Myocardial Infarction Related to Trauma
Carlos E. Velasco, MD, Mahir Patel, MD, Jaime Mogollon, MD, Jerrold M. Grodin, MD, Robert C. Stoler, MD
Baylor Jack and Jane Hamilton Heart and Vascular Hospital and Baylor University Medical Center, Dallas, TX
Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare. A previously healthy man developed acute MI shortly after a motor vehicle accident. This case illustrates the feasibility of primary percutaneous coronary intervention for acute MI due to complete coronary artery occlusion related to trauma, including the use of manual thrombectomy, stents, and dual antiplatelet therapy. This approach requires the intervention of a multidisciplinary team in a Level 1 trauma center that can rapidly evaluate the patient and rule out other life-threatening injuries that could preclude antiplatelet therapy.
[ Rev Cardiovasc Med. 2015;16(4):261-264 doi: 10.3909/ricm0795 ]
© 2016 MedReviews®, LLC
Myocardial Infarction Related to Trauma
Carlos E. Velasco, MD, Mahir Patel, MD, Jaime Mogollon, MD, Jerrold M. Grodin, MD, Robert C. Stoler, MD
Baylor Jack and Jane Hamilton Heart and Vascular Hospital and Baylor University Medical Center, Dallas, TX
Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare. A previously healthy man developed acute MI shortly after a motor vehicle accident. This case illustrates the feasibility of primary percutaneous coronary intervention for acute MI due to complete coronary artery occlusion related to trauma, including the use of manual thrombectomy, stents, and dual antiplatelet therapy. This approach requires the intervention of a multidisciplinary team in a Level 1 trauma center that can rapidly evaluate the patient and rule out other life-threatening injuries that could preclude antiplatelet therapy.
[ Rev Cardiovasc Med. 2015;16(4):261-264 doi: 10.3909/ricm0795 ]
© 2016 MedReviews®, LLC
Myocardial Infarction Related to Trauma
Carlos E. Velasco, MD, Mahir Patel, MD, Jaime Mogollon, MD, Jerrold M. Grodin, MD, Robert C. Stoler, MD
Baylor Jack and Jane Hamilton Heart and Vascular Hospital and Baylor University Medical Center, Dallas, TX
Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare. A previously healthy man developed acute MI shortly after a motor vehicle accident. This case illustrates the feasibility of primary percutaneous coronary intervention for acute MI due to complete coronary artery occlusion related to trauma, including the use of manual thrombectomy, stents, and dual antiplatelet therapy. This approach requires the intervention of a multidisciplinary team in a Level 1 trauma center that can rapidly evaluate the patient and rule out other life-threatening injuries that could preclude antiplatelet therapy.
[ Rev Cardiovasc Med. 2015;16(4):261-264 doi: 10.3909/ricm0795 ]
© 2016 MedReviews®, LLC
KEY WORDS
Acute ST segment elevation myocardial infarction • Chest trauma • Primary percutaneous coronary intervention
KEY WORDS
Acute ST segment elevation myocardial infarction • Chest trauma • Primary percutaneous coronary intervention
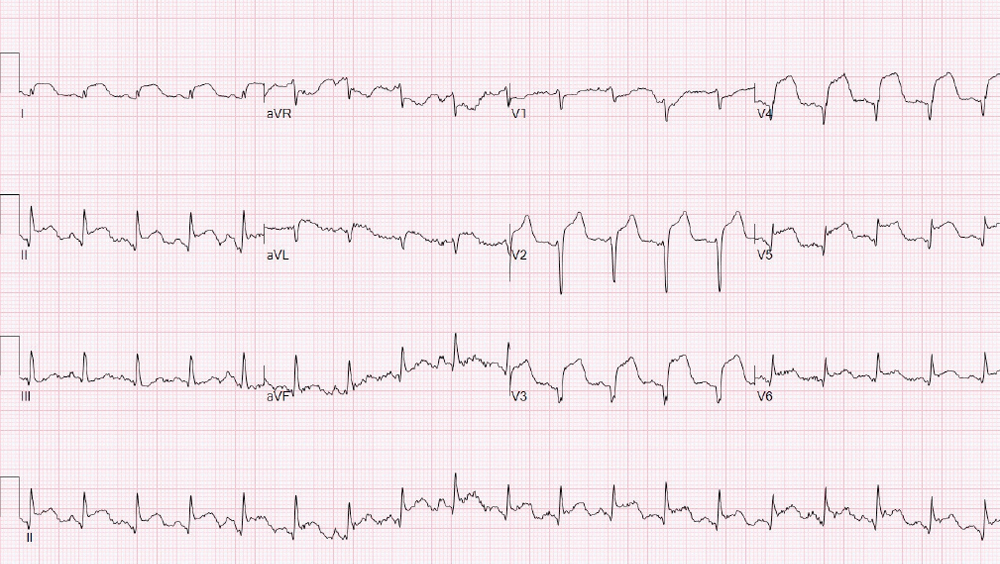
Figure 1. Electrocardiogram showed sinus tachycardia with marked ST segment elevation in the anterior and lateral leads.
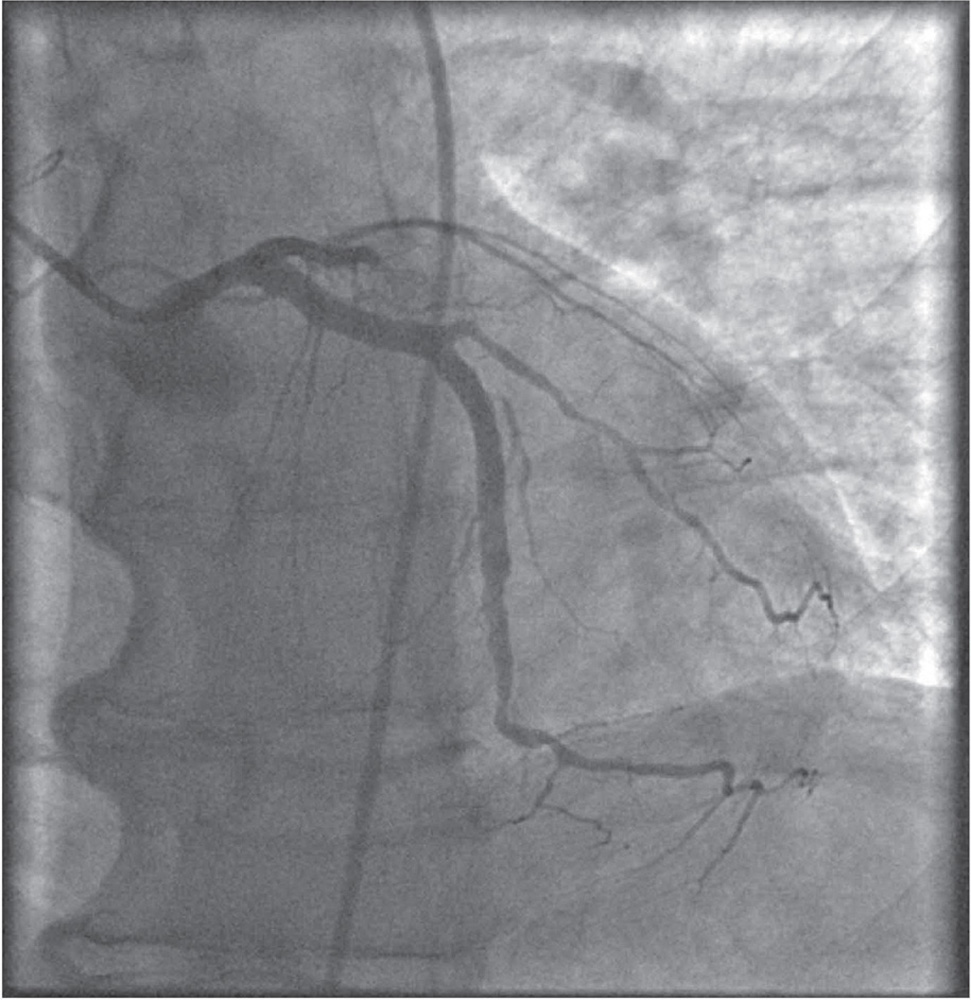
Figure 2. Coronary angiogram showing complete occlusion of the proximal left anterior descending artery, as well as mild to moderate disease in the left circumflex artery.

Figure 3. Coronary angiogram after primary percutaneous coronary intervention, showing Thrombolysis in Myocardial Infarction grade III distal flow.
Direct trauma to the coronary arteries leading to intracoronary thrombosis, particularly the LAD, has long been considered a mechanism of trauma-related infarction.
Main Points
• Most cardiac complications related to trauma are myocardial contusions, arrhythmias, or pericardial effusions. Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare. Transportationrelated trauma is a leading mechanism of injury, especially when blunt cardiac injury occurs.
• It is critical to differentiate acute MI from myocardial contusion.
• Most patients with electrocardiographic evidence of ST segment elevation after trauma must undergo emergency cardiac catheterization and percutaneous coronary intervention should be considered if indicated and feasible.
• Use of computed tomography scanning provides a fast way to rule out other complications, including findings suggestive of serious bleeding.
Main Points
• Most cardiac complications related to trauma are myocardial contusions, arrhythmias, or pericardial effusions. Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare. Transportationrelated trauma is a leading mechanism of injury, especially when blunt cardiac injury occurs.
• It is critical to differentiate acute MI from myocardial contusion.
• Most patients with electrocardiographic evidence of ST segment elevation after trauma must undergo emergency cardiac catheterization and percutaneous coronary intervention should be considered if indicated and feasible.
• Use of computed tomography scanning provides a fast way to rule out other complications, including findings suggestive of serious bleeding.
Most cardiac complications related to trauma are myocardial contusions, arrhythmias, or pericardial effusions. Myocardial infarction (MI) secondary to acute coronary occlusion related to trauma is rare, and without mention as a complication of traumatic injury in some textbooks. Recognition of this problem is important, as MI may lead to increased morbidity and mortality in trauma patients. Transportation-related trauma is a leading mechanism of injury, especially when blunt cardiac injury occurs.1
The challenges to performing primary percutaneous coronary intervention (PCI) on these patients include prompt diagnosis, decisions on placement of intracoronary stents, and need of dual antiplatelet therapy (DAPT) in a patient with multiorgan trauma who may also require urgent noncardiac surgery. Here we describe a case of a previously healthy man who developed acute MI shortly after a motor vehicle accident.
Case Report
A previously healthy 48-year-old white man had major trauma after a vehicle fleeing the police collided with his truck from the right side. The accident was witnessed by the police and paramedics arrived promptly. It took 15 minutes to extricate him from the truck, and he was brought to Baylor University Medical Center (Dallas, TX), a Level 1 trauma center. While in the ambulance, he complained of shortness of breath and chest pain. Immediately upon arrival to the emergency room, a computed tomography (CT) scan showed right tension pneumothorax with mediastinal shift. A chest tube was then inserted without significant improvement of his symptoms. His heart rate then increased to 160 beats/min, and an electrocardiogram showed sinus tachycardia with marked ST segment elevation in the anterior (anteroseptal and anterolateral) and lateral leads (Figure 1). The patient was taken to the cardiac catheterization laboratory, where cine coronary angiography showed acute occlusion of the proximal left anterior descending artery (LAD), probably secondary to dissection and/or thrombosis (Figure 2); other arteries had moderate diffuse disease. Heparin, 3000 U, and aspirin, 325 mg, were given. At the beginning of the procedure, no other medications were given due to concerns of possible intra-abdominal hematoma, which was suggested by the initial CT scan. Export manual thrombectomy followed by primary PCI of the LAD was performed, resulting in prompt reperfusion; however, attempting it as a balloon-only procedure was unsuccessful due to reocclusion of the artery after removal of the balloon, despite the coronary guidewire still being in place. Therefore, a 3.0 × 28 mm VeriFLEX™ (Boston Scientific, Marlborough, MA) bare metal stent was placed, obtaining Thrombolysis in Myocardial Infarction grade III distal flow (Figure 3). A trauma surgery team was consulted to reassess the CT scan of the abdomen, given the presence of possible pelvic hematoma; surgeons approved the use of a second antiplatelet agent and clopidogrel, 600 mg, was given at that time. The patient had an uneventful recovery but was left with a left ventricular function of 30% with anterolateral akinesis, later requiring placement of an implantable cardioverter defibrillator.
Discussion
MI related to acute coronary occlusion secondary to closed-chest trauma is very rare. Our patient had previously undiagnosed moderate coronary artery disease and infarction was likely related to sudden plaque rupture secondary to severe chest contusion. Many patients with heart injury related to trauma are labeled as having myocardial contusion, diagnosed mainly based on the presence of abnormal cardiac enzymes.2
A case series demonstrated that the most common mechanism of injury in individuals diagnosed with acute MI related to trauma is falls; however, in individuals 45 years or younger, the leading mechanism of injury is transportation related.1 Direct trauma to the coronary arteries leading to intracoronary thrombosis, particularly the LAD, has long been considered a mechanism of trauma-related infarction.3-5
As stated by Guo and colleagues,6 a key point is to differentiate acute MI from myocardial contusion. For practical purposes most patients with electrocardiographic evidence of ST segment elevation after trauma must undergo emergency cardiac catheterization and PCI should be considered if indicated and feasible.
The first report of PCI treatment of acute MI secondary to blunt chest trauma was published in 1996 about a patient with right coronary artery dissection who was treated with coronary angioplasty without stenting.7 The LAD is more commonly involved, likely due to its proximity to the chest wall.7
It is possible that the presence of some atherosclerotic disease makes these patients more susceptible to coronary dissection due to trauma by providing a hinge point for intimal tear related to shear force, ultimately leading to acute thrombosis and myocardial ischemia. Also, a patient involved in sudden trauma without significant chronic coronary artery disease could have an MI without significant recruitment of collateral circulation, which could therefore result in a larger infarct size. This could explain why our patient left the hospital with severe left ventricular systolic dysfunction despite having had successful coronary reperfusion approximately 65 minutes after the onset of his chest injury.
Maenza and colleagues2 published a meta-analysis of blunt cardiac trauma, including prospective and retrospective studies, which cited a number of complications of trauma, including ventricular and supraventricular arrhythmias, electrocardiographic abnormalities, MI, congestive heart failure, hypotension, pericardial effusion, atrioventricular block, and intracardiac thrombus. Of importance, MI is not limited to chest trauma, but could be a consequence of pelvic or abdominal injury, as well.1
Our case illustrates the feasibility of manual thrombectomy and primary PCI for acute MI due to coronary thrombosis related to trauma, including the use of stents and DAPT. This approach requires the intervention of a multidisciplinary team in a Level 1 trauma center that can rapidly evaluate the patient and rule out other life-threatening injuries, which could preclude antiplatelet therapy. Widespread use of CT scanning provides a fast way to rule out other problems, including findings suggestive of serious bleeding.
We believe that a conservative approach with a balloon-only procedure is reasonable, given the uncertainty regarding the presence of significant injury in other organs at the time of admission, some of which could require emergency surgery and preclude DAPT. When the balloon-only result is not optimal, then stent placement is mandatory. Currently, it is reasonable to limit these procedures to bare metal stents, which could allow a brief course of DAPT, if needed. ![]()
References
- Ismailov RM, Ness RB, Weiss HB, et al. Trauma associated with acute myocardial infarction in a multi-state hospitalized population. Int J Cardiol. 2005;105:141-146.
- Maenza RL, Seaberg D, D’Amico F. A meta-analysis of blunt cardiac trauma: ending myocardial confusion. Am J Emerg Med. 1996;14:237-241.
- Lehmus HJ, Sundquist AB, Giddings LW. Coronary thrombosis with myocardial infarction secondary to nonpenetrating injury of the chest wall. Am Heart J. 1954;47:470-473.
- Jokl E, Greenstein J. Fatal coronary sclerosis in a boy of 10 years. Lancet. 1944;244:659-662.
- Parmley LF, Manion WC, Mattingly TW. Nonpenetrating traumatic injury of the heart. Circulation. 1958;18:371-396.
- Guo H, Chi J, Yuan M, Qiu Y. Acute myocardial infarction caused by blunt chest trauma: a case report. Int J Cardiol. 2011;149:e80-e81.
- Marcum JL, Booth DC, Sapin PM. Acute myocardial infarction caused by blunt chest trauma: successful treatment by direct coronary angiography. Am Heart J. 1996;132:1275-1277.