Cardiovascular Effects of Altitude on Performance Athletes
Ankit B. Shah, MD, MPH, Neil Coplan, MD, FACC
Lenox Hill Hospital, New York, NY
Altitude plays an important role in cardiovascular performance and training for athletes. Whether it is mountaineers, skiers, or sea-level athletes trying to gain an edge by training or living at increased altitude, there are many potential benefits and harms of such endeavors. Echocardiographic studies done on athletes at increased altitude have shown evidence for right ventricular dysfunction and pulmonary hypertension, but no change in left ventricular ejection fraction. In addition, 10% of athletes are susceptible to pulmonary hypertension and high-altitude pulmonary edema. Some studies suggest that echocardiography may be able to identify athletes susceptible to high-altitude pulmonary edema prior to competing or training at increased altitudes. Further research is needed on the long-term effects of altitude training, as repeated, transient episodes of pulmonary hypertension and right ventricular dysfunction may have long-term implications. Current literature suggests that performance athletes are not at higher risk for ventricular arrhythmias when training or competing at increased altitudes. For sea-level athletes, the optimal strategy for attaining the benefits while minimizing the harms of altitude training still needs to be clarified, although—for now—the “live high, train low” approach appears to have the most rationale.
[Rev Cardiovasc Med. 2016;17(1/2):49-56 doi: 10.3909/ricm0810]
© 2016 MedReviews®, LLC
Cardiovascular Effects of Altitude on Performance Athletes
Ankit B. Shah, MD, MPH, Neil Coplan, MD, FACC
Lenox Hill Hospital, New York, NY
Altitude plays an important role in cardiovascular performance and training for athletes. Whether it is mountaineers, skiers, or sea-level athletes trying to gain an edge by training or living at increased altitude, there are many potential benefits and harms of such endeavors. Echocardiographic studies done on athletes at increased altitude have shown evidence for right ventricular dysfunction and pulmonary hypertension, but no change in left ventricular ejection fraction. In addition, 10% of athletes are susceptible to pulmonary hypertension and high-altitude pulmonary edema. Some studies suggest that echocardiography may be able to identify athletes susceptible to high-altitude pulmonary edema prior to competing or training at increased altitudes. Further research is needed on the long-term effects of altitude training, as repeated, transient episodes of pulmonary hypertension and right ventricular dysfunction may have long-term implications. Current literature suggests that performance athletes are not at higher risk for ventricular arrhythmias when training or competing at increased altitudes. For sea-level athletes, the optimal strategy for attaining the benefits while minimizing the harms of altitude training still needs to be clarified, although—for now—the “live high, train low” approach appears to have the most rationale.
[Rev Cardiovasc Med. 2016;17(1/2):49-56 doi: 10.3909/ricm0810]
© 2016 MedReviews®, LLC
Cardiovascular Effects of Altitude on Performance Athletes
Ankit B. Shah, MD, MPH, Neil Coplan, MD, FACC
Lenox Hill Hospital, New York, NY
Altitude plays an important role in cardiovascular performance and training for athletes. Whether it is mountaineers, skiers, or sea-level athletes trying to gain an edge by training or living at increased altitude, there are many potential benefits and harms of such endeavors. Echocardiographic studies done on athletes at increased altitude have shown evidence for right ventricular dysfunction and pulmonary hypertension, but no change in left ventricular ejection fraction. In addition, 10% of athletes are susceptible to pulmonary hypertension and high-altitude pulmonary edema. Some studies suggest that echocardiography may be able to identify athletes susceptible to high-altitude pulmonary edema prior to competing or training at increased altitudes. Further research is needed on the long-term effects of altitude training, as repeated, transient episodes of pulmonary hypertension and right ventricular dysfunction may have long-term implications. Current literature suggests that performance athletes are not at higher risk for ventricular arrhythmias when training or competing at increased altitudes. For sea-level athletes, the optimal strategy for attaining the benefits while minimizing the harms of altitude training still needs to be clarified, although—for now—the “live high, train low” approach appears to have the most rationale.
[Rev Cardiovasc Med. 2016;17(1/2):49-56 doi: 10.3909/ricm0810]
© 2016 MedReviews®, LLC
KEY WORDS
Altitude • Athlete • Cardiovascular • Performance
KEY WORDS
Altitude • Athlete • Cardiovascular • Performance
Hyperventilation is the first physiologic change noted during hypoxic exposure at increased altitude.
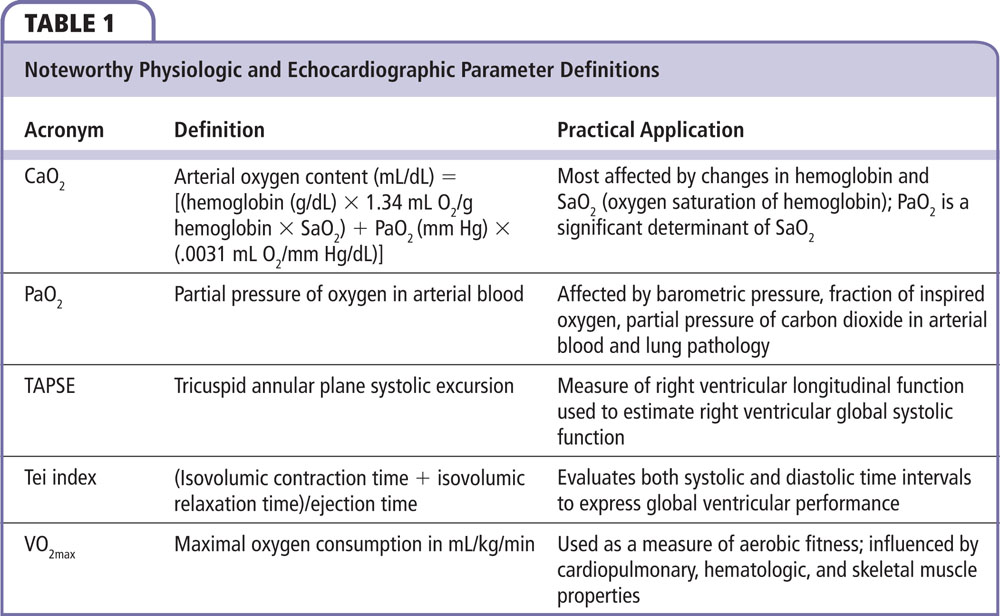
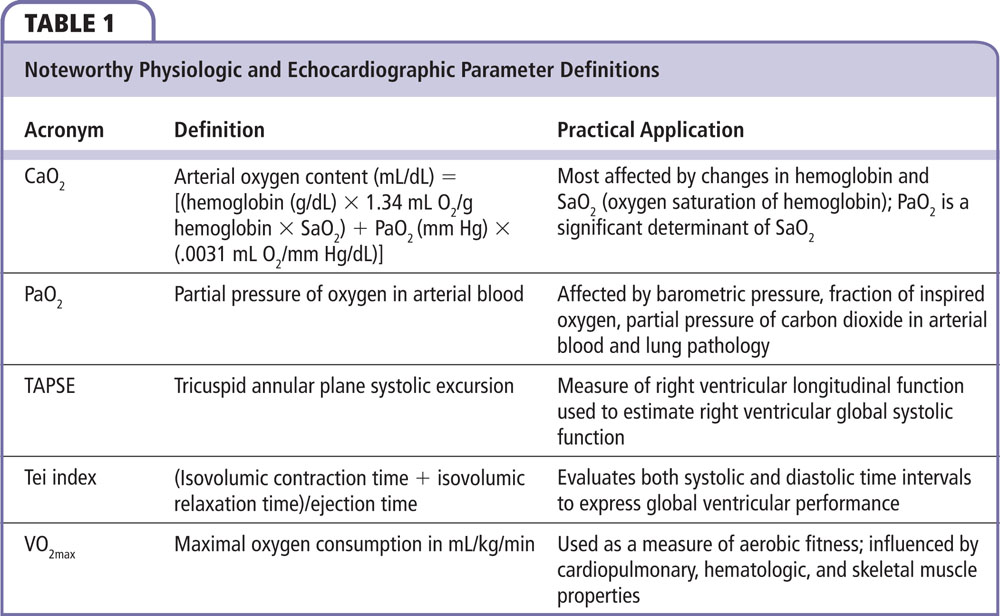
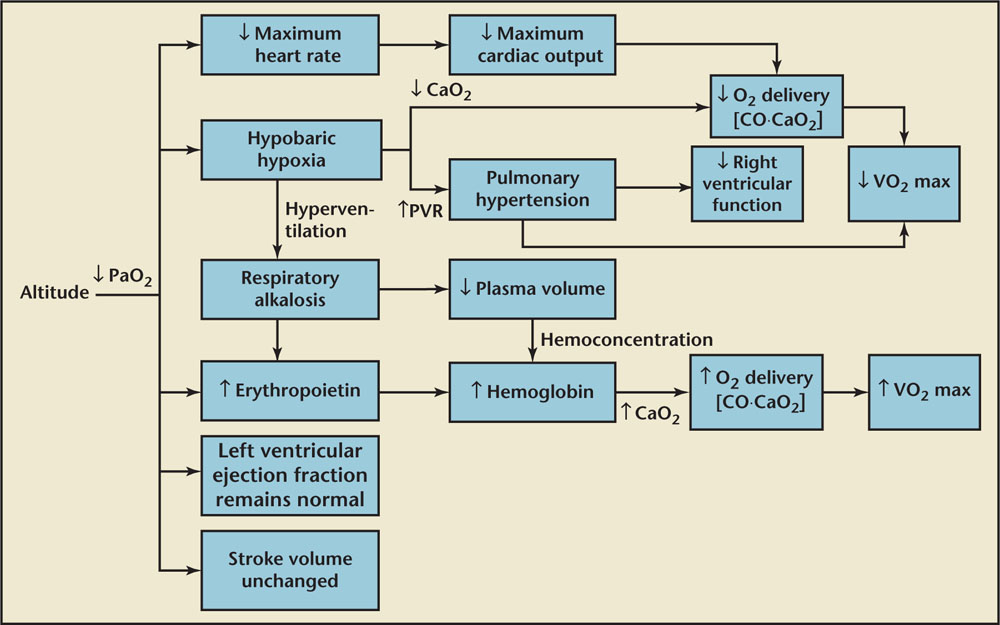
Figure 1. Effects of increased altitude on cardiopulmonary physiology and maximal performance. CaO2, arterial oxygen content; CO, cardiac output; PaO2, partial pressure of oxygen in arterial blood; PVR, pulmonary vascular resistance; VO2max, maximal oxygen consumption.
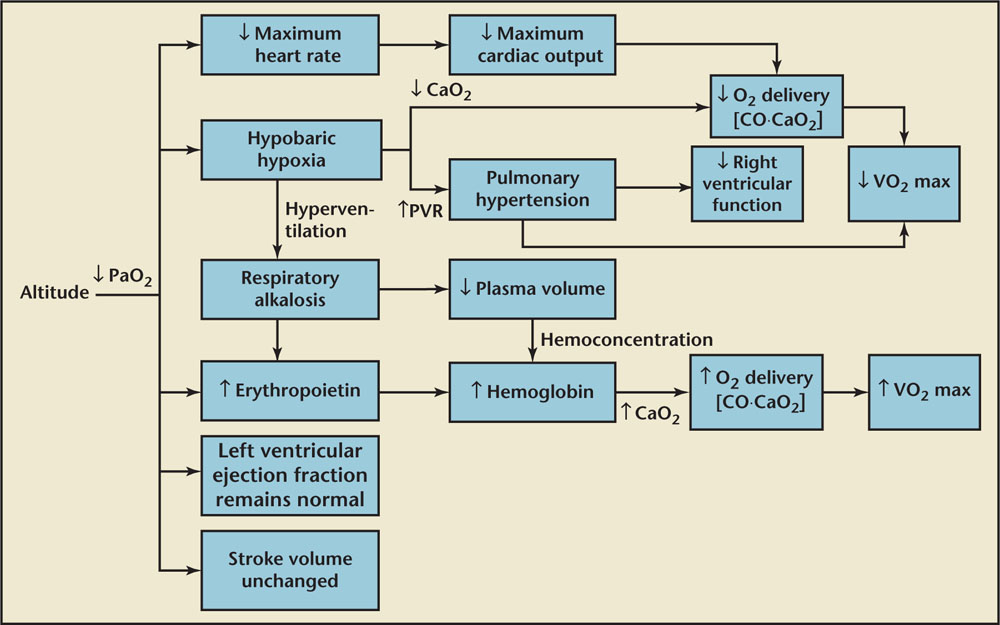
Figure 1. Effects of increased altitude on cardiopulmonary physiology and maximal performance. CaO2, arterial oxygen content; CO, cardiac output; PaO2, partial pressure of oxygen in arterial blood; PVR, pulmonary vascular resistance; VO2max, maximal oxygen consumption.
A study simulating the altitude of Mount Everest showed a decrease in LV volumes but preserved EF that increased with exercise.
Increased altitude and resultant hypoxia has been shown to influence RV function.
… the majority of studies suggest that, in trained athletes, strenuous exercise at increased altitude does not result in LV damage or dysfunction.
Increased efficiency of oxygen extraction is unlikely at increased altitude so the hypoxic myocardium relies on increased oxygen delivery.
Main Points
• Altitude plays an important role in cardiovascular performance and training for athletes. Athletes participating in activities at increased altitude should be aware of high-altitude pulmonary edema (HAPE), as well as the effects of hypoxia on the body.
• During prolonged exposure to increased altitude, the hemoglobin initially increases due to hemoconcentration and eventually due to increased erythropoietin production. The increased hemoglobin functions to increase CaO2 and increase oxygen delivery. This facilitates transport of oxygen to active muscles and increases the maximal volume of oxygen that can be used.
• HAPE is one of most dangerous conditions related to increased altitude exposure among unacclimatized athletes. Athletes should be aware that the acclimatization process does not correlate with the level of physical conditioning. However, after acclimatization, cardiopulmonary capacity is the same as it is at sea level.
• Athletes traditionally lived and trained at increased altitude with the hope of improving exercise performance at sea level. However, results from a study evaluating performance of athletes who (1) lived and trained at low altitudes, (2) lived at moderate altitudes but trained at low altitudes, and (3) lived at moderate altitudes and trained at moderate altitudes challenged the traditional thinking. It was found that “living high and training low” offered the best improvement in performance, as these athletes obtained the benefits of altitude but avoided its training hindrances.
Main Points
• Altitude plays an important role in cardiovascular performance and training for athletes. Athletes participating in activities at increased altitude should be aware of high-altitude pulmonary edema (HAPE), as well as the effects of hypoxia on the body.
• During prolonged exposure to increased altitude, the hemoglobin initially increases due to hemoconcentration and eventually due to increased erythropoietin production. The increased hemoglobin functions to increase CaO2 and increase oxygen delivery. This facilitates transport of oxygen to active muscles and increases the maximal volume of oxygen that can be used.
• HAPE is one of most dangerous conditions related to increased altitude exposure among unacclimatized athletes. Athletes should be aware that the acclimatization process does not correlate with the level of physical conditioning. However, after acclimatization, cardiopulmonary capacity is the same as it is at sea level.
• Athletes traditionally lived and trained at increased altitude with the hope of improving exercise performance at sea level. However, results from a study evaluating performance of athletes who (1) lived and trained at low altitudes, (2) lived at moderate altitudes but trained at low altitudes, and (3) lived at moderate altitudes and trained at moderate altitudes challenged the traditional thinking. It was found that “living high and training low” offered the best improvement in performance, as these athletes obtained the benefits of altitude but avoided its training hindrances.
Altitude plays an important role in cardiovascular performance and training for athletes. Mountaineers, skiers, and sea-level athletes trying to gain an edge by training or living at increased altitude all face potential benefits and harms from this type of training. Athletes participating in activities at increased altitude should be aware of high-altitude pulmonary edema (HAPE), as well as the effects of hypoxia on the body. This article reviews the cardiovascular changes in athletes training at increased altitude, and addresses the potential benefits and harms of increased-altitude training. We adopt previously used parameters to define altitude: low altitude is sea level to 1500 m above sea level, moderate altitude is from 1500 m to 2500 m, and high altitude is above 2500 m.1 The term increased altitude includes both moderate and high altitudes.
Physiologic Changes
As elevation increases, barometric pressure decreases and results in decreased partial pressure of oxygen in arterial blood (PaO2)—60 mm Hg at 2500 m compared with 90 mm Hg at sea level (Table 1).2 The fraction of oxygen content in the air remains unchanged at these altitudes, and the hypoxia is termed hypobaric hypoxia (Figure 1).1
Hyperventilation is the first physiologic change noted during hypoxic exposure at increased altitude. Hyperpnoea, the increased depth of breathing to meet physiologic requirements, occurs above 2500 m.3 The respiratory alkalosis created by hyperventilation is corrected within a few days by increased urinary excretion of bicarbonate.3-5
Due to the decreased arterial oxygen content (CaO2), oxygen delivery—the product of cardiac output and arterial oxygen content—is maintained by an increase in cardiac output.1 At increased altitude, this is achieved by an increase in the baseline heart rate (HR).6 This is supported by the fact that echocardiographic studies done at sea level and 4730 m showed an increase in HR but no increase in stroke volume.7
During prolonged exposure to increased altitude, the hemoglobin initially increases due to hemoconcentration and eventually due to increased erythropoietin production.8 Increases in hemoglobin have been noted to occur at altitudes above 2200 m.9 The increased hemoglobin functions to increase CaO2 and increase oxygen delivery. This facilitates transport of oxygen to active muscles and increases the maximal volume of oxygen that can be used (VO2max, mL/kg/min). Erythropoietin release may correlate with degree of hyperventilation elicited by hypoxia and degree of respiratory alkalosis.10
There is also a decrease in plasma volume from loss of water due to increased ventilation, perspiration, urine output, and decreased oral intake by hypoxia-induced adipsia, the lack of thirst despite dehydration.11 Decreased stroke volume in athletes at increased altitude has been attributed to a reduction in preload.12
Electrocardiogram
Studies have looked at electrocardiograms (ECGs) in athletes with normal sea level ECG results and again after exercise at increased altitude. The most common ECG changes noted are increased P-wave amplitude in the inferior leads, right ventricular (RV) conduction delay, and right axis deviation.13 These changes suggest the presence of RV strain and right atrial enlargement, and may be secondary to the pulmonary hypertension that is seen in individuals at increased altitude. Similar findings have been reproduced when increased altitude is simulated in hypobaric chambers.14 ECG changes revert back to normal values when athletes return to sea level.14
Data on changes to the QT interval are conflicting. There are many factors that influence this parameter, including the autonomic nervous system, hypoxia, hypobarometric pressure, chill, individual differences in acclimatization to high altitude, erythrocytosis, electrolyte changes, and hyperventilation.15 In performance athletes with no known coronary artery disease, ST-segment changes are not appreciable.13
Echocardiography
Many studies have found that left ventricular (LV) ejection fraction (EF) does not change with hypoxia and increased altitude.7,16,17 Studies done in high-altitude ultramarathoners showed a preserved EF and a decrease in LV end-systolic and end-diastolic areas and volumes.18,19 A study simulating the altitude of Mount Everest showed a decrease in LV volumes but preserved EF that increased with exercise. Enhanced contractility was seen in the simulated altitude of 8400 m, suggesting that normal myocardium can tolerate extreme oxygen deprivation.17
Data on diastolic function are conflicting,20 although recent research using speckle-tracking echocardiography suggests that life-long exposure to increased altitudes may affect LV diastolic function.16,21 These studies found a lower LV diastolic untwisting velocity in those who lived at increased altitude, although other parameters of diastolic function were unchanged.16,18 Tissue Doppler imaging has been used to evaluate diastolic function in climbers at 4600 m—the transmitral E/A ratio decreased from 1.4 to 1.1, due to an increase in the A wave.21 The authors proposed that this might reflect an adaptive increase in atrial contraction rather than alteration in diastolic function, although the decreased E/A ratio may be a result of tachycardia experienced at altitude, leading to the fusion of the E and A waves and an increase in A-wave velocity.22 In contrast, tissue Doppler evaluation is not limited in tachycardia and studies that simulated hypoxia in subjects showed no change in the E/e' ratio, suggesting normal diastolic function.23
Increased altitude and resultant hypoxia has been shown to influence RV function.24 RV dilation, decreased tricuspid annular plane systolic excursion, and global hypokinesis with an increase in RV end-systolic and end-diastolic areas have been seen in athletes at increased altitude.16,18,25 In addition, paradoxical septal motion and increase in tricuspid regurgitation jet velocity are noted and correspond to elevated pulmonary artery systolic pressure (PASP).24 Comparison of echocardiograms done at sea level and at 4730 m showed worsening RV diastolic function, impaired RV free-wall longitudinal strain, and increased RV myocardial performance index at increased altitude.7 Myocardial performance, or Tei index, evaluates both systolic and diastolic time intervals to express global ventricular performance as a single value, with higher values signifying worsening function.26 This was seen along with an oxygen saturation that dropped from 98% at sea level to 87% at increased altitude and resulted in significantly increased PASP and pulmonary vascular resistance.27 The authors suggest that hypoxia-induced pulmonary hypertension is a capillary phenomenon because the increase in PASP is associated with an increase in pulmonary vascular resistance.7,28 Repeat echocardiograms done after as little as 18 hours show resolution of these changes.24
Echocardiography in studies evaluating cardiac troponin I (cTnI) and creatine kinase MB during an ultramarathon at increased altitude showed that all subjects had an increase in creatine kinase MB but normal LV function. Only one subject had an elevation in cTnI. That subject also had the highest PASP and the most RV dilation, suggesting that elevations in cTnI may reflect RV and not LV injury.24
Overall, the majority of studies suggest that, in trained athletes, strenuous exercise at increased altitude does not result in LV damage or dysfunction.24 RV dysfunction and elevated pulmonary pressure is seen in athletes at increased altitude, but changes are transient and return to baseline upon return to sea level. However, further investigation is needed to determine the long-term impact of altitude training and whether repeated insults to the pulmonary vasculature and RV have impact on morbidity and mortality. This is especially important in light of publications suggesting an association between endurance training at sea level and arrhythmogenic remodeling of the RV.29,30
HAPE
HAPE is one of most dangerous conditions related to increased altitude exposure among unacclimatized athletes. Athletes should be aware that the acclimatization process does not correlate with the level of physical conditioning. However, after acclimatization, cardiopulmonary capacity is the same as it is at sea level.31 The prevalence of HAPE is influenced by the rate of ascent, overall altitude, and individual susceptibility.32 Approximately 10% of unselected mountaineers reportedly develop HAPE within 24 hours after a rapid ascent to 4500 m.33 Recurrence rates can be as high as 60%.34 HAPE is a noncardiogenic pulmonary edema, as shown by documentation of elevated pulmonary artery pressures in setting of normal left atrial pressures.35 The elevated pulmonary artery pressure is seen in response to hypoxia and can be exaggerated in those who are susceptible.35
Athletes with HAPE have been found to have dilatation of the RV and right atrium and septal shift, and RV tissue Doppler shows apically prominent postsystolic shortening.36 This reflects asynchronous contraction of the RV.6 Echocardiographic studies have compared athletes who have previously developed HAPE with those who have not in an attempt to identify any characteristic findings that may help predict which athletes are more susceptible to developing HAPE.37,38 In one study, PASP was measured in athletes under two conditions: (1) stress echocardiography under normoxic conditions at sea level, and (2) with prolonged exposure to normobaric hypoxia at rest. The athletes who had previously experienced HAPE had an exaggerated increase in PASP to > 45 mm Hg in both stress and hypoxic conditions.37 Similar results were seen in a study evaluating Tei index in subjects with previous history of HAPE. Subjects with a previous history of HAPE had a significantly higher increase in PASP under hypoxic conditions compared with those without a prior history of HAPE. In addition, the RV Tei index increased in those with prior HAPE but remained unchanged in the control subjects.39 Although these results need to be reproduced and validated, echocardiography evaluating changes in PASP and Tei index under stress or simulated hypoxic conditions may be able to identify athletes who are susceptible to HAPE.
Arrhythmias
Many of the arrhythmias seen at increased altitude are benign and related to hypoxia. Marked sinus bradycardia, sinus arrhythmia, and first-degree heart block can be seen in athletes. There is usually loss of the circadian rhythm in HR as well.40 Interestingly, studies have shown that at increased altitude, 80% of athletes can have periodic breathing similar to Cheyne-Stokes respiration.14,41 During the apneic cycles, vagal tone increases and marked sinus bradycardia can be seen with HR as low as 30 beats/min.42
Ventricular arrhythmias in performance athletes at increased altitude are rare. If they do occur, they are unlikely to happen at rest and more likely to happen during or soon after exercise. This may be related to the increased adrenergic activation with acute hypoxia that is needed to increase cardiac output to compensate for the reduced arterial oxygen content. An electrophysiologic study showed that microvolt T-wave alternans, an alternating pattern in the T wave on a surface ECG, correlated with inducible and spontaneous ventricular tachycardia in patients with structural and nonstructural heart disease. Testing in healthy subjects at increased altitude and with exercise was negative for microvolt T-wave alternans despite the increased sympathetic activity. The authors concluded that healthy athletes who exercise at increased altitude are at low risk for ventricular arrhythmias.43 In contrast, known cardiovascular disease is associated with an increased risk for sudden cardiac death during mountaineering and downhill skiing.44
Coronary Arteries
At baseline, coronary extraction of oxygen from the blood is very high, resulting in the coronary sinus partial pressure of oxygen being one of the lowest in the body.11 Increased efficiency of oxygen extraction is unlikely at increased altitude so the hypoxic myocardium relies on increased oxygen delivery. This is achieved by dilation of epicardial coronary arteries resulting in an increase in coronary blood flow.45 With prolonged exposure to increased altitude and hypoxia, coronary blood flow is preserved and an increase in CaO2 is achieved by polycythemia.46 Thus, coronary circulation is well adapted to accommodate hypoxia at increased altitude. Studies showing preserved EF and the lack of ST changes in healthy subjects at increased altitude support these theories. This does not hold true in those with known coronary artery disease, as the physiologic changes associated with increased altitude can result in earlier onset of angina symptoms due to impaired coronary flow reserve and hypoxia.1
Exercise Performance at Increased Altitude
Prior studies have shown that highly trained athletes have significantly improved performance capacity after receiving autologous erythrocyte infusions.47,48 The International Olympic Committee and other sports organizations prohibit blood doping due to its artificial process. As a result, competitive athletes have used altitude training as a means to achieve polycythemia, hoping for improved sea-level performance.49 However, improved performance has not been corroborated by studies of athletes who have trained at increased altitude to achieve polycythemia. Findings showed that, despite achieving polycythemia, VO2max and endurance performance were not increased.50,51
It has been well established that exposure to hypobaric hypoxia decreases VO2max proportionally to the decrease in CaO2 and inspired PaO2.52,53 During initial exposure, athletes have a much greater reduction (80%-85% of sea-level baseline) in their VO2max. With acclimatization, the relationship between oxygen, workload, and oxygen uptake is the same as at sea level, but reaches a peak at a lower VO2max, with some evidence that the VO2max recovers (2%-5% over 2-3 wk).54,55 It has been shown that at increased altitude, elite sea-level athletes are not able to sustain the same degree of high work rates that are necessary to maintain competitive fitness.56
The lower VO2max achieved despite findings of increased erythrocyte volume was initially explained by the decreased maximal HR achieved at increased altitude. Despite studies showing preserved LVEF and myocardial oxygen supply, during maximal exercise at increased altitude, the maximum HR was reduced by 20% and cardiac output and exercise capacity were reduced by 40% to 50%.57 Absence of changes in VO2max by pharmacologic manipulations (atropine, propranolol, isoproterenol) of autonomic nervous system indirectly suggest that decreased chronotropic reserve does not contribute to decreased exercise capacity at increased altitude.11,58 Similarly, it was noted that healthy subjects exercising in hypoxia had a decrease in VO2max, but after nonselective β-adrenergic blockade, there was no change in VO2max despite a significant decrease in peak HR and cardiac output.59,60 The authors suggest that VO2max at increased altitude has many determinants beyond HR and may involve changes in ventilation control, pulmonary pressure with exercise, mitochondrial function, lung gas diffusion, peripheral blood flow, and consequent levels of blood oxygen saturation affecting oxygen delivery and oxygen availability at the tissue level.61
Decreased preload, a result of hypovolemia, has also been evaluated as a factor contributing to the decreased VO2max at increased altitude. However, plasma volume expansion does not consistently increase maximum cardiac output and VO2max.62,63 Pulmonary vasoconstriction induced by hypoxia has also been investigated. These studies used phosphodiesterase inhibitors and found a decrease in PASP and an increase in maximum cardiac output and workload.64 Similarly, studies using endothelin receptor antagonists in subjects at increased altitude also found a significant decrease in PASP, increase in oxygen saturation, and partial restoration of VO2max.65,66
Athletes traditionally lived and trained at increased altitude with the hope of improving exercise performance at sea level. However, results from a study evaluating performance of athletes who (1) lived and trained at low altitudes, (2) lived at moderate altitudes but trained at low altitudes, and (3) lived at moderate altitudes and trained at moderate altitudes challenged the traditional thinking.67 The authors found that “living high and training low” offered the best improvement in performance, as these athletes obtained the benefits of altitude but avoided its training hindrances. Similar findings have been noted in studies in which athletes train low and rested in normobaric hypoxia as means to simulate “living high.”3
Available literature suggests that training at an altitude of 2500 m provides the ideal balance of benefit from altitude training, which is lost at levels below 1500 m, and minimizes excessive harm that is seen when training above 4500 m.4 The optimal time for living at increased altitude has yet to be determined. Performance improvement and erythrocyte volume has been seen in as little as 4 weeks, but some suggest longer periods (eg, 10-12 wk) may allow for complete hematologic adaptation to hypoxia.67,68
Conclusions
The cardiovascular effects of altitude on athletic performance are unavoidable for athletes who participate in sports such as skiing and mountaineering. It appears that certain people may be susceptible to pulmonary hypertension and HAPE at increased altitude, and echocardiography may become useful in screening these athletes prior to climbing to increased altitudes. For sea-level athletes, the optimal strategy for attaining the benefits while minimizing the harms of altitude training still needs to be clarified, although the “live high, train low” approach seems to have the most rationale. Further studies are needed on the long-term effects of such altitude training as repeated, transient episodes of pulmonary hypertension and RV dysfunction may have long-term implications. ![]()
There are no relevant financial disclosures, acknowledgments or conflicts of interest.
References
- Higgins JP, Tuttle T, Higgins JA. Altitude and the heart: is going high safe for your cardiac patient? Am Heart J. 2010;159:25-32.
- Gong H Jr. Exposure to moderate altitude and cardiorespiratory diseases. Cardiologia. 1995;40:477-488.
- Nummela A, Rusko H. Acclimatization to altitude and normoxic training improve 400-m running performance at sea level. J Sports Sci. 2000;18:411-419.
- Hahn AG, Gore CJ. The effect of altitude on cycling performance: a challenge to traditional concepts. Sports Med. 2001;31:533-557.
- Honig A. Peripheral arterial chemoreceptors and reflex control of sodium and water homeostasis. Am J Physiol. 1989;257(6 Pt 2):R1282-R1302.
- Bartsch P, Gibbs JS. Effect of altitude on the heart and the lungs. Circulation. 2007;116:2191-2202.
- Pagé M, Sauvé C, Serri K, et al. Echocardiographic assessment of cardiac performance in response to high altitude and development of subclinical pulmonary edema in healthy climbers. Can J Cardiol. 2013; 29:1277-1284.
- Fisher JW. Recent advances in erythropoietin research. Prog Drug Res. 1993;41:293-311.
- Levine BD, Stray-Gundersen J. A practical approach to altitude training: where to live and train for optimal performance enhancement. Int J Sports Med. 1992;13(suppl 1):S209-S212.
- Miller ME, Rorth M, Parving HH, et al. pH effect on erythropoietin response to hypoxia. N Engl J Med. 1973;288:706-710.
- Naeije R. Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis. 2010;52:456-466.
- Alexander JK, Grover RF. Mechanism of reduced cardiac stroke volume at high altitude. Clin Cardiol. 1983;6:301-303.
- Karliner JS, Sarnquist FF, Graber DJ, et al. The electrocardiogram at extreme altitude: experience on Mt. Everest. Am Heart J. 1985;109(3 Pt 1):505-513.
- Malconian M, Rock P, Hultgren H, et al. The electrocardiogram at rest and exercise during a simulated ascent of Mt. Everest (Operation Everest II). Am J Cardiol. 1990;65:1475-1480.
- Horii M, Takasaki I, Ohtsuka K, et al. Changes of heart rate and QT interval at high altitude in alpinists: analysis by Holter ambulatory electrocardiogram. Clin Cardiol. 1987;10:238-242.
- Dedobbeleer C, Hadefi A, Pichon A, et al. Left ventricular adaptation to high altitude: speckle tracking echocardiography in lowlanders, healthy highlanders and highlanders with chronic mountain sickness. Int J Cardiovasc Imaging. 2015;31:743-752.
- Suarez J, Alexander JK, Houston CS. Enhanced left ventricular systolic performance at high altitude during Operation Everest II. Am J Cardiol. 1987;60: 137-142.
- Stembridge M, Ainslie PN, Hughes MG, et al. Ventricular structure, function, and mechanics at high altitude: chronic remodeling in Sherpa vs. short-term lowlander adaptation. J Appl Physiol (1985). 2014;117:334-343.
- Boussuges A, Molenat F, Burnet H, et al. Operation Everest III (Comex ‘97): modifications of cardiac function secondary to altitude-induced hypoxia. An echocardiographic and Doppler study. Am J Respir Crit Care Med. 2000;161:264-270.
- Bernheim AM, Kiencke S, Fischler M, et al. Acute changes in pulmonary artery pressures due to exercise and exposure to high altitude do not cause left ventricular diastolic dysfunction. Chest. 2007;132:380-387.
- Allemann Y, Rotter M, Hutter D, et al. Impact of acute hypoxic pulmonary hypertension on LV diastolic function in healthy mountaineers at high altitude. Am J Physiol Heart Circ Physiol. 2004;286:H856-H862.
- Armstrong WF, Ryan T. Evaluation of left ventricular diastolic function. In: Feigenbaum’s Echocardiography. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:180.
- Frobert O, Moesgaard J, Toft E, et al. Influence of oxygen tension on myocardial performance. Evaluation by tissue Doppler imaging. Cardiovasc Ultrasound. 2004;2:22.
- Dávila-Román VG, Guest TM, Tuteur PG, et al. Transient right but not left ventricular dysfunction after strenuous exercise at high altitude. J Am Coll Cardiol. 1997;30:468-473.
- de Vries ST, Kleijn SA, van ‘t Hof AW, et al. Impact of high altitude on echocardiographically determined cardiac morphology and function in patients with coronary artery disease and healthy controls. Eur J Echocardiogr. 2010;11:446-450.
- Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26:357-366.
- Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness. Circulation. 2007;115:1132-1146.
- Maggiorini M, Mélot C, Pierre S, et al. High-altitude pulmonary edema is initially caused by an increase in capillary pressure. Circulation. 2001;103: 2078-2083.
- Heidbuchel H, Prior DL, La Gerche A. Ventricular arrhythmias associated with long-term endurance sports: what is the evidence? Br J Sports Med. 2012;46(suppl 1):i44-i50.
- Ector J, Ganame J, van der Merwe N, et al. Reduced right ventricular ejection fraction in endurance athletes presenting with ventricular arrhythmias: a quantitative angiographic assessment. Eur Heart J. 2007;28:345-353.
- Campos AL, Costa RV. Physical activity at moderate and high altitudes. Cardiovascular and respiratory morbidity. Arq Bras Cardiol. 1999;73:113-128.
- Bärtsch P, Mairbäurl H, Maggiorini M, Swenson ER. Physiological aspects of high-altitude pulmonary edema. J Appl Physiol (1985). 2005;98:1101-1110.
- Bartsch P, Vock P, Maggiorini M, et al. Respiratory symptoms, radiographic and physiologic correlations at high altitude. In: Sutton JR, Coates G, Remmers JE, eds. Hypoxia: The Adaptation. Toronto, Canada: B.C. Decker; 1990:241-245.
- Bärtsch P, Maggiorini M, Ritter M, et al. Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1991;325:1284-1289.
- Penaloza D, Sime F. Circulatory dynamics during high altitude pulmonary edema. Am J Cardiol. 1969;23: 369-378.
- Huez S, Faoro V, Vachiéry JL, et al. Images in cardiovascular medicine. High-altitude-induced right-heart failure. Circulation. 2007;115:e308-e309.
- Grünig E, Mereles D, Hildebrandt W, et al. Stress Doppler echocardiography for identification of susceptibility to high altitude pulmonary edema. J Am Coll Cardiol. 2000;35:980-987.
- Eldridge MW, Podolsky A, Richardson RS, et al. Pulmonary hemodynamic response to exercise in subjects with prior high-altitude pulmonary edema. J Appl Physiol (1985). 1996;81:911-921.
- Hanaoka M, Kogashi K, Droma Y, et al. Myocardial performance index in subjects susceptible to high-altitude pulmonary edema. Intern Med. 2011;50: 2967-2973.
- Houston CS. Altitude illness. The dangers of the heights and how to avoid them. Postgrad Med. 1983;74:231-248.
- Sutton JR, Houston CS, Mansell AL, et al. Effect of acetazolamide on hypoxemia during sleep at high altitude. N Engl J Med. 1979;301:1329-1331.
- Cummings P, Lysgaard M. Cardiac arrhythmia at high altitude. West J Med. 1981;135:66-68.
- Narayan SM. T-wave alternans and the susceptibility to ventricular arrhythmias. J Am Coll Cardiol. 2006; 47:269-281.
- Burtscher M, Pachinger O, Mittleman MA, Ulmer H. Prior myocardial infarction is the major risk factor associated with sudden cardiac death during downhill skiing. Int J Sports Med. 2000;21:613-615.
- Wyss CA, Koepfli P, Fretz G, et al. Influence of altitude exposure on coronary flow reserve. Circulation. 2003;108:1202-1207.
- Grover RF, Lufschanowski R, Alexander JK. Alterations in the coronary circulation of man following ascent to 3,100 m altitude. J Appl Physiol. 1976;41: 832-838.
- Brien AJ, Simon TL. The effects of red blood cell infusion on 10-km race time. JAMA. 1987;257:2761-2765.
- Berglund B, Hemmingson P. Effect of reinfusion of autologous blood on exercise performance in cross-country skiers. Int J Sports Med. 1987;8:231-233.
- Dick FW. Training at altitude in practice. Int J Sports Med. 1992;13(suppl 1):S203-S206.
- Hansen JE, Vogel JA, Stelter GP, Consolazio CF. Oxygen uptake in man during exhaustive work at sea level and high altitude. J Appl Physiol. 1967;23: 511-522.
- Adams WC, Bernauer EM, Dill DB, Bomar JB Jr. Effects of equivalent sea-level and altitude training on VO2max and running performance. J Appl Physiol. 1975;39:262-266.
- Mollard P, Woorons X, Letournel M, et al. Determinant factors of the decrease in aerobic performance in moderate acute hypoxia in women endurance athletes. Respir Physiol Neurobiol. 2007;159:178-186.
- Lawler J, Powers SK, Thompson D. Linear relationship between VO2max and VO2max decrement during exposure to acute hypoxia. J Appl Physiol (1985). 1988;64:1486-1492.
- Daniels J, Oldridge N. The effects of alternate exposure to altitude and sea level on world-class middle-distance runners. Med Sci Sports. 1970;2:107-112.
- Hartley LH, Alexander JK, Modelski M, Grover RF. Subnormal cardiac output at rest and during exercise in residents at 3,100 m altitude. J Appl Physiol. 1967;23:839-848.
- Saltin B. Aerobic and anaerobic work capacity at 2300 meters. Med Thorac. 1967;24:205-210.
- Sutton JR, Reeves JT, Wagner PD, et al. Operation Everest II: oxygen transport during exercise at extreme simulated altitude. J Appl Physiol (1985). 1988;64:1309-1321.
- Bogaard HJ, Hopkins SR, Yamaya Y, et al. Role of the autonomic nervous system in the reduced maximal cardiac output at altitude. J Appl Physiol (1985). 2002;93:271-279.
- Hopkins SR, Bogaard HJ, Niizeki K, et al. Beta-adrenergic or parasympathetic inhibition, heart rate and cardiac output during normoxic and acute hypoxic exercise in humans. J Physiol. 2003;550(Pt 2): 605-616.
- Moore LG, Cymerman A, Huang SY, et al. Propranolol does not impair exercise oxygen uptake in normal men at high altitude. J Appl Physiol (1985). 1986;61:1935-1941.
- Mollard P, Woorons X, Letournel M, et al. Role of maximal heart rate and arterial O2 saturation on the decrement of VO2max in moderate acute hypoxia in trained and untrained men. Int J Sports Med. 2007;28:186-192.
- Calbet JA, Rådegran G, Boushel R, et al. Plasma volume expansion does not increase maximal cardiac output or VO2max in lowlanders acclimatized to altitude. Am J Physiol Heart Circ Physiol. 2004;287: H1214-H1224.
- Alexander JK, Hartley LH, Modelski M, Grover RF. Reduction of stroke volume during exercise in man following ascent to 3,100 m altitude. J Appl Physiol. 1967;23:849-858.
- Ghofrani HA, Reichenberger F, Kohstall MG, et al. Sildenafil increased exercise capacity during hypoxia at low altitudes and at Mount Everest base camp: a randomized, double-blind, placebo-controlled crossover trial. Ann Intern Med. 2004;141:169-177.
- Faoro V, Boldingh S, Moreels M, et al. Bosentan decreases pulmonary vascular resistance and improves exercise capacity in acute hypoxia. Chest. 2009;135:1215-1222.
- Naeije R, Huez S, Lamotte M, et al. Pulmonary artery pressure limits exercise capacity at high altitude. Eur Respir J. 2010;36:1049-1055.
- Levine BD, Stray-Gundersen J. “Living high-training low”: effect of moderate-altitude acclimatization with low-altitude training on performance. J Appl Physiol (1985). 1997;83:102-112.
- Berglund B. High-altitude training. Aspects of haematological adaptation. Sports Med. 1992;14:289-303.