continue to provide patient-centered pharmacy services.
REFERENCES
- Blumenthal D, Collins SR. Health care coverage under the Affordable Care Act – A progress report. N Engl J Med. 2014;371:275-281.
- The Henry J. Kaiser Family Foundation. Health Reform Implementation Timeline. http://kff.org/interactive/implementation-timeline. Accessed December 2, 2014.
- ASHP Foundation. Pharmacy Forecast 2014-2018: Strategic planning advice for pharmacy departments in hospitals and health systems. December 2013. http://www.ashpfoundation.org/PharmacyForecast2014PDF. Accessed December 3, 2014.
- American Society of Health-System Pharmacists. ASHP policies approved by the 2013 ASHP House of Delegates. www.ashp.org/DocLibrary/Policy/HOD/OfficialLang2013Policies.aspx. Accessed December 19, 2014.
- American Society of Health-System Pharmacists. ASHP policy positions, 2009-2012 (with rationales): Education and training. www.ashp.org/DocLibrary/Best Practices/EducationPositions.aspx. Accessed December 19, 2014.
- Buie L. The layered learner practice model and the pharmacy practice model initiative. http://connect.ashp.org/blogsmain/blogviewer/?BlogKey=1ff0fea1-dd0b-46c3-81f6-b5c5ec1e0e95&ssopc=1. Accessed December 19, 2014.
- Delgado O, Kernan WP, Knoer SJ. Advancing the pharmacy practice model in a community teaching hospital by expanding student rotations. Am J Health Syst Pharm. 2014;71:
1871-1876. - http://www.pharmacycredentialing.org/. Accessed December 18, 2014.
- Policies of the University of North Texas Health Science Center. https://app.unthsc.edu/policies/PoliciesPDF/
Physician%20Delegation%20to%20Pharmacists%20under%20a%20Drug%20Therapy%20Management%20Protocol.pdf. Accessed December 17, 2014.
*Administrator, Pharmacy Services, The Ohio State University Wexner Medical Center, The Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, Columbus, Ohio