A Decade of Progress in Regional ST-Segment Elevation Myocardial Infarction Systems of Care: A Tale of Two Cities
David C. Lange, MD,1 Ivan C. Rokos, MD,2 David C. Larson, MD,3 Scott W. Sharkey, MD,3 William J. French, MD,4 William J. Koenig, MD,5 Timothy D. Henry, MD1
1Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles, CA; 2Department of Emergency Medicine, The David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Division of Cardiology, Minneapolis Heart Institute, Minneapolis, MN; 4Division of Cardiology, Harbor UCLA Medical Center, Los Angeles, CA; 5Department of Emergency Medicine, Long Beach Memorial Medical Center, Long Beach, CA
Over the past 20 years, care for patients with ST-elevation myocardial infarction (STEMI) has rapidly evolved, not just in terms of how patients are treated, but where patients are treated. The advent of regional STEMI systems of care has decreased the number of “eligible but untreated” patients while improving access to primary percutaneous coronary intervention for patients. These regional STEMI systems of care have consistently demonstrated that rapid transport of STEMI patients is safe and effective, and have shown marked improvements in a variety of clinical outcomes. However, no two STEMI systems are alike, and each must be tailored to the unique geographic, political, and socioeconomic challenges of the region. This article takes an in-depth look at two of the earliest STEMI systems within the United States: the Minneapolis Heart Institute and the Los Angeles County STEMI receiving network.
[Rev Cardiovasc Med. 2016;17(1/2):1-6 doi: 10.3909/ricm0808]
© 2016 MedReviews®, LLC
A Decade of Progress in Regional ST-Segment Elevation Myocardial Infarction Systems of Care: A Tale of Two Cities
David C. Lange, MD,1 Ivan C. Rokos, MD,2 David C. Larson, MD,3 Scott W. Sharkey, MD,3 William J. French, MD,4 William J. Koenig, MD,5 Timothy D. Henry, MD1
1Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles, CA; 2Department of Emergency Medicine, The David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Division of Cardiology, Minneapolis Heart Institute, Minneapolis, MN; 4Division of Cardiology, Harbor UCLA Medical Center, Los Angeles, CA; 5Department of Emergency Medicine, Long Beach Memorial Medical Center, Long Beach, CA
Over the past 20 years, care for patients with ST-elevation myocardial infarction (STEMI) has rapidly evolved, not just in terms of how patients are treated, but where patients are treated. The advent of regional STEMI systems of care has decreased the number of “eligible but untreated” patients while improving access to primary percutaneous coronary intervention for patients. These regional STEMI systems of care have consistently demonstrated that rapid transport of STEMI patients is safe and effective, and have shown marked improvements in a variety of clinical outcomes. However, no two STEMI systems are alike, and each must be tailored to the unique geographic, political, and socioeconomic challenges of the region. This article takes an in-depth look at two of the earliest STEMI systems within the United States: the Minneapolis Heart Institute and the Los Angeles County STEMI receiving network.
[Rev Cardiovasc Med. 2016;17(1/2):1-6 doi: 10.3909/ricm0808]
© 2016 MedReviews®, LLC
A Decade of Progress in Regional ST-Segment Elevation Myocardial Infarction Systems of Care: A Tale of Two Cities
David C. Lange, MD,1 Ivan C. Rokos, MD,2 David C. Larson, MD,3 Scott W. Sharkey, MD,3 William J. French, MD,4 William J. Koenig, MD,5 Timothy D. Henry, MD1
1Division of Cardiology, Cedars-Sinai Heart Institute, Los Angeles, CA; 2Department of Emergency Medicine, The David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Division of Cardiology, Minneapolis Heart Institute, Minneapolis, MN; 4Division of Cardiology, Harbor UCLA Medical Center, Los Angeles, CA; 5Department of Emergency Medicine, Long Beach Memorial Medical Center, Long Beach, CA
Over the past 20 years, care for patients with ST-elevation myocardial infarction (STEMI) has rapidly evolved, not just in terms of how patients are treated, but where patients are treated. The advent of regional STEMI systems of care has decreased the number of “eligible but untreated” patients while improving access to primary percutaneous coronary intervention for patients. These regional STEMI systems of care have consistently demonstrated that rapid transport of STEMI patients is safe and effective, and have shown marked improvements in a variety of clinical outcomes. However, no two STEMI systems are alike, and each must be tailored to the unique geographic, political, and socioeconomic challenges of the region. This article takes an in-depth look at two of the earliest STEMI systems within the United States: the Minneapolis Heart Institute and the Los Angeles County STEMI receiving network.
[Rev Cardiovasc Med. 2016;17(1/2):1-6 doi: 10.3909/ricm0808]
© 2016 MedReviews®, LLC
KEY WORDS
STEMI • Systems of care • Health services research
KEY WORDS
STEMI • Systems of care • Health services research
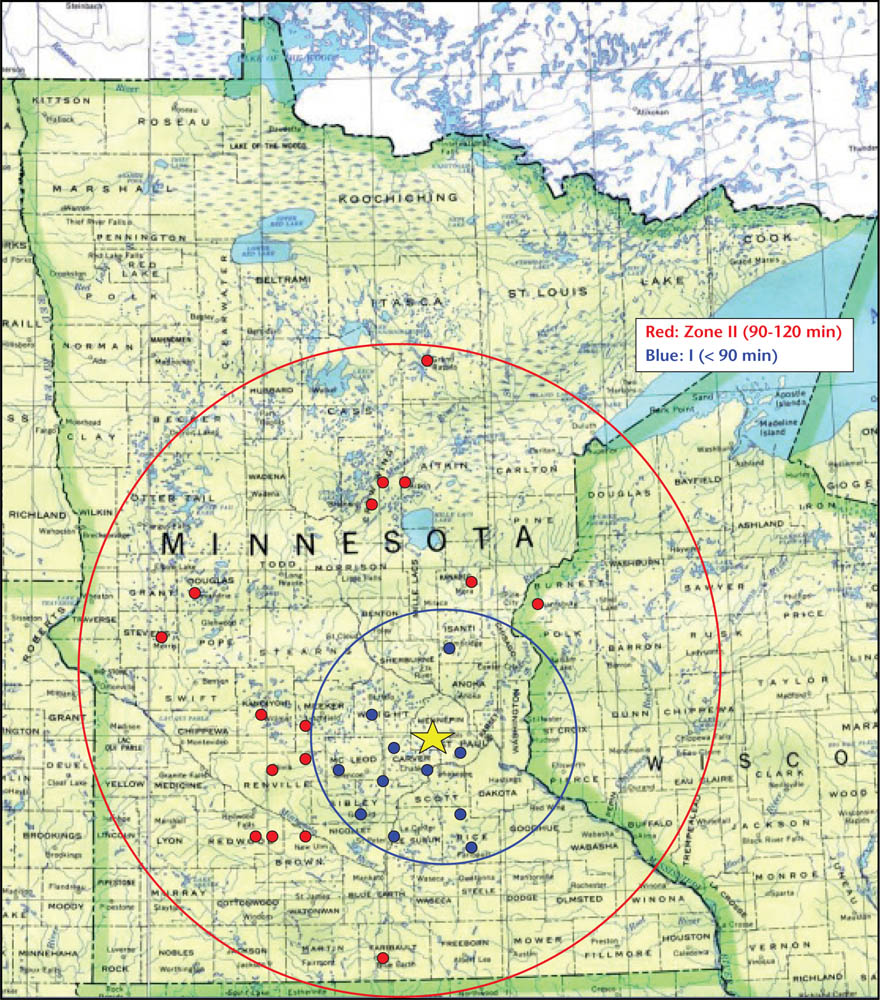
Figure 1. Minneapolis Heart Institute ST-segment elevation myocardial infarction receiving system of care.
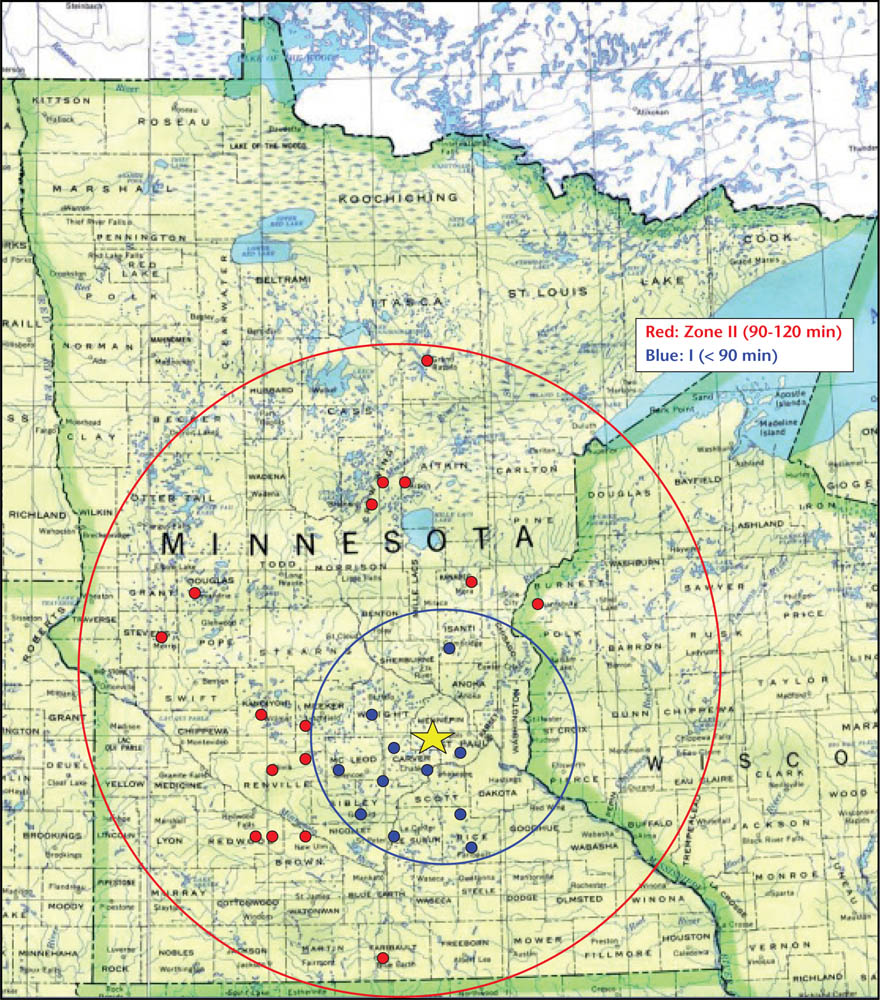
Figure 1. Minneapolis Heart Institute ST-segment elevation myocardial infarction receiving system of care.
We demonstrated safe and effective rapid transport of STEMI patients and achieved unequivocal improvements in several key outcomes, including death, reinfarction, stroke, and length of hospital stay.
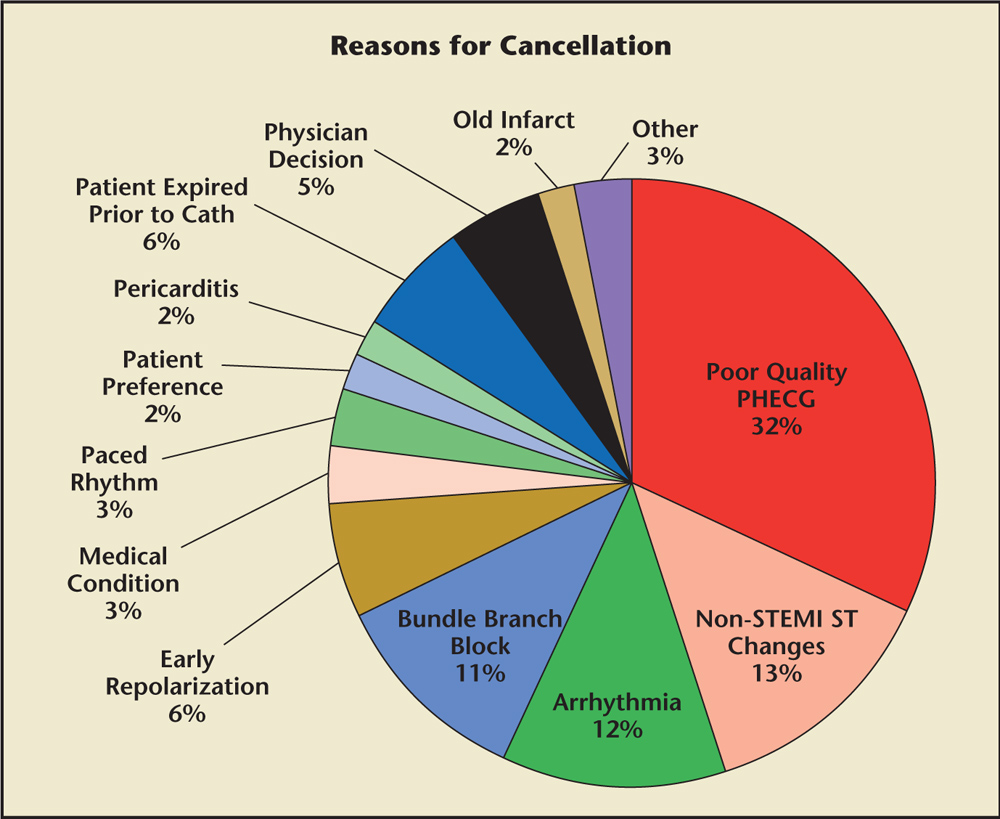
Figure 2. ST-segment elevation myocardial infarction (STEMI) cardiac catheterization laboratory activations that were not taken emergently for cardiac catheterization labeled according to the reasons for cancellation. Cath, catheterization; PHECG, prehospital electrocardiogram.
To effectively triage patients to the appropriate hospital (SRC vs closest available hospital), LA County pioneered the prehospital ECG (PHECG) into the EMS care plan, with the PHECG computer interpretation determining patient triage and destination.
Figure 3. Los Angeles County and Orange County ST-segment elevation myocardial infarction receiving center network. Image courtesy of the Los Angeles County Emergency Medical Services Agency.
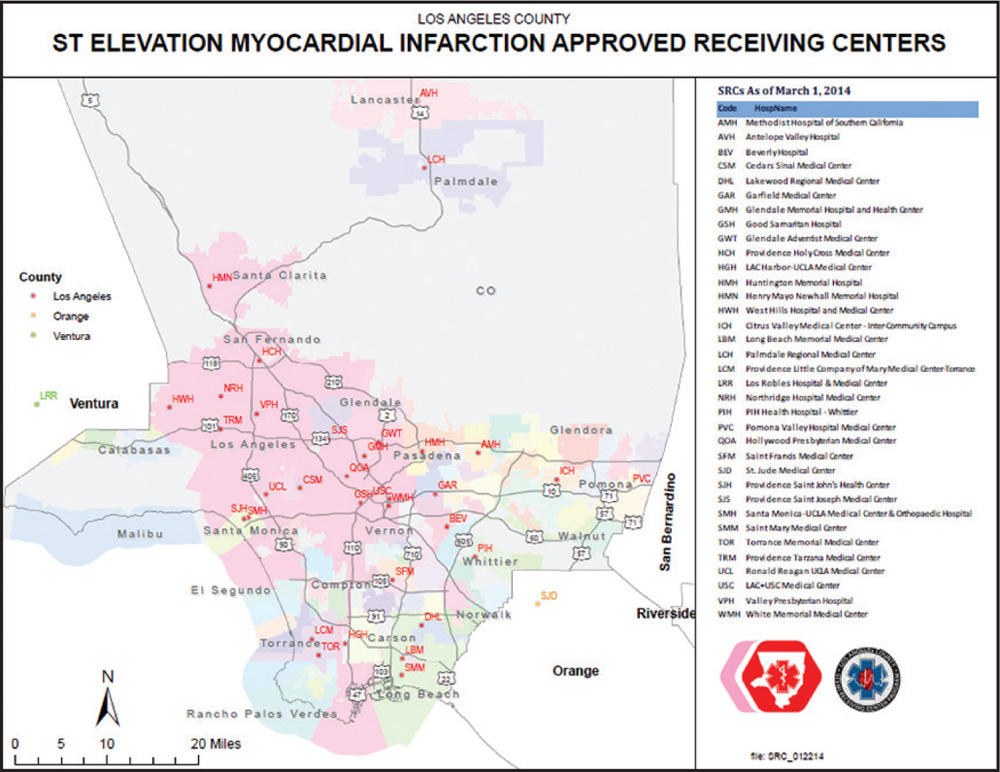
Figure 3. Los Angeles County and Orange County ST-segment elevation myocardial infarction receiving center network. Image courtesy of the Los Angeles County Emergency Medical Services Agency.
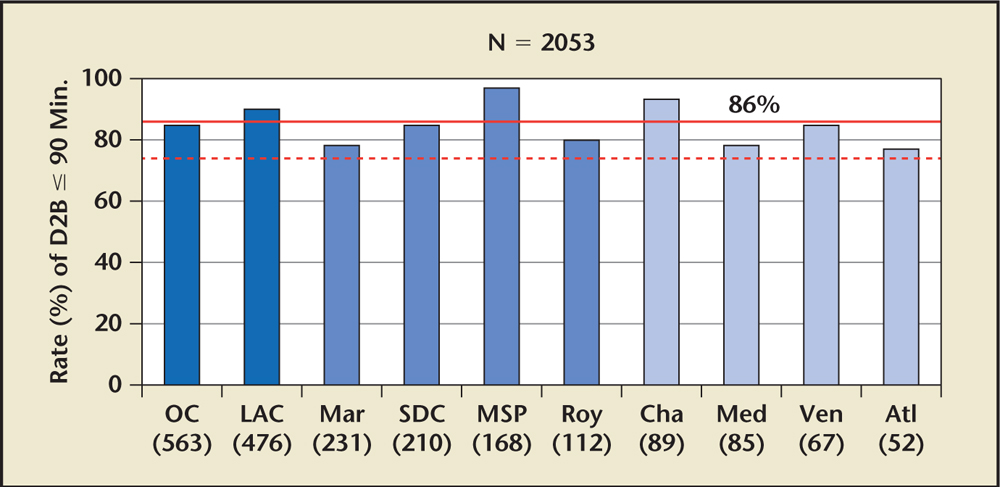
Figure 4. Rate of D2B time ≤ 90 minutes in US ST-segment elevation myocardial infarction receiving networks, 2009. Atl, Atlanta, Georgia; Cha, Charlotte, North Carolina; D2B, door-to-balloon; LAC, Los Angeles County, California; Mar, Marin County, California; Med, Medford, Oregon; MSP, Minneapolis/St. Paul, Minnesota; OC, Orange County, California; Roy, Royal Oak, Michigan; SDC, San Diego County, California; Ven, Ventura County, California. Reprinted with permission from Rokos IC et al.22
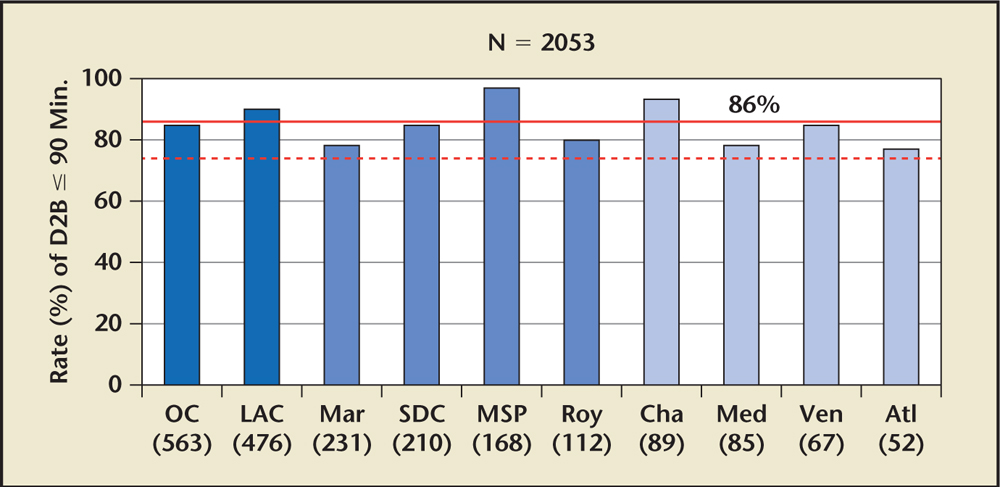
Figure 4. Rate of D2B time ≤ 90 minutes in US ST-segment elevation myocardial infarction receiving networks, 2009. Atl, Atlanta, Georgia; Cha, Charlotte, North Carolina; D2B, door-to-balloon; LAC, Los Angeles County, California; Mar, Marin County, California; Med, Medford, Oregon; MSP, Minneapolis/St. Paul, Minnesota; OC, Orange County, California; Roy, Royal Oak, Michigan; SDC, San Diego County, California; Ven, Ventura County, California. Reprinted with permission from Rokos IC et al.22
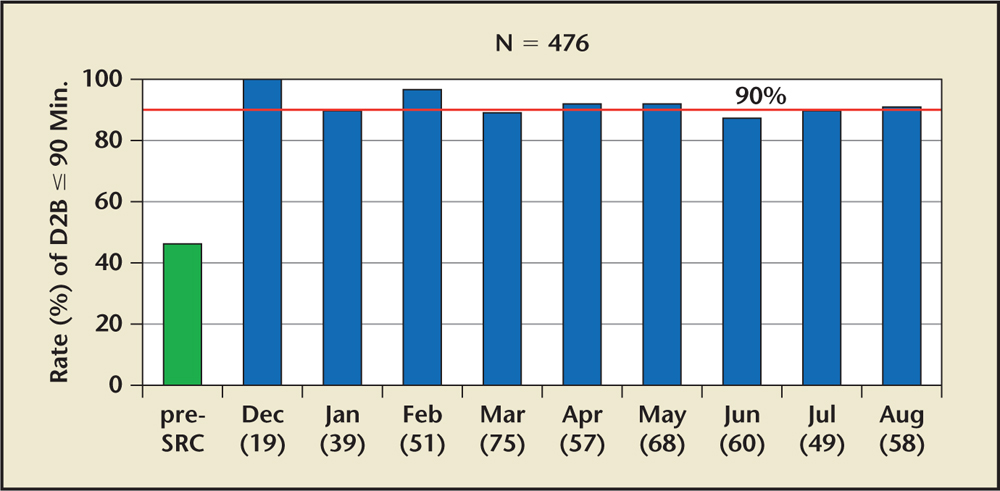
Figure 5. Rate of door-to-balloon (D2B) time ≤ 90 minutes in Los Angeles County ST-segment elevation myocardial infarction (STEMI) receiving network before STEMI Receiving Center (SRC) network implementation (green) and immediately after implementation (blue). Reprinted with permission from Rokos IC et al.22
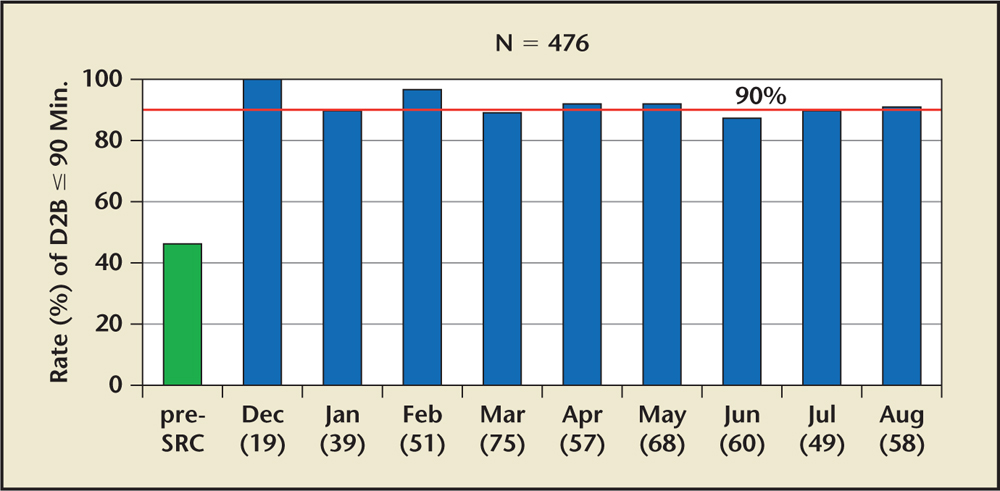
Figure 5. Rate of door-to-balloon (D2B) time ≤ 90 minutes in Los Angeles County ST-segment elevation myocardial infarction (STEMI) receiving network before STEMI Receiving Center (SRC) network implementation (green) and immediately after implementation (blue). Reprinted with permission from Rokos IC et al.22
The fundamental task for successful regional STEMI systems of care is to match the individual STEMI patient with an appropriate hospital or treatment center able to provide the highest and most definitive quality of care (eg, primary PCI).
Main Points
• When performed in a timely manner by experienced operators, primary percutaneous coronary intervention (PCI) is the preferred method of reperfusion for patients presenting with ST-segment elevation myocardial infarction (STEMI).
• The Minneapolis Heart Institute (MHI; Minneapolis, MN) initiated one of the first regional STEMI systems in the United States, and was modeled after successful regional trauma systems and based on preliminary results from a Danish trial, with the premise that prompt diagnosis and a streamlined process with a standardized care protocol was fundamental to the implementation of a successful STEMI system within the United States.
• Shortly after the creation of the MHI STEMI network, Los Angeles (LA) County began formulating its unique network of STEMI receiving centers—hospitals that provide primary PCI around the clock and also accept STEMI patients even when the hospital’s Emergency Department is on diversion because of overcrowding.
• Although the MHI STEMI network was established as a wheel-and-spoke model, with a single central hub, the unique geography, population density, and political climate of LA County demanded a different model, with multiple hubs strategically located throughout LA County. MHI focused initially on an interhospital transfer model, whereas LA County focused on a prehospital triage model.
• Continued advancements in digital technology will allow faster and more reliable prehospital electrocardiogram (PHECG) transmission with immediate front-line physician review, which should significantly reduce inappropriate cardiac catheterization laboratory (CCL) activation while concurrently allowing earlier appropriate CCL activation (and potential Emergency Department bypass) for patients with unequivocal STEMI on PHECG.
Main Points
• When performed in a timely manner by experienced operators, primary percutaneous coronary intervention (PCI) is the preferred method of reperfusion for patients presenting with ST-segment elevation myocardial infarction (STEMI).
• The Minneapolis Heart Institute (MHI; Minneapolis, MN) initiated one of the first regional STEMI systems in the United States, and was modeled after successful regional trauma systems and based on preliminary results from a Danish trial, with the premise that prompt diagnosis and a streamlined process with a standardized care protocol was fundamental to the implementation of a successful STEMI system within the United States.
• Shortly after the creation of the MHI STEMI network, Los Angeles (LA) County began formulating its unique network of STEMI receiving centers—hospitals that provide primary PCI around the clock and also accept STEMI patients even when the hospital’s Emergency Department is on diversion because of overcrowding.
• Although the MHI STEMI network was established as a wheel-and-spoke model, with a single central hub, the unique geography, population density, and political climate of LA County demanded a different model, with multiple hubs strategically located throughout LA County. MHI focused initially on an interhospital transfer model, whereas LA County focused on a prehospital triage model.
• Continued advancements in digital technology will allow faster and more reliable prehospital electrocardiogram (PHECG) transmission with immediate front-line physician review, which should significantly reduce inappropriate cardiac catheterization laboratory (CCL) activation while concurrently allowing earlier appropriate CCL activation (and potential Emergency Department bypass) for patients with unequivocal STEMI on PHECG.
When performed in a timely manner by experienced operators, primary percutaneous coronary intervention (PCI) is the preferred method of reperfusion for patients presenting with ST-segment elevation myocardial infarction (STEMI).1,2 In the early 2000s, multiple European trials demonstrated that transferring STEMI patients to PCI-capable hospitals yielded superior outcomes compared with fibrinolysis at non-PCI capable hospitals.3-5 However, there were doubts as to whether these results could be replicated within the construct of the US healthcare system.6 Although the trial was small and underpowered, the only US STEMI transfer trial (Air Primary Angioplasty in Myocardial Infarction) reported a total median door-to-balloon (D2B) time of 155 minutes with equivocal results when compared with European trials.7
In 2003, the Minneapolis Heart Institute (MHI) at Abbott Northwestern Hospital (Minneapolis, MN) initiated one of the first regional STEMI systems in the United States. The system was modeled after successful regional trauma systems and based on preliminary results from the Danish Trial in Acute Myocardial Infarction-2 (DANAMI-2), with the premise that prompt diagnosis and a streamlined process with a standardized care protocol is fundamental to the implementation of a successful STEMI system within the United States.3,8,9 The MHI system functioned as a “wheel-and-spoke” model, with MHI at the center of the system (Figure 1). Referral hospitals and clinics within a 60-mile radius of MHI were designated as Zone 1, with a standardized protocol that included evidence-based adjunctive medications (aspirin, clopidogrel, weight-based intravenous heparin loading dose, and intravenous β-blockers), together with a prespecified transfer plan for each site. Transfer times within a 60-mile radius were felt to be short enough to allow primary PCI to be performed within 90 minutes of presentation in these patients. The regional STEMI system grew quickly and was expanded to a broader geographic area, Zone 2, which included referral hospitals within a 60- to 210-mile radius using a similar standardized protocol with the addition of onsite half-dose intravenous tenecteplase followed by immediate transfer to MHI for pharmacoinvasive PCI.9,10 Given the longer distances (and thus, longer transfer times), we believed initiating reperfusion at the referral hospital would improve outcomes. Implementation of this complex regional STEMI system of care increased access to primary PCI for patients who would otherwise be ineligible due to geographic constraints or medical comorbidities.10-12 We demonstrated safe and effective rapid transport of STEMI patients and achieved unequivocal improvements in several key outcomes, including death, reinfarction, stroke, and length of hospital stay.9-13 Although these results demonstrate remarkable progress in the care of STEMI patients, significant challenges remain.13-15 In particular, patients transferred from non-PCI centers continue to experience delays, although the frequency, magnitude, and clinical impact depend on a variety of factors. In addition, the issue of false-positive catheterization laboratory activation is a vexing problem in many US regions, though rates of false-positive STEMIs in the MHI system remain low.16-19 In the MHI system, the STEMI team is activated with a single phone call based on the review and interpretation of the initial provider, which includes a variety of professionals (doctors, mid-level providers, and emergency medical services [EMS]) with various areas of expertise (eg, emergency medicine, general internal medicine, family practice). All providers are trained, and prompt and consistent feedback is emphasized. There is no mechanism for transmission or over-reading of the electrocardiogram (ECG), although a provider is able to request cardiology input if needed, which occurs in fewer than 5% of cases. STEMI activations are only cancelled if contraindications to cardiac catheterization become evident after activations (eg, severe hyperkalemia, anemia/bleeding diathesis, goals of care). With in this system, the rates of false-positive activation (as [1] no culprit lesion on cardiac catheterization, and [2] negative cardiac enzymes) is 9.2%.15 Other systems may vary depending on the definition of false-positive, but have reported rates as high as 40% to 60%.16-18 Common reasons for cancellation at Los Angeles (LA) County STEMI receiving center are shown in Figure 2.19
Shortly after the creation of the MHI STEMI network, LA County began formulating its unique network of STEMI receiving centers (SRCs)—hospitals that provide primary PCI around the clock and also accept STEMI patients even when the hospital’s Emergency Department is on diversion because of overcrowding. The creation of the LA County SRC network was precipitated by a convergence of events, including the 2004 American College of Cardiology (ACC)/American Heart Association (AHA) STEMI guidelines, which established the benchmark goal for D2B time of ≤ 90 minutes and the 2006 ACC D2B Alliance.20 With regulatory authority over all 25 EMS providers and 2500 paramedics in the region, the LA County EMS Agency built a consensus among diverse stakeholders and implemented a 2006 policy in which any STEMI patient identified before reaching the hospital was preferentially transported to the nearest designated SRC, even if this required bypassing a closer non-PCI hospital (Figure 3).21 To effectively triage patients to the appropriate hospital (SRC vs closest available hospital), LA County pioneered the integration of the prehospital ECG (PHECG) into the EMS care plan, with the PHECG computer interpretation determining patient triage and destination. This system improved D2B times throughout LA County, and promptly exceeded national standards set forth by the D2B Alliance much sooner than comparable large urban centers. (Figures 4 and 5).22
Although the MHI STEMI network was established as a wheel-and-spoke model,8 with a single central hub (MHI), the unique geography, population density, and political climate of LA County demanded a different model, with multiple hubs strategically located throughout LA County. In essence, MHI focused initially on an interhospital transfer model, whereas LA County focused on a prehospital triage model.20 Ultimately, both locations implemented models to create a comprehensive network across their patient service area. Moreover, both systems layered a system for management of patients with out-of-hospital cardiac arrest in conjunction with their existing STEMI network.
After early success in 2006, LA County faced several serious challenges. Four years elapsed before an interhospital transfer network was successfully established. This process required gradual efforts that encouraged each SRC to partner with surrounding nonaffiliated non-PCI hospitals, as well as solving the issue of slow interhospital transport by private ambulance. Consequently, LA County pioneered the “call 9-1-1” interhospital transfer process in which the local EMS providers were dispatched to the non-PCI hospital Emergency Department to transport a STEMI patient to the nearest SRC.23 A second challenge for LA County has been false-positive or inappropriate cardiac catheterization laboratory (CCL) activations due to errors in interpreting the PHECG. Yet another issue relates to Emergency Department bypass at the SRC for obvious STEMI cases identified by PHECG. Unlike the 24-hour CCL staffing at MHI, most LA County SRCs do not have a CCL team in house after hours (nights, weekends, or holidays); thus, STEMI patients may be delayed in the Emergency Department after hours. Perhaps related to the issue of in-house versus on-call from home STEMI teams, off-hours STEMI activations in the LA County STEMI network had longer D2B times; however, length of stay, vascular complications, and in-hospital mortality did not differ between off-hours and on-hours STEMI activations.24 We hope that continued advancements in digital technology will allow faster and more reliable PHECG transmission with immediate front-line physician review, which should significantly reduce inappropriate CCL activation while concurrently allowing earlier appropriate CCL activation (and potential Emergency Department bypass) for patients with unequivocal STEMI on PHECG.
The successes and challenges encountered by both MHI and LA County systems emphasize that no two STEMI programs are alike. Each US region has unique geographic, political, and socioeconomic challenges, which form complex interactions within the health care system. The fundamental task for successful regional STEMI systems of care is to match the individual STEMI patient with an appropriate hospital or treatment center able to provide the highest and most definitive quality of care (eg, primary PCI). Each system requires construction and refinement tailored to the unique geographic, political, and social needs of regional STEMI systems and, therefore, has led to changes in the ACC/AHA guidelines for STEMI patients. Current guidelines assign a class I, level of evidence B recommendation that “all communities should create and maintain a regional system of STEMI care.”1 The same recommendation level is given to 12-lead ECG performance by EMS personnel.1 Additionally, these systems have provided the impetus for nationwide programs such as the AHA’s Mission: Lifeline.
Although we are proud of the accomplishments contributed by the development and implementation of SRCs in LA County, MHI, and elsewhere, our work is not complete and challenges await resolution. The successful STEMI systems of care model is now being applied to other acute cardiovascular emergencies such as stroke, out-of-hospital cardiac arrest, acute aortic dissection, and massive pulmonary embolism.25 We are confident that the continued efforts of dedicated individuals and communities will further refine, expand, and improve these robust SRC networks. ![]()
The authors report no real or apparent conflicts of interest.
References
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78-e140.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
- Andersen HR, Nielsen TT, Rasmussen K, et al; DANAMI-2 Investigators. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349:733-742.
- Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation. 2003;108:1809-1814.
- De Luca G, Biondi-Zoccai G, Marino P. Transferring patients with ST-segment elevation myocardial infarction for mechanical reperfusion: a meta-regression analysis of randomized trials. Ann Emerg Med. 2008;52:665-676.
- Henry TD, Atkins JM, Cunningham MS, et al. ST-segment elevation myocardial infarction: recommendations on triage of patients to heart attack centers: is it time for a national policy for the treatment of ST-segment elevation myocardial infarction? J Am Coll Cardiol. 2006;47:1339-1345.
- Grines CL, Browne KF, Marco J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993;328:673-679.
- Henry TD, Unger BT, Sharkey SW, et al. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005;150:373-384.
- Henry TD, Sharkey SW, Burke MN, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721-728.
- Larson DM, Duval S, Sharkey SW, et al. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long distance transfers. Eur Heart J. 2012;33:1232-1240.
- Smith LG, Duval S, Tannenbaum MA, et al. Are the results of a regional ST-elevation myocardial infarction system reproducible? Am J Cardiol. 2012;109:1582-1588.
- Newell MC, Henry JT, Henry TD, et al. Impact of age on treatment and outcomes in ST-elevation myocardial infarction. Am Heart J. 2011;161:664-672.
- Miedema MD, Newell MC, Duval S, et al. Causes of delay and associated mortality in patients transferred with ST-elevation myocardial infarction. Circulation. 2011;124:1636-1644.
- Henry TD. From concept to reality: a decade of progress in regional ST-elevation myocardial infarction systems. Circulation. 2012;126:166-168.
- Miedema MD, Newell MC, Henry TD. Delays in the treatment of STEMI: remarkable progress, room for improvement. Interv Cardiol. 2012;4:1-4.
- Larson DM, Menssen KM, Sharkey SW, et al. “False positive” cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA. 2007;298:2754-2760.
- Garvey JL, Monk L, Granger CB, et al. Rates of cardiac catheterization cancellation for ST-segment elevation myocardial infarction after activation by emergency medical services or emergency physicians: results from the North Carolina Catheterization Laboratory Activation Registry. Circulation. 2012;125:308-313.
- Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010;160:995-1003.
- Lange D, Conte S, Pappas-Block E, et al. Cardiac catheterization lab activations for ST-segment elevation myocardial infarction (STEMI) are frequently cancelled at a major Los Angeles County STEMI-receiving center (SRC). Circulation. 2014;130:A12834.
- Rokos IC, Larsen DM, Henry TD, et al. Rationale for establishing a regional ST-elevation myocardial infarction receiving center (SRC) networks. Am Heart J. 2006;152:661-667.
- Map of Los Angeles County STEMI-receiving centers. Los Angeles County Emergency Medical Services Agency. http://ems2.dhs.lacounty.gov/GIS/Maps/Hospital/SRC.pdf. Accessed April 7, 2016..
- Rokos IC, French WJ, Koenig WJ, et al. Integration of pre-hospital electrocardiograms and ST-elevation myocardial infarction receiving (SRC) networks: impact on door-to-balloon times across 10 independent regions. JACC Cardiovasc Interv. 2009;2:339-346.
- Baruch T, Rock A, Koenig WJ, et al. “Call 911” STEMI protocol to reduce delays in transfer of patients from non-primary percutaneous coronary intervention referral centers. Crit Pathw Cardiol. 2010;9:113-115.
- Shavelle DM, Zhang L, Ottochian M, et al. Time of day variation in door-to-balloon times for STEMI patients in Los Angeles County: does time of day make a difference? Acute Card Care. 2013;15:52-57.
- Graham KJ, Strauss CE, Boland LL, et al. Has the time come for a national cardiovascular emergency care system? Circulation. 2012;125:2035-2044.