Vascular Complications of Percutaneous Transradial Cardiac Catheterization
Manish Patwardhan, MD, Sanjay Mehra, MD, Assad Movahed, MD, Ramesh Daggubati, MD
East Carolina Heart Institute, Greenville, NC
The percutaneous transradial approach for coronary angiography and percutaneous coronary intervention is increasing in the United States. Although its vascular safety profile is better than the traditional femoral approach, it is important to learn about potential complications. In this article, we present two cases of vascular complications, namely, pseudoaneurysm and radial artery occlusion, after transradial cardiac catheterization, along with a review of the relevant literature.
[Rev Cardiovasc Med. 2016;17(1/2):76-79 doi: 10.3909/ricm0801]
© 2016 MedReviews®, LLC
Vascular Complications of Percutaneous Transradial Cardiac Catheterization
Manish Patwardhan, MD, Sanjay Mehra, MD, Assad Movahed, MD, Ramesh Daggubati, MD
East Carolina Heart Institute, Greenville, NC
The percutaneous transradial approach for coronary angiography and percutaneous coronary intervention is increasing in the United States. Although its vascular safety profile is better than the traditional femoral approach, it is important to learn about potential complications. In this article, we present two cases of vascular complications, namely, pseudoaneurysm and radial artery occlusion, after transradial cardiac catheterization, along with a review of the relevant literature.
[Rev Cardiovasc Med. 2016;17(1/2):76-79 doi: 10.3909/ricm0801]
© 2016 MedReviews®, LLC
Vascular Complications of Percutaneous Transradial Cardiac Catheterization
Manish Patwardhan, MD, Sanjay Mehra, MD, Assad Movahed, MD, Ramesh Daggubati, MD
East Carolina Heart Institute, Greenville, NC
The percutaneous transradial approach for coronary angiography and percutaneous coronary intervention is increasing in the United States. Although its vascular safety profile is better than the traditional femoral approach, it is important to learn about potential complications. In this article, we present two cases of vascular complications, namely, pseudoaneurysm and radial artery occlusion, after transradial cardiac catheterization, along with a review of the relevant literature.
[Rev Cardiovasc Med. 2016;17(1/2):76-79 doi: 10.3909/ricm0801]
© 2016 MedReviews®, LLC
KEY WORDS
Transradial • Pseudoaneurysm • Artery occlusion • Percutaneous coronary intervention
KEY WORDS
Transradial • Pseudoaneurysm • Artery occlusion • Percutaneous coronary intervention
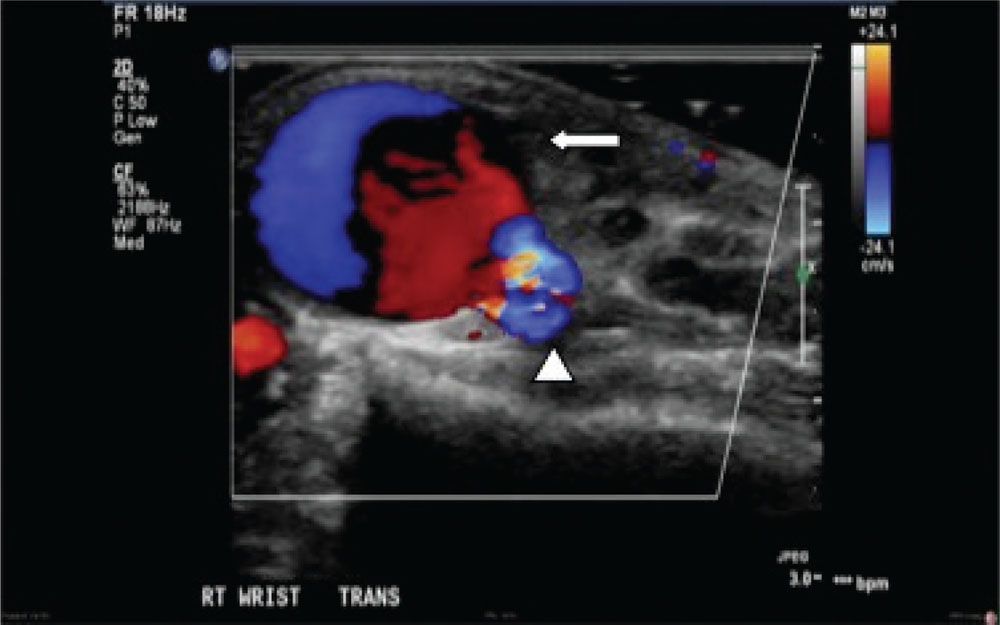
Figure 1. Doppler ultrasound image showing 4.5 3 1.6 3 2.7 cm hypoechoic collection (arrow) superficial to the radial artery (arrowhead).
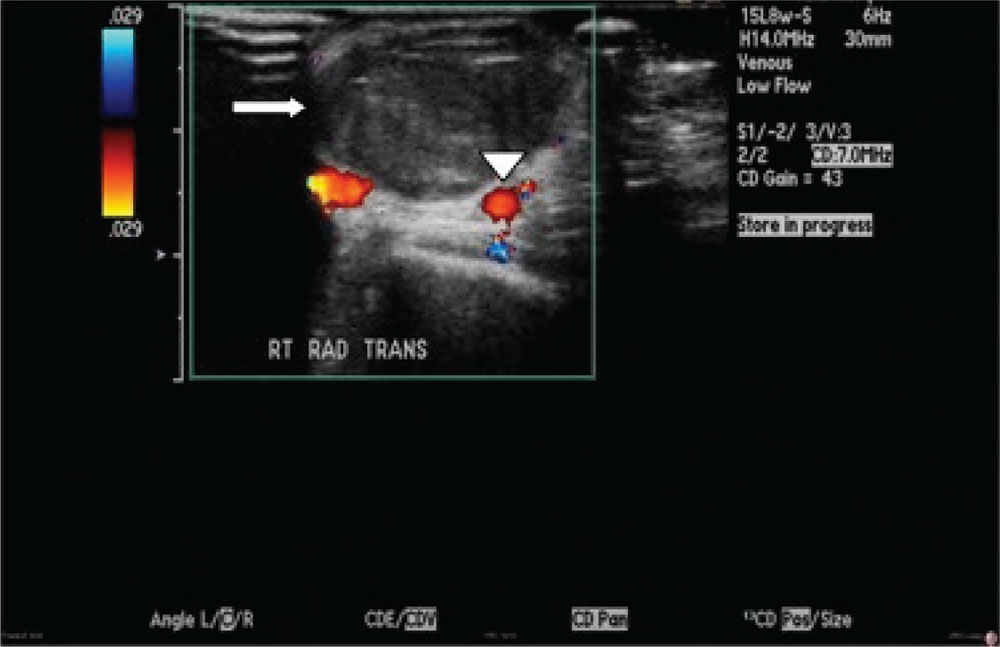
Figure 2. Repeat Doppler ultrasound showing no flow in the hematoma (arrow). The radial artery is seen below (arrowhead).
The so-called steep learning curve associated with TRA has long been considered a hurdle. However, recent evidence suggests the learning curve is less prohibitive than previously perceived…
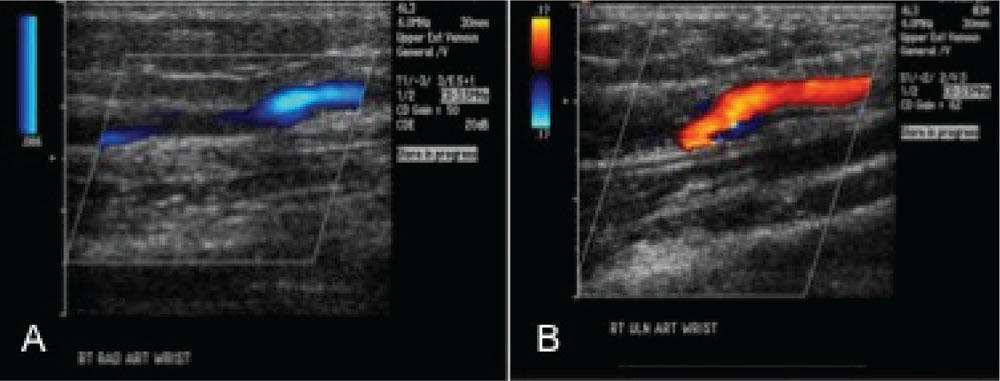
Figure 3. Doppler ultrasound through the right radial artery (A) demonstrates no definite flow from the level of the wrist to the level of the elbow. Right ulnar artery (B) at the level of the wrist is patent.
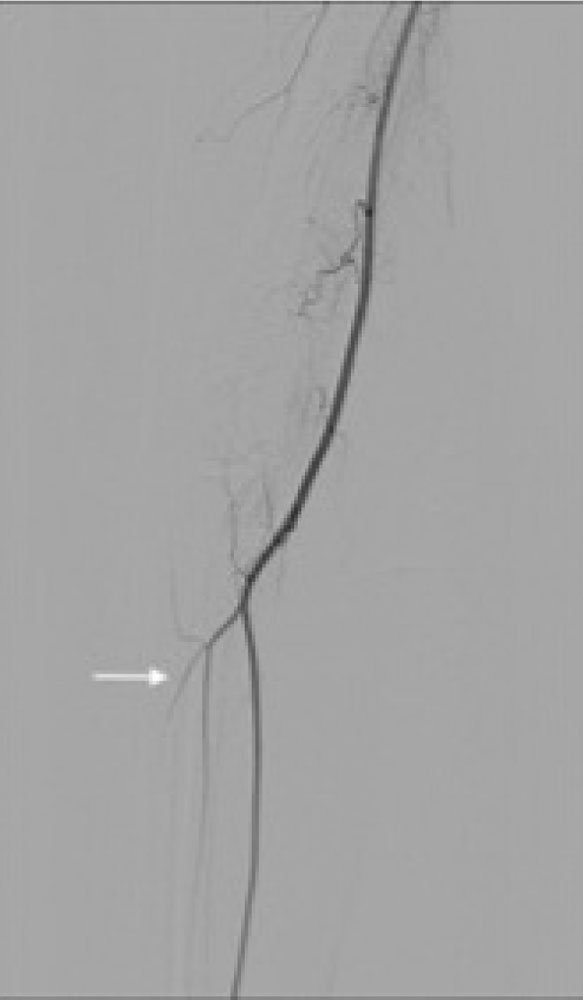
Figure 4. Right radial artery (arrow) occluded at the level of the brachial artery bifurcation just below the antecubital fossa.
Risk factors for PA formation include multiple puncture attempts, aggressive manipulation of the catheters and wires, larger sheath size, inadequate hemostasis, catheter-related infection, and aggressive systemic anticoagulation.
Main Points
• The percutaneous transradial approach is increasingly being used for diagnostic coronary angiography and percutaneous coronary intervention. Proponents of this approach recommend a “radial first” strategy to overcome the learning curve.
• Risk factors for pseudoaneurysm formation include multiple puncture attempts, aggressive manipulation of the catheters and wires, larger sheath size, inadequate hemostasis, catheter-related infection, and aggressive systemic anticoagulation.
• Radial artery occlusion (RAO) is a common complication of transradial catheterization. In contemporary literature, the incidence of RAO is reported to be 5% to 10%. Although a patent arch often ensures that this complication remains benign, catastrophic complications of hand ischemia have been reported.
• Treatment is rarely required for RAO, as it remains clinically asymptomatic in most cases. In acute cases, transient ipsilateral ulnar artery occlusion was reported to recanalize an occluded radial artery.
Main Points
• The percutaneous transradial approach is increasingly being used for diagnostic coronary angiography and percutaneous coronary intervention. Proponents of this approach recommend a “radial first” strategy to overcome the learning curve.
• Risk factors for pseudoaneurysm formation include multiple puncture attempts, aggressive manipulation of the catheters and wires, larger sheath size, inadequate hemostasis, catheter-related infection, and aggressive systemic anticoagulation.
• Radial artery occlusion (RAO) is a common complication of transradial catheterization. In contemporary literature, the incidence of RAO is reported to be 5% to 10%. Although a patent arch often ensures that this complication remains benign, catastrophic complications of hand ischemia have been reported.
• Treatment is rarely required for RAO, as it remains clinically asymptomatic in most cases. In acute cases, transient ipsilateral ulnar artery occlusion was reported to recanalize an occluded radial artery.
The percutaneous transradial approach (TRA) is increasingly being used for diagnostic coronary angiography and percutaneous coronary intervention (PCI). Described first in 1989,1 radial access has gained wider acceptance only in recent years. In the hands of experienced operators, the safety and efficacy of TRA in ST-elevation myocardial infarction is comparable to that of femoral access.2 As radial PCI becomes more prevalent, it is important to learn about potential complications associated with this approach. We present two cases of vascular complications with a review of the management strategies.
Case Report 1
A 66-year-old white woman with hypertension, chronic obstructive pulmonary disease (COPD), and tobacco abuse underwent transradial cardiac catheterization for non–ST-elevation myocardial infarction with routine postprocedural care. One week later, she presented with pounding pain in her right wrist at the site of access and a tingling sensation over the lateral right palm. On examination, she was found to have a pulsatile mass measuring 3 cm in diameter at the radial artery access site extending into the radial border of thenar eminence. Ultrasound and Doppler examination confirmed the presence of a pseudoaneurysm (PA; Figure 1). The patient’s wrist was placed into a carpal tunnel splint for comfort. A vascular surgeon was consulted and conservative management was recommended. On re-evaluation after 5 days, no palpable pulsation could be felt at the site of swelling. Ultrasound showed a hematoma above the pulsating radial artery. Repeat ultrasound examination with Doppler showed no flow into the area of the hematoma (Figure 2).
Case Report 2
A 51-year-old white woman with a history of COPD and anxiety disorder presented to the emergency room with right hand pain. Four days prior, the patient underwent a diagnostic coronary angiogram performed through the right radial artery. On examination, the hand was warm and pink with intact muscle strength, but a radial pulse was absent. An ultrasound examination demonstrated a right radial artery occlusion with absence of any definitive flow through the radial artery from elbow to wrist (Figure 3). Given the absence of neurologic sequelae on examination, and the possibility of spontaneous recanalization, a vascular surgeon recommended a conservative approach with follow-up serial ultrasound examination.
The patient returned a few days later with new paresthesias of her thumb and index finger, and worsening pain over her entire hand. We performed an arteriogram that revealed an occluded right radial artery at the level of the brachial artery bifurcation, just distal to the antecubital fossa (Figure 4). The interosseous artery was patent at the mid right forearm, along with a large patent ulnar artery filling the ulnar arch and digital arteries. The patient was managed conservatively; 6 weeks later, the patient reported resolution of hand pain and paresthesias.
Discussion
Coronary angiography and PCI through TRA were first performed over two decades ago.1,3 In comparison with Europe and Asia, TRA is less commonly used in the United States.4 The so-called steep learning curve associated with TRA has long been considered a hurdle. However, recent evidence suggests the learning curve is less prohibitive than previously perceived5; proponents of this approach recommend a “radial first” strategy to overcome the learning curve.6 In the past decade, the use of TRA for PCI has increased.7 With an improved access site complication profile, decreased cost, and improved patient comfort, TRA is likely to gain more widespread acceptance in the coming years. Therefore, there is a greater need to learn about its possible complications.
Radial Artery PA
PA is described as a tear through all three layers of an arterial wall leading to containment of blood outside the vessel.8 Although an exceedingly rare complication after transradial catheterization (, 0.1%), radial artery PA can have significant sequelae in some patients.9 Risk factors for PA formation include multiple puncture attempts, aggressive manipulation of the catheters and wires, larger sheath size, inadequate hemostasis, catheter-related infection, and aggressive systemic anticoagulation. It usually has an insidious course and can remain unrecognized for several days or weeks after the procedure. Clinical suspicion and early recognition are essential to decrease long-term ischemic or neurologic adverse effects. Diagnosis is confirmed by ultrasound and Doppler examination.
As in our case, PA can sometimes spontaneously resolve itself with absorption of the hematoma; however, on most occasions it warrants an intervention. Management requires discontinuation of the flow communication between the true lumen and pooled blood outside of the lumen. This can be achieved in several different ways. Ultrasound-guided compression is often used to obliterate the neck of the PA using a transducer probe.10 Percutaneous thrombin injection into the sac of the PA under direct sonographic visualization is an option,11 but is deemed less favorable compared with direct surgical repair. A newer approach with a TR Band® (Terumo Interventional Systems, Somerset, NJ) is also reported as a treatment option. The TR Band is positioned over the PA and secured with a hook-and-loop strap. The inflator syringe permits accurate pressure adjustment as air is injected into the side port, which inflates the compression balloon overlying the PA.12
Radial Artery Occlusion
Radial artery occlusion (RAO) is a common complication of transradial catheterization. In contemporary literature, the incidence of RAO is reported to be 5% to 10%.13,14 The radial artery is a convenient access site for catheterization, as the distal upper extremity enjoys a rich collateral flow through the superficial and deep palmar arches. In most cases, RAO remains clinically silent owing to a dual blood supply. Although a patent arch often ensures that this complication remains benign, catastrophic complications of hand ischemia have been reported.15-17 The Allen test, or the more objective Barbeau test, can be used to evaluate this dual blood supply.18 Radial compression using a pneumatic device and achieving patent hemostasis have been shown to decrease the incidence of RAO.19,20 Newer sheath systems are particularly useful in radial arteries that are small; 5F sheaths are now routinely used for most diagnostic and interventional procedures. Sheathless hydrophilic guides may further help in complex PCIs requiring more flexibility with the size of the system.21 Anticoagulation with either heparin or bivalirudin should be used in all PCIs and most diagnostic catheterizations.
Treatment is rarely required for RAO, as it remains clinically asymptomatic in most cases. In acute cases, transient ipsilateral ulnar artery occlusion was reported to recanalize an occluded radial artery.22 Both anterograde and retrograde interventional approaches have been described to recanalize RAOs.23-25 Enoxaparin or fondaparinux was successfully used to treat RAO in a nonrandomized trial by Zankl and colleagues.26
Conclusions
Radial artery PA and RAO are rare but serious complications of TRA. Familiarity with their clinical presentation and management options is critical as we move into an era of increasing use of TRA for diagnostic coronary angiograms and percutaneous interventions. ![]()
References
- Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16:3-7.
- Jolly SS, Yusuf S, Cairns J, et al; RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicenter trial. Lancet. 2011;377:1409-1420.
- Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet Cardiovasc Diagn. 1993;30:173-178.
- Bertrand OF, Rao SV, Pancholy S, et al. Transradial approach for coronary angiography and interventions: results of the first international transradial practice survey. JACC Cardiovasc Interv. 2010;3:1022-1031.
- Rao SV, Cohen MG. Staying ahead of the curve. Cardiovasc Revasc Med. 2014;15:193-194.
- Barbash IM, Minha S, Gallino R, et al. Operator learning curve for transradial percutaneous coronary interventions: implications for the initiation of a transradial access program in contemporary US practice. Cardiovasc Revasc Med. 2014;15:195-199.
- Feldman DN, Swaminathan RV, Kaltenbach LA, et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: an updated report from the national cardiovascular data registry (2007-2012). Circulation. 2013;127:2295-2306.
- Rao SV, Cohen MG. Staying ahead of the curve. Cardiovasc Revasc Med. 2014;15:193-194.
- Kalapatapu VR, Shelton KR, Ali AT, et al. Pseudoaneurysm: a review. Curr Treat Options Cardiovasc Med. 2008;10:173-183.
- Sanmartín M, Cuevas D, Goicolea J, et al. Vascular complications associated with radial artery access for cardiac catheterization [Article in Spanish]. Rev Esp Cardiol. 2004;57:581-584.
- Komorowska-Timek E, Teruya TH, Abou-Zamzam AM Jr, et al. Treatment of radial and ulnar artery pseudoaneurysm using percutaneous thrombin injection. J Hand Surg Am. 2004;29: 936-942.
- Herold J, Brucks S, Boenigk H, et al. Ultrasound guided thrombin injection of pseudo aneurysm of the radial artery after percutaneous coronary intervention. Vasa. 2011;40:78-81.
- Liou M, Tung F, Kanei Y, Kwan T. Treatment of radial artery pseudoaneurysm using a novel compression device. J Invasive Cardiol. 2010;22:293-229.
- Zankl AR, Andrassy M, Volz C, et al. Radial artery thrombosis following transradial coronary angiography: incidence and rationale for treatment of symptomatic patients with low-molecular-weight heparins. Clin Res Cardiol. 2010;99:841-847.
- Sanmartin M, Gomez M, Rumoroso JR, et al. Interruption of blood flow during compression and radial artery occlusion after transradial catheterization. Catheter Cardiovasc Interv. 2007;70:185-189.
- Rhyne D, Mann T. Hand ischemia resulting from a transradial intervention: successful management with radial artery angioplasty. Catheter Cardiovasc Interv. 2010;76:383-386.
- de Bucourt M, Teichgräber U. Digital ischemia and consecutive amputation after emergency transradial cardiac catheter examination. Cardiovasc Intervent Radiol. 2012;35:1242-1244.
- Ruzsa Z, Pintér L, Kolvenbach R. Anterograde recanalisation of the radial artery followed by transradial angioplasty. Cardiovasc Revasc Med. 2010;11:266. e1-266.e4.
- Barbeau GR, Arsenault F, Dugas L, et al. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen‘s test in 1010 patients. Am Heart J. 2004;147:489-493.
- Cubero JM, Lombardo J, Pedrosa C, et al. Radial compression guided by mean artery pressure versus standard compression with a pneumatic device (RACOMAP). Catheter Cardiovasc Interv. 2009;73: 467-472.
- Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion—patent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc Interv. 2008;72:335-340.
- Kotowycz MA, Dzavík V. Radial artery patency after transradial catheterization. Circ Cardiovasc Interv. 2012;5:127-133.
- Bernat I, Bertrand OF, Rokyta R, et al. Efficacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am J Cardiol. 2011;107:1698-1701.
- Babunashvili A, Dundua D. Recanalization and reuse of early occluded radial artery within 6 days after previous transradial diagnostic procedure. Catheter Cardiovasc Interv. 2011;77:530-536.
- Pancholy SB. Transradial access in an occluded radial artery: new technique. J Invasive Cardiol. 2007;19: 541-544.
- Zankl AR, Andrassy M, Volz C, et al. Radial artery thrombosis following transradial coronary angiography: incidence and rationale for treatment of symptomatic patients with low-molecular-weight heparins. Clin Res Cardiol. 2010;99:841-847.