Original Article
Risk Factors for Recurrent Clostridium difficile Infections and Strategies to Decrease Readmissions in a Community Hospital
Darrin Majors, PharmD, BCPS,* and Patrick Ellis, PharmD*
Original Article
Risk Factors for Recurrent Clostridium difficile Infections and Strategies to Decrease Readmissions in a Community Hospital
Darrin Majors, PharmD, BCPS,* and Patrick Ellis, PharmD*
Original Article
Risk Factors for Recurrent Clostridium difficile Infections and Strategies to Decrease Readmissions in a Community Hospital
Darrin Majors, PharmD, BCPS,* and Patrick Ellis, PharmD*
Abstract
Background: Currently there are no universally accepted approaches for the prevention of recurrent Clostridium difficile infections (CDI) following the initial infection. Several studies have identified common risk factors for the emergence of recurrent CDI. Identifying patients at high risk for recurrent CDI through the assessment of risk factors at initial diagnosis could enable health care providers to optimize available treatment options. A vancomycin hydrochloride–tapered regimen may be an effective treatment option for the prevention of recurrent CDI following the initial infection.
Methods: In this single-center, prospective study, we examined the efficacy of orally administered vancomycin-tapered regimens for the prevention of recurrent CDI in high-risk patients. High-risk patients were identified using patient risk factors found in a retrospective chart review. The primary objective was to decrease hospital readmissions for recurrent CDI. The secondary objective was to improve the discharge coordination-of-care process by providing a pharmacy benefits evaluation, which ensured vancomycin affordability and assistance in prescription attainment, and discharge counseling.
Results: Of the 83 patients enrolled in the study, 5 experienced recurrent CDI (6%). Memorial Health Care System’s (Chattanooga, Tennessee) historical recurrent CDI rate was 8.2%. Thirty-one of the 83 patients received a vancomycin-tapered regimen following their initial infection (37%). A pharmacy benefits evaluation was performed on 35 of the 57 patients who were discharged home on vancomycin (61%).
Conclusions: Vancomycin-tapered regimens may provide a cost-effective method for the prevention of recurrent CDI following an initial infection in patients at high risk for recurrence.
Key Words—hospital readmissions, recurrent Clostridium difficile, risk factors, vancomycin taper
Hosp Pharm 2015;50:1003–1010
Abstract
Background: Currently there are no universally accepted approaches for the prevention of recurrent Clostridium difficile infections (CDI) following the initial infection. Several studies have identified common risk factors for the emergence of recurrent CDI. Identifying patients at high risk for recurrent CDI through the assessment of risk factors at initial diagnosis could enable health care providers to optimize available treatment options. A vancomycin hydrochloride–tapered regimen may be an effective treatment option for the prevention of recurrent CDI following the initial infection.
Methods: In this single-center, prospective study, we examined the efficacy of orally administered vancomycin-tapered regimens for the prevention of recurrent CDI in high-risk patients. High-risk patients were identified using patient risk factors found in a retrospective chart review. The primary objective was to decrease hospital readmissions for recurrent CDI. The secondary objective was to improve the discharge coordination-of-care process by providing a pharmacy benefits evaluation, which ensured vancomycin affordability and assistance in prescription attainment, and discharge counseling.
Results: Of the 83 patients enrolled in the study, 5 experienced recurrent CDI (6%). Memorial Health Care System’s (Chattanooga, Tennessee) historical recurrent CDI rate was 8.2%. Thirty-one of the 83 patients received a vancomycin-tapered regimen following their initial infection (37%). A pharmacy benefits evaluation was performed on 35 of the 57 patients who were discharged home on vancomycin (61%).
Conclusions: Vancomycin-tapered regimens may provide a cost-effective method for the prevention of recurrent CDI following an initial infection in patients at high risk for recurrence.
Key Words—hospital readmissions, recurrent Clostridium difficile, risk factors, vancomycin taper
Hosp Pharm 2015;50:1003–1010
Abstract
Background: Currently there are no universally accepted approaches for the prevention of recurrent Clostridium difficile infections (CDI) following the initial infection. Several studies have identified common risk factors for the emergence of recurrent CDI. Identifying patients at high risk for recurrent CDI through the assessment of risk factors at initial diagnosis could enable health care providers to optimize available treatment options. A vancomycin hydrochloride–tapered regimen may be an effective treatment option for the prevention of recurrent CDI following the initial infection.
Methods: In this single-center, prospective study, we examined the efficacy of orally administered vancomycin-tapered regimens for the prevention of recurrent CDI in high-risk patients. High-risk patients were identified using patient risk factors found in a retrospective chart review. The primary objective was to decrease hospital readmissions for recurrent CDI. The secondary objective was to improve the discharge coordination-of-care process by providing a pharmacy benefits evaluation, which ensured vancomycin affordability and assistance in prescription attainment, and discharge counseling.
Results: Of the 83 patients enrolled in the study, 5 experienced recurrent CDI (6%). Memorial Health Care System’s (Chattanooga, Tennessee) historical recurrent CDI rate was 8.2%. Thirty-one of the 83 patients received a vancomycin-tapered regimen following their initial infection (37%). A pharmacy benefits evaluation was performed on 35 of the 57 patients who were discharged home on vancomycin (61%).
Conclusions: Vancomycin-tapered regimens may provide a cost-effective method for the prevention of recurrent CDI following an initial infection in patients at high risk for recurrence.
Key Words—hospital readmissions, recurrent Clostridium difficile, risk factors, vancomycin taper
Hosp Pharm 2015;50:1003–1010
Hosp Pharm 2015;50(11):1003–1010
2015 © Thomas Land Publishers, Inc.
doi: 10.1310/hpj5011-1003



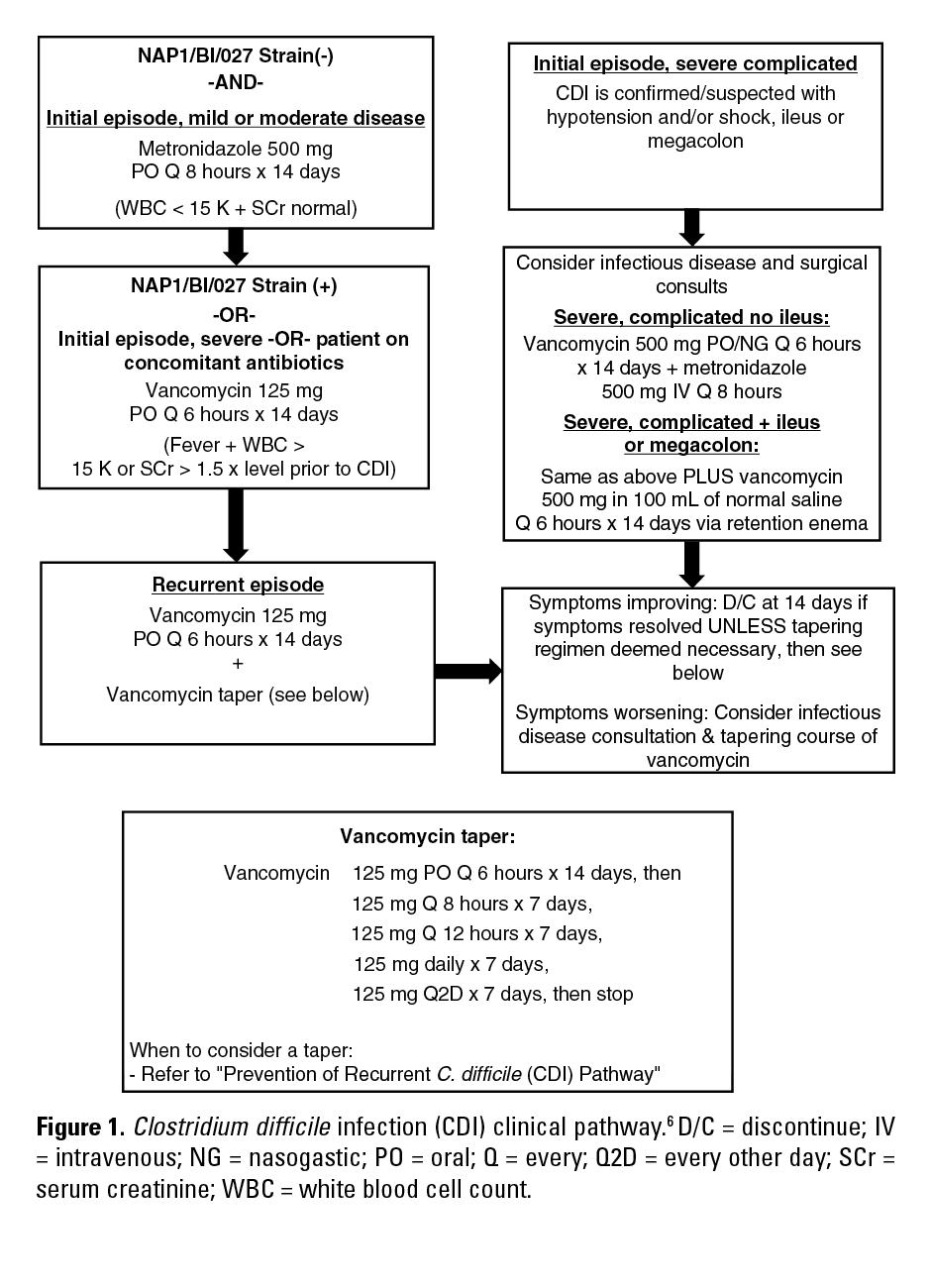
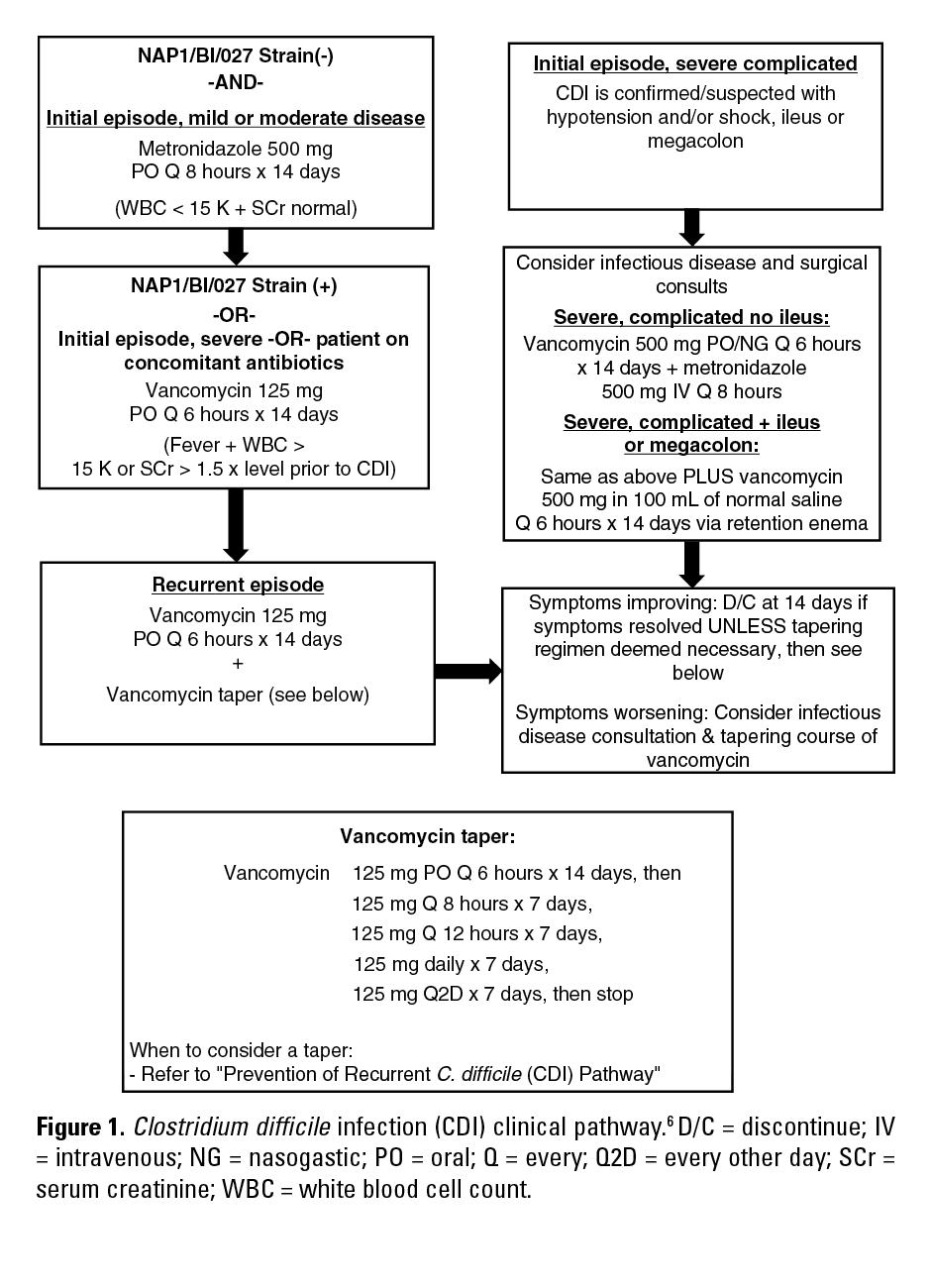




Clostridium difficile is the leading cause of hospital-acquired infectious diarrhea.1 C. difficile is a spore-forming, gram-positive anaerobic bacilli capable of producing toxins, which are the primary virulence factors that cause the clinical manifestations of infection. Toxins bind to receptors in the intestine, which trigger an inflammatory response and diarrhea. The clinical manifestations of infection can range from symptomless colonization to mild, moderate, or severe diarrhea and pseudomembranous colitis.2 The current treatment recommendations issued by the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America (SHEA/IDSA) and the American College of Gastroenterology (ACG) are similar. For a mild or moderate initial episode, the recommended treatment is metronidazole 500 mg by mouth 3 times per day for 10 to 14 days.2,3 For a severe initial episode, the recommended treatment is vancomycin 125 mg by mouth 4 times per day for 10 to 14 days.2,3 For the treatment of a first recurrence, it is recommended to repeat the treatment that was given for the initial episode.2,3 For subsequent recurrent infections, the primary treatment should consist of the use of a vancomycin-tapered and/or pulsed regimen.2,3 Fecal microbiota transfer (FMT) is a novel therapy that may be considered in patients with multiple recurrent infections that have not responded to therapy.3
One of the most troublesome aspects of C. difficile infection (CDI) is the proclivity of recurrence.4 Published literature cite recurrence rates of approximately 20% following the initial diagnosis of CDI and suggest that the recurrence rate is greater than 45% for patients who have had one recurrence.5,6 Recurrent CDI is much more difficult to treat and causes significant morbidity and mortality.5 In addition, recurrent CDI increases the economic burden of health care expenditure. Recurrent CDI most commonly occurs within the first week following cessation of treatment for the original episode but can occur for up to 8 weeks.1,5 Recurrent CDI can be due to either relapse with the original infecting strain or re-infection with a new strain.4 The Centers for Disease Control and Prevention Ad Hoc Clostridium difficile Surveillance Working Group defines recurrent CDI as episodes that occur 2 to 8 weeks after diagnosis of the initial episode and new infections as episodes that occur more than 8 weeks after the onset of a previous episode.7
Preventing and reducing CDI relapse rates is a critical issue in infectious disease. Identifying the most prevalent risk factors for recurrent CDI could enable health care providers to optimize available treatment options and decrease the rate of recurrent CDIs through the implementation of targeted strategies, which would decrease the economic burden of recurrent CDIs.
Currently there are no universally accepted approaches for the prevention of recurrent CDIs following the initial infection. The SHEA/IDSA and ACG guidelines recommend orally administered vancomycin hydrochloride–tapered regimens in patients with multiple recurrent infections.2,3 However, tapered regimens may have larger utility following an initial infection. The evidence of the use of vancomycin-tapered regimens following an initial infection is largely anecdotal, but it may play a larger role in the prevention of recurrent infections. The rationale behind a vancomycin-tapered regimen is the ability to keep C. difficile vegetative forms under control while allowing restoration of the normal flora.2
The aim of this study is to evaluate and identify risk factors for the recurrence of C. difficile infections in patients who are readmitted to the hospital with a diagnosis of C. difficile–associated diarrhea (CDAD) and to implement strategies to decrease the number of recurrent CDIs.
METHODS
Study Design
We conducted a single-center, prospective study to decrease hospital readmissions for recurrent CDI in a community hospital. The protocol was approved by the institutional review board at Memorial Health Care System, Chattanooga, Tennessee.
Study Population
A retrospective chart review was completed for all patients admitted to Memorial Health Care System for recurrent CDI from June 2011 to June 2013 to establish baseline data and identify the most prevalent risk factors for recurrent CDI. In this chart review, an analysis was performed of prespecified patient characteristics that have been identified in clinical trials as risk factors for recurrent CDI (Table 1).1,2,4,5,8,9 In addition, an analysis of physician prescribing practices on appropriate antibiotic selection and duration was performed based on current treatment guidelines published by the SHEA/IDSA and ACG.
The results of the retrospective analysis were then used to identify high-risk patients for recurrent CDI for inclusion in the prospective aspect of the study. Patients were included if they were older than 18 years of age and had a polymerase chain reaction (PCR)–confirmed C. difficile stool sample with acute symptoms at our institution. Exclusion criteria included age younger than 18 years, initial CDI diagnosed prior to admission, non-admitted patients with an emergency department C. difficile–positive stool culture, and death while admitted to the hospital.
Study Procedures
Clinical surveillance, with utilization of MedMined services, was used to identify patients admitted to Memorial Health Care System with a PCR confirmed and symptomatic CDI. Upon patient identification, an antibiotic stewardship pharmacist adhered to 2 algorithms. The first was to ensure appropriate treatment was given according to disease severity as recommended in the SHEA/IDSA treatment guidelines (Figure 1). A second algorithm was used to determine whether the patient was a candidate for a specified 6-week vancomycin-tapered regimen based on the risk factors identified in the retrospective data analysis as well as an additional risk factor that our infectious diseases physician leadership thought was important to include secondary to observed high-risk frequencies (Figure 2).2,6,8 The risk factors for recurrent CDI were used to identify patients at high risk for recurrence. It was the responsibility of the antibiotic stewardship pharmacist to utilize clinical judgment to determine the appropriateness of a vancomycin-tapered regimen. Recommendations for changes in treatment, if any, were then related to the primary physician.
In addition to assessing patient risk for recurrence, the antibiotic stewardship pharmacist performed a pharmacy benefits evaluation on patients discharged home on vancomycin to ensure affordability and attainability of medications, regardless of the regimen or formulation (10-14 days vs tapered). Prior to discharge, an antibiotic stewardship pharmacist provided vancomycin counseling, which included medication adherence, risk of recurrence, out-of-pocket costs, and prescription attainment.
Surveillance and Follow-Up
Patients were monitored by clinical surveillance with the use of MedMined services for re-admittance to Memorial Health Care System for recurrent CDI for a period of 8 weeks following the initial PCR-confirmed stool sample.
Outcome Measures
The primary objective was to decrease hospital readmissions for recurrent CDI. Recurrent CDI was defined as any episode that occurred 2 to 8 weeks after the initial positive stool sample.7 Episodes that occurred more than 8 weeks after the initial positive stool sample were defined as a new infection.7
The secondary objective was to improve the discharge coordination of care process by ensuring vancomycin affordability and providing patient assistance in prescription attainment.
Statistical Analysis
Statistical analysis was not performed.
RESULTS
Retrospective Data Analysis
From June 2011 to June 2013, 474 patients were admitted to Memorial Health Care System with a diagnosis of CDI and 39 were readmitted with recurrent infection (8.2%). The most prevalent risk factors identified in the patients with recurrent infection were age older than 65 years (77%), a primary diagnosis of CDI at admission (64%), immunosuppression (21%), and concomitant non-CDI antibiotic use at diagnosis (15%). Physician prescribing practices, per recommendations published in the SHEA/IDSA and ACG treatment guidelines, were appropriate.
Patients
From January 21 to May 5, 2014, 96 patients were admitted to Memorial Health Care System with a diagnosis of CDI. Thirteen patients were excluded from the study; 9 due to incomplete documentation, 2 due to an initial CDI diagnosed prior to admission, and 2 due to death. Of the remaining 83 patients, a total of 12 patients were treated with 10 or more days of metronidazole, 30 were treated with 10 or more days of vancomycin, 3 were treated with 10 or more days of metronidazole plus vancomycin, and 38 were treated with a vancomycin-tapered regimen (Figure 3).
Efficacy
Of the 83 patients enrolled in the study, 5 patients were readmitted to Memorial Health Care System with a diagnosis of recurrent CDI (6%) in the time frame of February 4, 2014 to July 31, 2014. Two of the 5 patients were treated with a standard vancomycin regimen for 14 days and 3 were treated with a vancomycin-tapered regimen. Of the 5 patients who experienced recurrence, 4 received a pharmacy benefits evaluation. The 1 patient who did not receive a pharmacy benefits evaluation was discharged on a vancomycin-tapered regimen.
A total of 31 patients were treated with a vancomycin-tapered regimen following the diagnosis of their initial infection. Of these, 3 patients were readmitted for recurrent CDI (9.4%).
Other Outcomes
Per SHEA/IDSA guideline recommendations, 79 of the 83 patients (95%) enrolled in the study received appropriate treatment given their disease severity.
Of the 57 patients who were discharged home on oral vancomycin, pharmacists performed a pharmacy benefits evaluation on 35 (61%) prior to discharge.
DISCUSSION
In the retrospective chart review, it was noted that the most common risk factors in the patient population were age older than 65 years, a primary diagnosis of CDI at admission, immunosuppression, and concomitant non-CDI antibiotic use at diagnosis. Chronic hemodialysis was included as an additional risk factor as our infectious diseases physician leadership thought it was an important risk factor to include secondary to observed high-risk frequencies. Patients who present to the hospital with a primary diagnosis of CDI are more likely to have a more severe case. The rationale is that the symptoms were severe enough to bring the patient to the hospital. It should be noted that all patients have different propensities to go to the hospital. A primary diagnosis at admission should prompt a thorough history and subsequent work-up on the severity of the patient’s infection. C. difficile produces toxins that bind to receptors in the intestine, which trigger an inflammatory response and diarrhea. Immunosuppressed patients have a diminished number of antibodies with the ability to bind toxins and thus are more susceptible to a more severe infection. In addition, these patients are more likely to experience treatment failure. Patients who are older than 65 years of age are more likely to have a diminished immune system and multiple co-morbidities, which make them more likely to receive antibiotics.
This study showed that an institution may decrease the rate of recurrent CDI by using risk factors to identify patients at high risk for recurrent CDI to guide treatment decisions. Prior to this study, Memorial Health Care System’s CDI recurrence rate was 8.2%. After study implementation, the recurrent CDI rate decreased to 6%.
The efficacy of the vancomycin taper can be demonstrated in the overall decrease in the rate of recurrent CDI. In the retrospective analysis, which was used to identify the historical recurrent CDI rate, 6% of the patients received a vancomycin taper following their initial infection. In the prospective analysis, approximately 37% of the patients were treated with a vancomycin taper following their initial infection. The taper recommended by our antibiotic stewardship pharmacist was adapted from a regimen used by an in-house infectious diseases physician. This regimen was chosen secondary to anecdotal success and to provide consistency. Tapered regimens initiated independent of pharmacy recommendations varied according to the regimen preferred by the prescribing physician.
In this study, it was the responsibility of the antibiotic stewardship pharmacist to utilize the risk factors identified in the retrospective analysis in conjunction with clinical judgment to determine the appropriateness of a vancomycin-tapered regimen. It should be noted that the inclusion of a single risk factor did not automatically establish a patient as a potential candidate for a taper.
Although this study was not designed to assess medication compliance, we were able to improve the discharge coordination of care process by ensuring outpatient vancomycin affordability and providing patient assistance in prescription attainment. Previously, these processes were not being performed at Memorial Health Care System. Although medication adherence was not assessed in this study, we believe that these processes increased patient medication compliance, which in turn may have assisted with decreasing hospital readmissions due to recurrent CDI.
When prescribing a medication that is taken 4 times a day that gradually tapers over multiple weeks, it is imperative to provide patient education and assistance to ensure compliance. Costs and compliance are limiting factors of vancomycin-tapered regimens, but this obstacle can be overcome with similar methods to those described in the current study.
Fidaxomicin, a macrolide antibiotic approved for the treatment of CDI, has been shown to decrease the rate of recurrence when compared to a standard 10-day course of vancomycin.10,11 Fidaxomicin demonstrated a decreased rate of recurrent infection at 25 days, but the decreased rate was not seen in patients infected with the more virulent BI/NAP1/027 strain, which has shown to be a predictor of more severe disease, treatment failure, and recurrent disease.6,10,12 In clinical studies, the rates of clinical cure with fidaxomicin were nearly identical to that of vancomycin. The benefit of fidaxomicin versus vancomycin for the treatment of an initial infection is largely predicated on the patient’s risk for recurrent infection and the strain of infection. The high cost of fidaxomicin may limit its role in treatment to patients with exceptional insurance or those capable of handling its financial burden. Vancomycin-tapered regimens may provide a cost-effective method for preventing recurrent CDIs. Additional studies comparing fidaxomicin and vancomycin-tapered regimens could provide a clearer insight on the most efficient means for preventing recurrent CDIs.
Memorial Health Care System’s historical BI/NAP1/027 strain prevalence is approximately 11%. The observed BI/NAP1/027 rate in the prospective analysis was 10.8%. In the retrospective analysis, the BI/NAP1/027 strain was observed in 5 of 32 patients who were readmitted with recurrent CDI (15.6%). In the prospective analysis, the BI/NAP1/027 strain was observed in 3 of the 5 patients who experienced recurrent CDI (60%). Of the 3 patients infected with the BI/NAP1/027 strain and who experienced recurrence, 2 were treated with a vancomycin-tapered regimen following their initial diagnosis.
At Memorial Health Care System, the lab performs 1-step PCR only on loose stool samples following a prescriber’s order. Stool samples are analyzed with PCR technology by utilizing the GeneXpert by Cepheid, which provides C. difficile toxin results in approximately 30 minutes with 93.5% sensitivity and 94% specificity.
The current study has limitations. The study was underpowered to detect a significant difference between treatments. At Memorial Health Care System, a group of clinical pharmacists serve on an antibiotic stewardship team and alternate throughout the week. For a large portion of the study, the antibiotic stewardship pharmacist was responsible for performing each patient’s chart review; therefore the quality of protocol adherence could be variable. In addition, Memorial Health Care System is located in close proximity to 2 different hospitals that provide care to patients in this region. There is a possibility of losing patients to follow-up at neighboring hospitals. Because we only evaluated recurrent CDI that required hospitalization, patients may have sought treatment in the outpatient setting under their primary care physician. However, patients lost to follow-up must be considered in both the retrospective and prospective analysis.
Vancomycin-tapered regimens are commonly used for the treatment of recurrent CDIs that are unresponsive to standard treatment options. Their use for the prevention of recurrent CDI following an initial infection is a novel approach, which may provide utility in controlling medical costs associated with recurrent CDI. FMT is a last-line approach for the treatment of multiple recurrent CDIs, with cited cure rates of up to 90%.13 Although highly effective, successful FMT possesses many difficult challenges, which may make practitioners hesitant to pursue this treatment option. FMT challenges include obtaining a suitable donor, lab screening, cost, and multiple logistical obstacles.13 More effective therapeutic strategies for primary CDIs are needed to help alleviate the need for more invasive strategies such as FMT for patients with recurrent disease. Treatment strategies capable of preventing this stage of infection provide a valuable resource to practitioners.
Currently, there is a lack of literature defining a standard vancomycin-tapered regimen and its efficacy in the prevention of recurrent CDIs. The use of vancomycin-tapered regimens for the prevention of recurrent CDI is largely centered on anecdotal evidence by individual practitioners. Similarly, many of the regimens that are used were developed from practitioner experience and lack clinical evidence of their efficacy. Future studies with the use of vancomycin-tapered regimens for the prevention of recurrent CDI in patients at high risk will be necessary to further validate its role in this setting and to define a standard tapered regimen. The efficacy of a vancomycin-tapered regimen could be more accurately described if this study were to be duplicated in the outpatient setting. This would allow the opportunity to analyze the overall recurrence rate.
ACKNOWLEDGMENTS
Neither author has any financial or personal relationships with commercial entities or their competitors to disclose.
REFERENCES
- Hu, M, Katchar, K, Kyne, L, et al. Prospective derivation and validation of a clinical prediction rule for recurrent Clostridium difficile infection. Gastroenterology. 2009;136:1206-1214.
- Cohen, SH, Gerding, DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults: 2010 Update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31(5):431-455.
- Surawicz, CM, Brandt, LJ, Binion, DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478-498.
- Marsh, J, Arora, R, Schlackman, J, et al. Recurrent Clostridium difficile disease: Association of relapse with BI/NAP1/027. J Clin Microbiol. 2012;50(12):4078-4082.
- Eyre W, Walker SA, Wyllie D, et al. Predictors of first recurrence of Clostridium difficile infection: Implications for initial management. Clin Infect Dis. 2012;55(S2):S77-87.
- Johnson S. Recurrent Clostridium difficile infection: Causality and therapeutic approaches. Int J Antimicrob Agents. 2009;33(suppl 1):S33-36.
- The Centers for Disease Control and Prevention and National Healthcare Safety Network. Multidrug-resistant organism and Clostridium difficile infection (MDRO/CDI) module. http://www.cdc.gov/nhsn/PDFs/pscManual/12pscMDRO_CDADcurrent.pdf. April 2015. Accessed October 7, 2015. July 2013 CDC/NHSN Protocol Clarifications.
- Drekonja DM, Amundson WH, DeCarolis DD, et al. Antimicrobial use and risk for recurrent Clostridium difficile infection. Am J Med. 2011;124:1081.e1-1081.e7.
- Garey KW, Sethi S, Yadav Y, et al. Meta-analysis to assess risk factors for recurrent Clostridium difficile infection. J Hosp Infect. 2008;70:298-304.
- Louie, TJ, Miller, MA, Mullane, KM, et al. Fidaxomicin versus vancomycin for Clostridium difficile infections. N Engl J Med. 2004;364:422-431.
- Cornely, OA, Crook, DW, Esposito, R, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: A double-blind, non-inferiority, randomised trial. Lancet Infect Dis. 2012;12:281-289.
- See, I, Mu, Y, Cohen, J, et al. NAP1 strain type predicts outcomes from Clostridium difficile infection. Clin Infect Dis. 2014;58(10):1394-1400.Youngster I, Sauk J, Pindar C, et al. Fecal microbiota transplant for relapsing Clostridium difficile infection using a frozen inoculum from unrelated donors: A randomized, open-label, controlled pilot study. Clin Infect Dis. 2014;58(11):1515-1522.

*Pharmacy Department, Memorial Health Care System, Chattanooga, Tennessee. Corresponding author: Darrin Majors, PharmD, BCPS, 2525 deSales Avenue, Chattanooga, TN 37404; phone: 423-495-8380; fax: 423-495-6703; e-mail: darrin_majors@memorial.org