Falls in the Elderly Secondary to Urinary Symptoms
Yousef Soliman, MD,1 Richard Meyer, MD,2 Neil Baum, MD3
1Cairo, Egypt; 2Department of Orthopedics, Touro Infirmary, New Orleans, LA; 3Department of Urology, Tulane Medical School, New Orleans, LA
Falls and fractures have a significant impact on our patients, their families, and caregivers, and cost the health care system billions of dollars. Each year, millions of adults aged 65 and older fall. Falls can cause moderate to severe injuries, such as hip fractures and head traumas, and can increase the risk of early death. Fortunately, falls are a public health problem that is largely preventable. Because many patients with falls and subsequent fractures have urologic conditions, urologists are positioned to help with the prevention of these significant and costly injuries. This article discusses the epidemiology of falls and fractures, and the urologic comorbidities that increase their risk.
[Rev Urol. 2016;18(1):28-32 doi: 10.3909/riu0686]
© 2016 MedReviews®, LLC
Falls in the Elderly Secondary to Urinary Symptoms
Yousef Soliman, MD,1 Richard Meyer, MD,2 Neil Baum, MD3
1Cairo, Egypt; 2Department of Orthopedics, Touro Infirmary, New Orleans, LA; 3Department of Urology, Tulane Medical School, New Orleans, LA
Falls and fractures have a significant impact on our patients, their families, and caregivers, and cost the health care system billions of dollars. Each year, millions of adults aged 65 and older fall. Falls can cause moderate to severe injuries, such as hip fractures and head traumas, and can increase the risk of early death. Fortunately, falls are a public health problem that is largely preventable. Because many patients with falls and subsequent fractures have urologic conditions, urologists are positioned to help with the prevention of these significant and costly injuries. This article discusses the epidemiology of falls and fractures, and the urologic comorbidities that increase their risk.
[Rev Urol. 2016;18(1):28-32 doi: 10.3909/riu0686]
© 2016 MedReviews®, LLC
Falls in the Elderly Secondary to Urinary Symptoms
Yousef Soliman, MD,1 Richard Meyer, MD,2 Neil Baum, MD3
1Cairo, Egypt; 2Department of Orthopedics, Touro Infirmary, New Orleans, LA; 3Department of Urology, Tulane Medical School, New Orleans, LA
Falls and fractures have a significant impact on our patients, their families, and caregivers, and cost the health care system billions of dollars. Each year, millions of adults aged 65 and older fall. Falls can cause moderate to severe injuries, such as hip fractures and head traumas, and can increase the risk of early death. Fortunately, falls are a public health problem that is largely preventable. Because many patients with falls and subsequent fractures have urologic conditions, urologists are positioned to help with the prevention of these significant and costly injuries. This article discusses the epidemiology of falls and fractures, and the urologic comorbidities that increase their risk.
[Rev Urol. 2016;18(1):28-32 doi: 10.3909/riu0686]
© 2016 MedReviews®, LLC
Key words
Falls • Fractures • Nocturia • Overactive bladder • Urinary tract infections • Prevention
Key words
Falls • Fractures • Nocturia • Overactive bladder • Urinary tract infections • Prevention
In older patients, a fall may be a nonspecific presenting sign of many acute illnesses, including pneumonia, urinary tract infection, or myocardial infarction.
Medications that cause orthostatic hypotension can result in falls.
… these symptoms may force abrupt, unexpected alterations of daily physical routines and compel affected individuals to engage in potentially risky behaviors, such as arising several times a night to urinate.
If a patient has decreased bone mineral density, which is determined by bone densitometry scanning, it is prudent to be certain that the patient is taking supplemental calcium and vitamin D and to refer the patient to a physical therapist for instructions on weight-bearing exercises.
Main Points
• Among older adults, falls are the leading cause of both fatal and nonfatal injuries. They are the leading cause of injury-related visits to emergency departments in the United States, as well as the primary etiology of accidental deaths in people over age 65.
• Many falls are linked to a person’s physical condition or a medical problem, such as arthritis, benign prostatic hyperplasia (BPH), or overactive bladder (OAB). Other causes include certain medications and lower urinary tract symptoms. Both BPH and OAB are associated with nocturia, which is often the prevailing factor leading to nighttime falls and fractures.
• Published reports have suggested that urgency, frequency, nocturia, and urinary incontinence are associated with an increased likelihood of falls in older adults. The inference is that these symptoms may force unexpected alterations of daily physical routines and compel affected individuals to engage in potentially risky behaviors, such as arising several times a night to urinate. Thus, urinary symptoms may be a potential target for preventive interventions to reduce fall risk in community-dwelling men and women.
• The most effective prevention of falls involves a multidisciplinary, holistic, and patient-specific approach. Proactive prevention of falls could include increasing exercise and physical activity, improving management of any medical conditions, reviewing medication, and changing adverse environmental factors.
Main Points
• Among older adults, falls are the leading cause of both fatal and nonfatal injuries. They are the leading cause of injury-related visits to emergency departments in the United States, as well as the primary etiology of accidental deaths in people over age 65.
• Many falls are linked to a person’s physical condition or a medical problem, such as arthritis, benign prostatic hyperplasia (BPH), or overactive bladder (OAB). Other causes include certain medications and lower urinary tract symptoms. Both BPH and OAB are associated with nocturia, which is often the prevailing factor leading to nighttime falls and fractures.
• Published reports have suggested that urgency, frequency, nocturia, and urinary incontinence are associated with an increased likelihood of falls in older adults. The inference is that these symptoms may force unexpected alterations of daily physical routines and compel affected individuals to engage in potentially risky behaviors, such as arising several times a night to urinate. Thus, urinary symptoms may be a potential target for preventive interventions to reduce fall risk in community-dwelling men and women.
• The most effective prevention of falls involves a multidisciplinary, holistic, and patient-specific approach. Proactive prevention of falls could include increasing exercise and physical activity, improving management of any medical conditions, reviewing medication, and changing adverse environmental factors.
One-third of adults over age 65 fall each year. Unfortunately, fewer than half of these people discuss falling with their health care providers.1 Among older adults, falls are the leading cause of both fatal and nonfatal injuries. In 2013, 2.5 million nonfatal falls among older adults were treated in emergency departments and more than 734,000 of these patients required hospitalization.2 In 2012, the direct medical costs of falls in the United States were $30 billion when adjusted for inflation.3
Falls are the leading cause of injury-related visits to emergency departments in the United States, as well as the primary etiology of accidental deaths in people over age 65.4,5 The mortality rate for falls increases dramatically with age in both sexes and in all racial and ethnic groups, with falls accounting for 70% of accidental deaths in people aged 75 years and older.4,5 Falls can be indicators of declining health and deteriorating motor function, and they are associated with significant morbidity. More than 90% of hip fractures occur as a result of falls, with most of these fractures occurring in people over age 70 years.4,5 One-third of community-dwelling elderly persons, and 60% of nursing home residents, fall each year.5 From 1992 through 1995, 147 million injury-related visits were made to emergency departments in the United States.6 Falls were the leading cause of external injury, accounting for 24% of these visits.6 Emergency department visits related to falls are most common in children under age 5 years and in adults over age 65 years. Compared with children, elderly persons who fall are 10 times more likely to be hospitalized and 8 times more likely to die as the result of a fall.7
Trauma is the fifth leading cause of death in persons older than age 65 years,4,5 and falls are responsible for 70% of accidental deaths in persons age 75 years and older.4,5 The elderly, who represent 12% of the population, account for 75% of deaths from falls.4,5 Annually, 1800 falls directly result in death.8 Approximately 9500 deaths in older Americans are associated with falls each year.9
Benign Prostatic Hyperplasia and Overactive Bladder
Falls do not occur de novo and people do not fall just because they age. Often, more than one underlying comorbid condition or risk factor is involved in a fall. As the number of risk factors rises, so does the possibility of falling. Many falls are linked to a person’s physical condition or a medical problem, such as arthritis, benign prostatic hyperplasia (BPH), or overactive bladder (OAB). Other causes include safety hazards in the person’s home or community environment; examples include a slick floor or a poorly lit stairway, loose rugs, lack of stair railings, lack of grab bars in the bathroom, and clutter on the floor.
In older patients, a fall may be a nonspecific presenting sign of many acute illnesses, including pneumonia, urinary tract infection, or myocardial infarction. It may also be the sign of acute exacerbation of a chronic disease.10
Medication
There are multiple medications that can contribute to falls. The leading medication culprits are psychotropic (especially benzodiazepines, antidepressants, and antipsychotics), blood pressure-lowering drugs, and anticonvulsants.11 Sedative medication, including hypnotics, may impair coordination and cause falls.12 There is a particular risk of falls in agitated patients with cognitive impairment. Medications that cause orthostatic hypotension can result in falls. Examples of medications causing orthostatic hypotension include the following13:
- Diuretics (can cause dehydration and may cause urgency and falls)
- Vasodilators (including calcium channel blockers and nitrates)
- Angiotensin-converting enzyme inhibitors
- α-blockers
- Phenothiazines
- Tricyclic antidepressants
- Levodopa
- Bromocriptine
- β-blockers
- Insulin
Major injuries, including head trauma, soft tissue injuries, fractures, and dislocations, occur in 5% to 15% of falls.14 Fractures account for 75% of serious injuries, with hip fractures occurring in 1% to 2% of falls.14
In 1996, more than 250,000 older Americans suffered fractured hips, at a cost in excess of $10 billion. More than 90% of hip fractures are associated with falls, and most of these fractures occur in persons over age 70 years.11 Hip fracture is the leading fall-related injury that results in hospitalization, which is often prolonged and costly.15
Lower Urinary Tract Symptoms
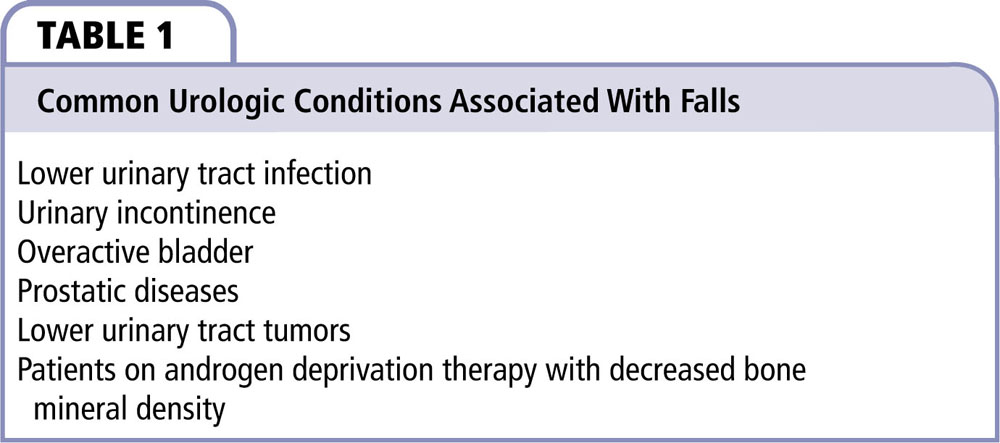
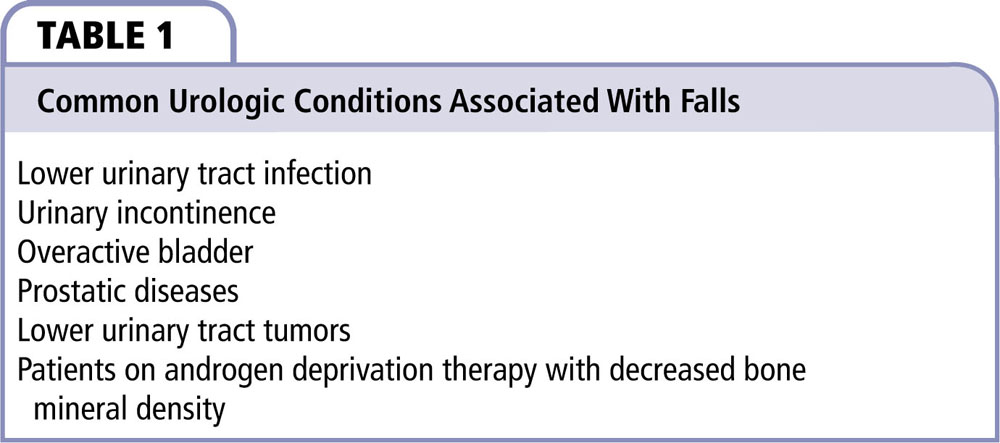
Lower urinary tract symptoms (LUTS) represent a cluster of highly prevalent chronic urinary disorders that occur among 15% to 60% of men over age 40.16,17 The prevalence increases sharply with age.17-19 The most common etiologies for chronic LUTS are BPH and OAB, conditions that collectively affect tens of millions of older men and women.16,20 BPH affects 70% of men aged 75 or older; 42% describe symptoms consistent with OAB.20 Both BPH and OAB are associated with nocturia, which is often the prevailing factor leading to nighttime falls and fractures. The most common etiologies of falls are listed in Table 1.16-20
Nearly one in four community-dwelling men over age 65 have one or more falls each year.21,22 A substantial proportion of these individuals will have serious injury, pain, depression, and other comorbidities. Multifaceted interventions directed toward known risk factors are an effective means of preventing falls in men and women living in the community.23
LUTS are a potential risk factor for falls in community-dwelling men. Published reports have suggested that urgency, frequency, nocturia, and urinary incontinence are associated with an increased likelihood of falls in older adults.24,25 The mechanistic inference is that these symptoms may force abrupt, unexpected alterations of daily physical routines and compel affected individuals to engage in potentially risky behaviors, such as arising several times a night to urinate. Thus, if this association is confirmed, urinary symptoms may be a potential target for preventive interventions to reduce fall risk in community-dwelling men and women.
In one US study of 6049 community-based women, one or more episodes per week of urgency incontinence were independently associated with fall risk.26 Similar findings from Finland were reported for 1016 older home-dwelling adults with both urinary urgency and urinary incontinence.27 In a prospective study of 405 Taiwanese community senior citizens, urinary frequency or incontinence was reported more frequently among fallers than nonfallers, and were among six factors that predicted the risk of falls.28 In addition to urgency and urgency incontinence, stress urinary incontinence and daytime or nocturnal urinary frequency have also been associated with increased risk of falls.29,30 Data from a longitudinal health-screening program of 1508 ambulatory older men and women revealed that nocturia episodes at least twice nightly significantly increased risk of falls, and that risk increased dramatically in those reporting more than three episodes.31
Prevention
Many clinical commissioning groups now have multidisciplinary fall teams that can assess and treat those at risk, but we believe that members of the primary care team should also contribute to the fall prevention strategy. Patient care providers and local communities can also play a role in prevention of falls.32 One study found that encouraging patients to manage their own exercise-based fall prevention program improves compliance, and that physiotherapists should become part of the fall prevention program.33
The most effective prevention of falls involves a multidisciplinary, holistic, and patient-specific approach. Measures should take into account the person’s medical conditions, social circumstances, and psychologic factors. Moreover, proactive prevention of falls could include increasing exercise and physical activity, improving management of any medical conditions, reviewing medication, and changing adverse environmental factors.
Examples of prevention include the following:
- Adapting the home: stairs, bathrooms, and kitchens can present hazards for older people; even if changes don’t need to be made immediately, perform an annual safety review in order to make necessary updates as individual needs change.
- Exercising and training: falls are serious in older people—they often result in fractures that can lead to disability, further health problems, or even death; safety precautions are important, but so are exercises that can improve balance and strength.
An effective screening tool for urologists who care for patients at risk for falls consists of five items: (1) assessing previous falls, (2) agitation, (3) visual impairment, (4) toileting frequency, and (5) transfer/mobility problems, using the Barthel Index Scoring System. Each item is scored with 1 point for a “yes” or 0 points for a “no” response to questions related to the above five items; loadings are not used, giving each risk equal value. A score of ≥ 2 is used to determine a high risk of falling.34
Communication With Colleagues to Prevent Falls and Fractures
Patients who are at risk for falls and fractures with urologic conditions, such as BPH, incontinence, and OAB, will need more attention and support than can be accomplished by a urologist alone. Other colleagues include the primary care physician, the orthopedist, the physical therapist, and the patient’s pharmacist.
When urologists have provided care for a patient who is at risk of falls and fractures, it is helpful to inform the primary care physician of concerns and alert him or her in the referral letter that this risk has been identified.
If a patient has decreased bone mineral density, which is determined by bone densitometry scanning, it is prudent to be certain that the patient is taking supplemental calcium and vitamin D and to refer the patient to a physical therapist for instructions on weight-bearing exercises.
Finally, if there is a question of decrease in the patient’s vision, the urologist should suggest that the patient have his or her eyes checked by an eye doctor at least annually and update his or her eyeglass prescription to maximize vision. Patients should consider getting a pair of glasses with single vision distance lenses for some activities, such as walking outside.
Conclusions
Falls and fractures are, for the most part, preventable. Physicians need to be aware of the morbidity and mortality associated with falls and fractures. Many patients who experience falls and subsequent fractures have associated urologic comorbidities. Urologists need to help patients who are at risk for falls and fractures by making every effort to bring these risk factors to the attention of patients and care givers, and find ways to help prevent falls and fractures. ![]()
References
- Stevens JA, Ballesteros MF, Mack KA, et al. Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med. 2012;43:59-62.
- Home and recreational safety. Important facts about falls. Centers for Disease Control and Prevention website. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed January 12, 2016.
- Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290-295.
- Weigelt JA. Trauma. In: Advanced Trauma Life Support for Doctors. 6th ed. Chicago, IL: American College of Surgeons;1997:26.
- Greenhouse AH. Falls among the elderly. In: Albert ML, Knoefel JE, eds. Clinical Neurology of Aging. 2nd ed. New York, NY: Oxford University Press; 1994:611-626.
- Burt CW, Fingerhut LA. Injury visits to hospital emergency departments: United States, 1992–95. Vital Health Stat 13. 1998:1-76.
- Runge JW. The cost of injury. Emerg Med Clin North Am. 1993;11:241-253.
- Dial LK. Falls. In: Sadovsky R, ed. Conditions of Aging. Baltimore, MD: Williams & Wilkins; 1999:119-126.
- Capezuti E. Falls. In: Forciea MA, Lavizzo-Mourey RJ, Schwab EP, eds. Geriatric Secrets. Philadelphia, PA: Hanley and Belfus; 1996:110-115.
- Rabin DW. Falls and gait disorders. In: Abrams WB, Beers MH, Berkow R, eds. The Merck Manual of Geriatrics. 2nd ed. Rahway, NJ: Merck Sharp & Dohme Research Laboratories; 1995:65-78.
- Hartikainen S, Lönnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62:1172-1181.
- Mets MA, Volkerts ER, Olivier B, Verster JC. Effect of hypnotic drugs on body balance and standing steadiness. Sleep Med Rev. 2010;14:259-267.
- Berlie HD, Garwood CL. Diabetes medications related to an increased risk of falls and fall-related morbidity in the elderly. Ann Pharmacother. 2010;44:712-717.
- King MB, Tinetti ME. A multifactorial approach to reducing injurious falls. Clin Geriatr Med. 1996;12:745-759.
- Mahoney JE. Immobility and falls. Clin Geriatr Med. 1998;14:699-726.
- Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256-1261.
- Trueman P, Hood SC, Nayak US, Mrazek MF. Prevalence of lower urinary tract symptoms and self-reported diagnosed ‘benign prostatic hyperplasia’, and their effect on quality of life in a community-based survey of men in the UK. BJU Int. 1999;83:410-415.
- Boyle P, Robertson C, Mazzetta C, et al; UrEpik Study Group. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int. 2003;92:409-414.
- Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637-649.
- Milsom I, Abrams P, Cardozo L, et al. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87:760-766.
- O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342-354.
- Blake AJ, Morgan K, Bendall MJ, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17:365-372.
- Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279-1284.
- Tromp AM, Pluijm SM, Smit JH, et al. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol. 2001;54:837-844.
- de Rekeneire N, Visser M, Peila R, et al. Is a fall just a fall: correlates of falling in healthy older persons. The Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:841-846.
- Brown JS, Vittinghoff E, Wyman JF, et al. Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48:721-725.
- Luukinen H, Koski K, Kivela SL, Laippala P. Social status, life changes, housing conditions, health, functional abilities and life-style as risk factors for recurrent falls among the home-dwelling elderly. Public Health. 1996;110:115-118.
- Huang HC. A checklist for assessing the risk of falls among the elderly. J Nurs Res. 2004;12:131-142.
- Foley AL, Loharuka S, Barrett JA, et al. Association between the geriatric giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age Ageing. 2012;41:35-40.
- Vaughan CP, Brown CJ, Goode PS, et al. The association of nocturia with incident falls in an elderly community-dwelling cohort. Int J Clin Pract. 2010;64:577-583.
- Stewart RB, Moore MT, May FE, et al. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992;40:1217-1220.
- Roe B, Howell F, Riniotis K, et al. Older people and falls: health status, quality of life, lifestyle, care networks. J Clin Nurs. 2009;18:2261-2272.
- Robinson L, Newton JL, Jones D, et al. Self-management and adherence with exercise-based falls prevention programmes: a qualitative study to explore the views and experiences of older people and physiotherapists. Disabil Rehabil. 2014;36:379-386.
- Preventing falls and harm from falls in older people. Best Practice Guidelines for Australian Hospitals and Residential Aged Care Facilities. Australian Commission on Safety and Quality in Healthcare website. http://www.safetyandquality.gov.au/wp-content/uploads/2012/01/Guidelines-RACF.pdf. Accessed January 12, 2016.