Home Telemedicine in Heart Failure: A Pilot Study of Integrated Telemonitoring and Virtual Provider Appointments
Shadi Idris, MD, George Degheim, MD, Wael Ghalayini, MD, Timothy R. Larsen, DO, Davar Nejad, MD, Shukri David, MD
Department of Internal Medicine, Section of Cardiology, Providence Hospital and Medical Center, Southfield, MI
Congestive heart failure is a significant cause of hospitalization, rehospitalization, and death. Reducing hospital readmission rates is a national priority. Various telemonitoring devices and programs have been developed to help meet this goal. The Health Connect system incorporates monitoring of physiologic data with regular virtual provider appointments. The Health Connect system integrates traditional telemedicine with virtual provider appointments. Virtual appointments empower patients to advocate for their own health by providing numerous opportunities for education and feedback. In addition to early identification of impending decompensation, virtual appointments allow providers to address noncompliance, which is a major factor driving poor outcomes. Further research is required to confirm the benefit of the Health Connect system.
[Rev Cardiovasc Med. 2015; 16(2):156-162 doi: 10.3909/ricm0760]
© 2015 MedReviews®, LLC
Home Telemedicine in Heart Failure: A Pilot Study of Integrated Telemonitoring and Virtual Provider Appointments
Shadi Idris, MD, George Degheim, MD, Wael Ghalayini, MD, Timothy R. Larsen, DO, Davar Nejad, MD, Shukri David, MD
Department of Internal Medicine, Section of Cardiology, Providence Hospital and Medical Center, Southfield, MI
Congestive heart failure is a significant cause of hospitalization, rehospitalization, and death. Reducing hospital readmission rates is a national priority. Various telemonitoring devices and programs have been developed to help meet this goal. The Health Connect system incorporates monitoring of physiologic data with regular virtual provider appointments. The Health Connect system integrates traditional telemedicine with virtual provider appointments. Virtual appointments empower patients to advocate for their own health by providing numerous opportunities for education and feedback. In addition to early identification of impending decompensation, virtual appointments allow providers to address noncompliance, which is a major factor driving poor outcomes. Further research is required to confirm the benefit of the Health Connect system.
[Rev Cardiovasc Med. 2015; 16(2):156-162 doi: 10.3909/ricm0760]
© 2015 MedReviews®, LLC
Home Telemedicine in Heart Failure: A Pilot Study of Integrated Telemonitoring and Virtual Provider Appointments
Shadi Idris, MD, George Degheim, MD, Wael Ghalayini, MD, Timothy R. Larsen, DO, Davar Nejad, MD, Shukri David, MD
Department of Internal Medicine, Section of Cardiology, Providence Hospital and Medical Center, Southfield, MI
Congestive heart failure is a significant cause of hospitalization, rehospitalization, and death. Reducing hospital readmission rates is a national priority. Various telemonitoring devices and programs have been developed to help meet this goal. The Health Connect system incorporates monitoring of physiologic data with regular virtual provider appointments. The Health Connect system integrates traditional telemedicine with virtual provider appointments. Virtual appointments empower patients to advocate for their own health by providing numerous opportunities for education and feedback. In addition to early identification of impending decompensation, virtual appointments allow providers to address noncompliance, which is a major factor driving poor outcomes. Further research is required to confirm the benefit of the Health Connect system.
[Rev Cardiovasc Med. 2015; 16(2):156-162 doi: 10.3909/ricm0760]
© 2015 MedReviews®, LLC
KEY WORDS
Telemedicine • Heart failure • Rehospitalization
KEY WORDS
Telemedicine • Heart failure • Rehospitalization
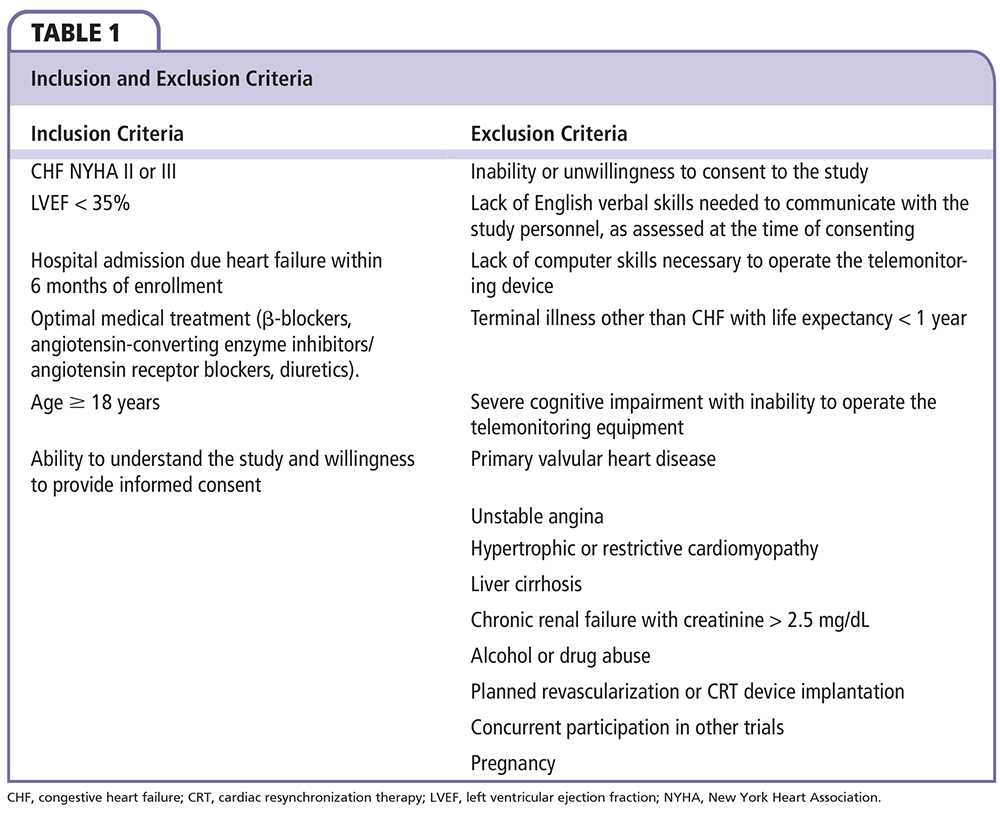
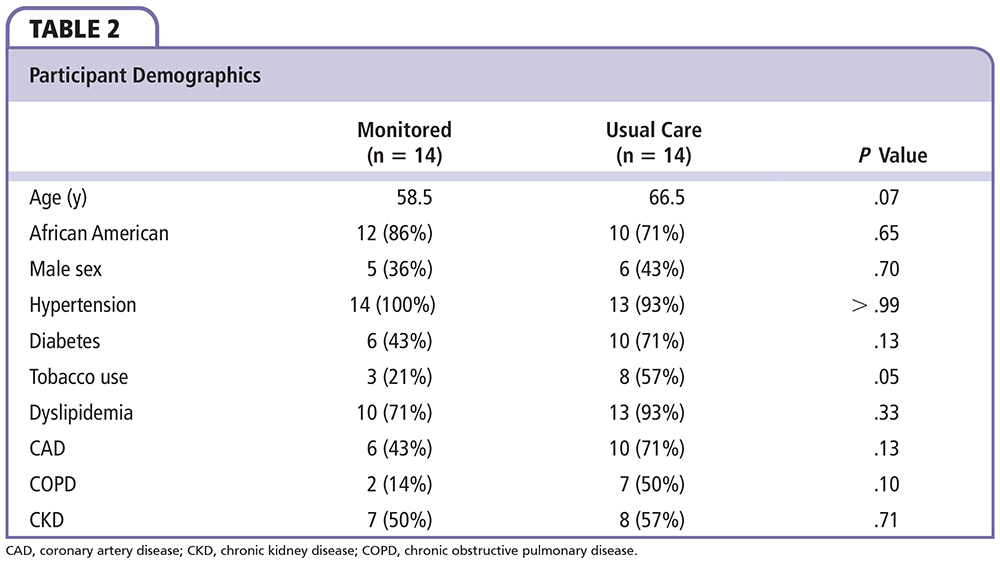
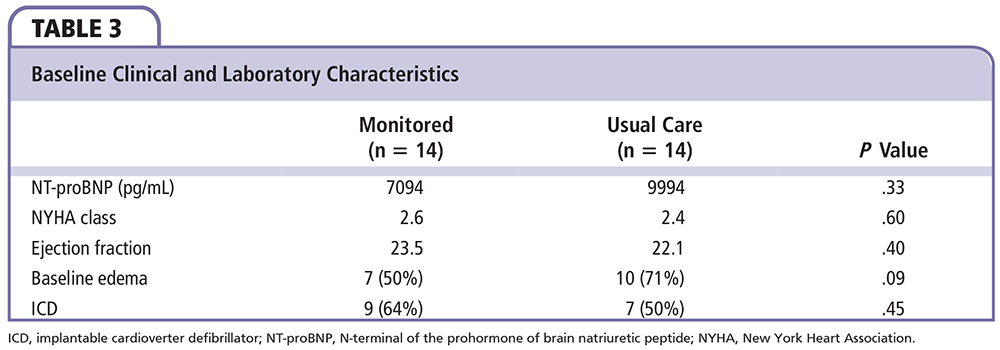
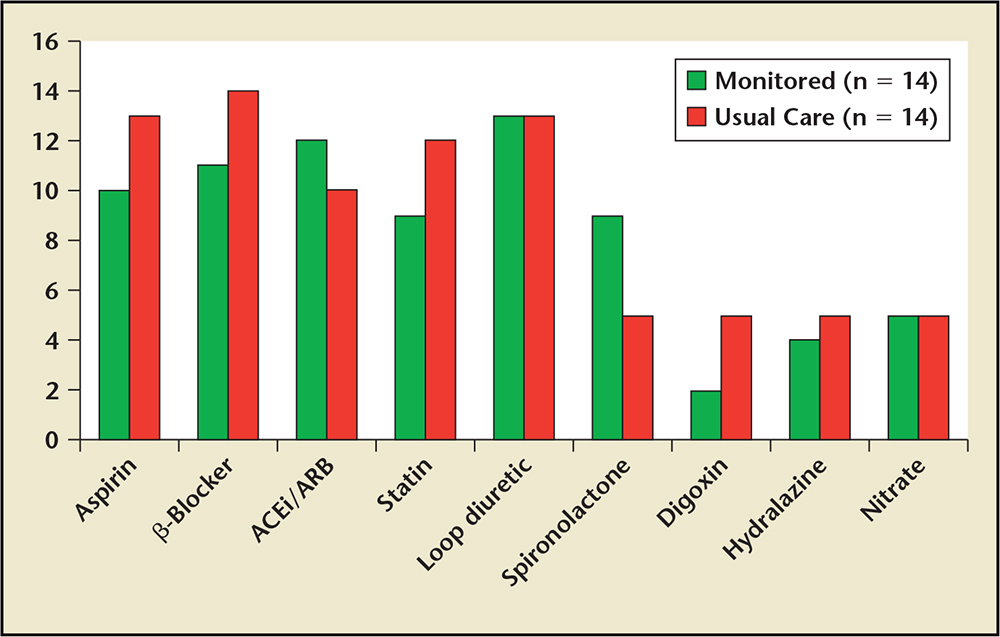
Figure 1. Discharge medications between participants in both arms of the study. ACEi, angiotensinconverting enzyme inhibitor; ARB, angiotensin-converting enzyme.
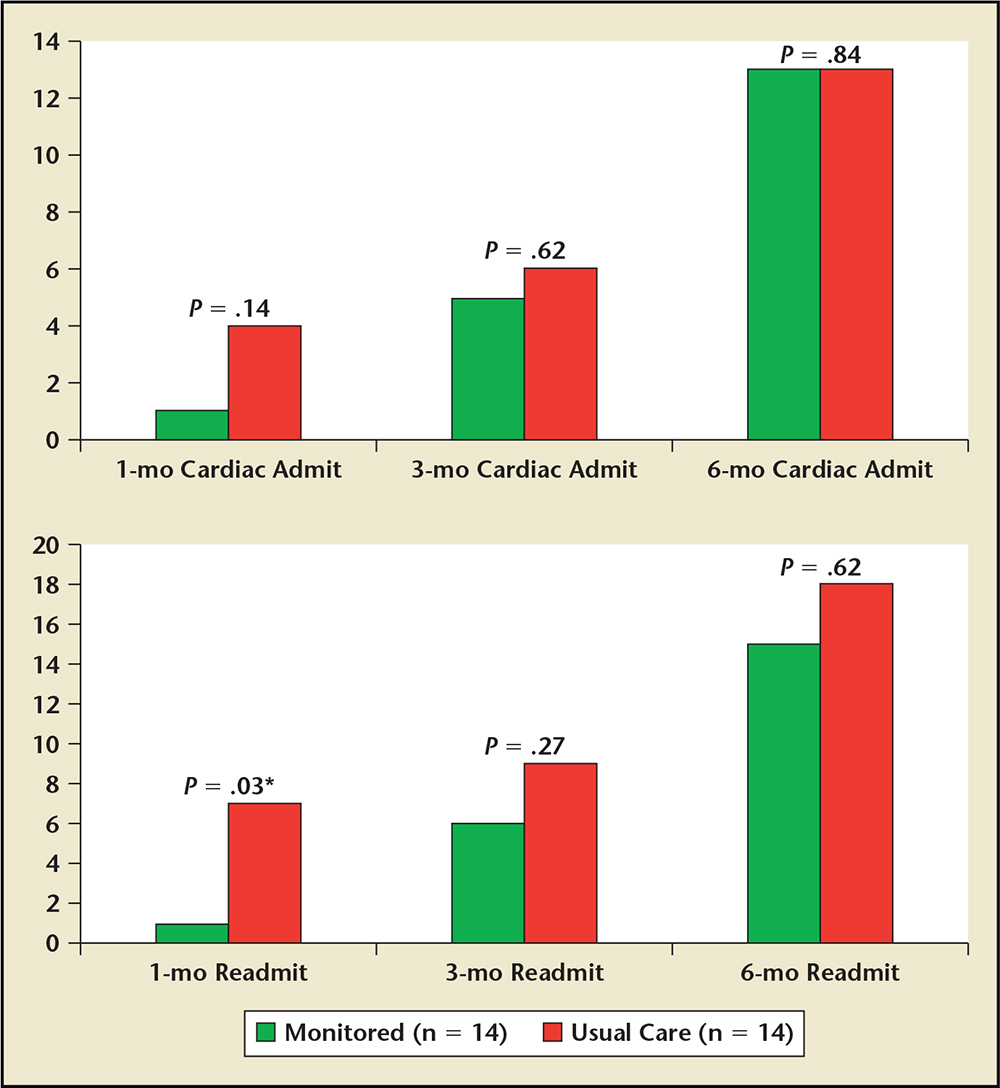
Figure 2. Clinical outcomes and hospital readmission at 1, 3, and 6 months. Readmissions were further classified as cardiac (top) or all causes (bottom). Admit, admission; Readmit, readmission.
Virtual appointments foster an environment that encourages patient empowerment… Virtual appointments ... enable clinicians to better determine the most appropriate intervention.
Main Points
• Congestive heart failure (CHF) is one of the most common causes of hospitalization and readmission in the United States. Despite progress in reducing CHF-related mortality, hospitalizations for CHF remain frequent and rates of readmissions continue to rise. Reducing hospital readmission rates is a national priority.
• Telemedicine and telemonitoring technologies have been developed to include a wide range of possible patient–healthcare provider interactions. In the home setting, telemonitoring has been utilized for several chronic conditions. Among cardiovascular diseases, heart failure stands out as being suitable for the utilization of telemedicine technology.
• An important benefit of telemonitoring appears to be related to patient empowerment. Patients gain insight and awareness into their disease when they are directly involved in the care process. Virtual appointments foster an environment that encourages patient empowerment by offering ideal opportunities for this type of interaction, and truly transform basic telemonitoring into telemedicine.
Main Points
• Congestive heart failure (CHF) is one of the most common causes of hospitalization and readmission in the United States. Despite progress in reducing CHF-related mortality, hospitalizations for CHF remain frequent and rates of readmissions continue to rise. Reducing hospital readmission rates is a national priority.
• Telemedicine and telemonitoring technologies have been developed to include a wide range of possible patient–healthcare provider interactions. In the home setting, telemonitoring has been utilized for several chronic conditions. Among cardiovascular diseases, heart failure stands out as being suitable for the utilization of telemedicine technology.
• An important benefit of telemonitoring appears to be related to patient empowerment. Patients gain insight and awareness into their disease when they are directly involved in the care process. Virtual appointments foster an environment that encourages patient empowerment by offering ideal opportunities for this type of interaction, and truly transform basic telemonitoring into telemedicine.
Congestive heart failure (CHF) is one of the most common causes of hospitalization and readmission in the United States.1 It is considered an epidemic, and is a staggering clinical and public health problem. CHF has been associated with significant mortality, morbidity, and healthcare expenditures, particularly among those aged ≥ 65 years. Despite progress in reducing CHF-related mortality, hospitalizations for CHF remain frequent and rates of readmissions continue to rise.2
Reducing hospital readmission rates is a national priority, but there is currently a lack of evidence supporting strategies to effectively do so.3 Some strategies include optimizing evidence-based drug and device therapies, addressing causes of CHF exacerbations, treating comorbid conditions, and improving care management and coordination.4 Basoor and colleagues5 demonstrated that effective discharge instructions (ie, appropriate dose up-titration, education regarding heart failure monitoring, and strict outpatient follow-up) can prevent CHF read-mission. All of these strategies are likely underutilized throughout the county. Ketterer and colleagues6 identified the presence of psychiatric disorders and cognitive impairment as possible risk factors for early readmission.
Interest in telemonitoring interventions to reduce hospital read-missions in patients with CHF is growing.7 The objective of this study was to determine the practicality and acceptability of a novel home telemonitoring system.
Methods
Patients with systolic heart failure, New York Heart Association class II/III symptoms, and left ventricular ejection fraction < 35% were included (N = 28). The patients were randomized in a 1:1 ratio to the control or monitored group. The control group received standard care, consisting of optimal medical therapy with a β-adrenergic antagonist, angiotensin-converting enzyme inhibitors, aldosterone receptor antagonists, vasodilators, and diuretics dosed to achieve a euvolemic state, resting heart rate < 100 beats/min, and blood pressure < 140/90 mm Hg. Medications were chosen and dosed at the discretion of the patients’ primary cardiologist. The monitored group received standard care in addition to daily remote monitoring of blood pressure, heart rate, oxygen saturation, and weight via the Health Connect telemonitoring system for 3 months. Furthermore, the monitored group received weekly video calls to discuss care issues, answer questions, and monitor compliance with medication regimens and office visits. Due to the nature of the study it was not possible to blind the caregivers or participants. Study participants were included if they met the conditions listed in Table 1. Study participants were excluded from the study if they met one or more of the conditions listed in Table 1.
Patient weight was charted and monitored for a change > 10%. Patients were typically scheduled for office-based follow-up at 2 weeks, 3 months, and 6 months after the initial consultation. Patient data were reviewed by a physician or nurse with expertise in cardiology. Any parameters outside of a normal range resulted in a consultation with a cardiologist for medication adjustments or recommendation for an office visit with a cardiologist. The intervention was performed for 3 months. The following parameters were considered abnormal for this study: heart rate > 100 beats/min; weight increase or decrease > 10% over baseline; systolic blood pressure > 140 mm Hg and/or diastolic blood pressure > 90 mm Hg; oxygen saturation < 92%; and development of new symptoms including angina, dyspnea, palpitations, orthopnea, dizziness, or lightheadedness (presyncope). At each visit (whether in person or virtual), vital signs, patient complaints and concerns, and changes to medications were recorded. Hospital readmissions were documented by interview and review of electronic medical records.
The primary study outcome measure was the frequency of heart failure related to readmission. Our secondary study outcome measures were cardiovascular and all-cause mortality. Follow-up meetings were conducted with all study patients at 1, 3, and 6 months.
Statistical Analysis
Descriptive statistics were generated to characterize the study populations according to demographic factors (age, sex, race, and known cardiovascular risk factors). Continuous variables were described using the mean, standard deviation, and range. Categorical variables were described using frequency distributions. Univariate analysis between groups was performed using Fisher's exact test for binary variables, χ2 tests for categorical variables, and t tests for continuous variables. Linear regression analysis was used to model differences according to age, sex, other demographic factors, or cardiovascular risk factors between study groups for the primary and secondary outcomes. A P value of ≤ .05 was considered statistically significant.
Results
Table 2 summarizes participant demographics. Overall, 28 patients were enrolled; 14 were randomized to the monitored arm and 14 to the control arm. As shown in Table 2, there was no significant difference in comorbid conditions between participants in both arms of the study. The majority of patients were African American: 12 (86%) in the monitored arm and 10 (71%) in the usual care arm (P = .65). However, tobacco use was less common in the monitored group versus the control group (21% vs 57%; P = .05), which was purely by chance.
Table 3 demonstrates the baseline clinical and laboratory characteristics. Figure 1 demonstrates discharge medications among participants in both arms of the study. Again, there was no statistically significant difference between the two arms with regard to N-terminal of the prohormone of brain natriuretic peptide (NT-proBNP) (7094 vs 9994; P = .33), ejection fraction (23.5 vs 22.1; P = .4), implantable cardioverter defibrillator use (9 vs 7; P = .45), and other parameters shown in Table 2.
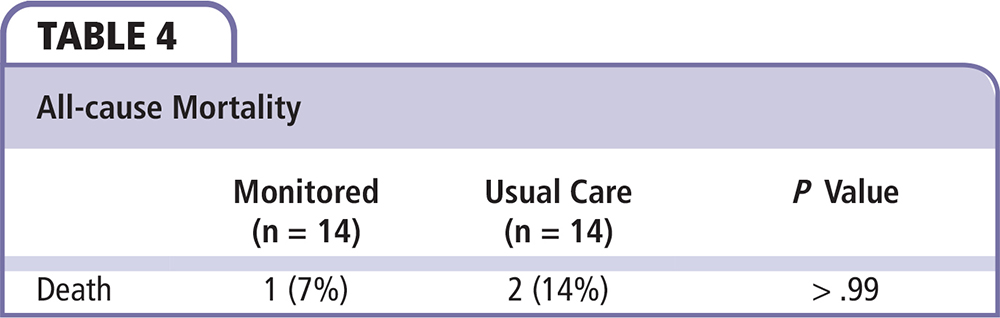
During the 6-month follow-up period, the monitored arm received the weekly teleconferencing intervention for the first 3 months. Figure 2 summarizes the primary and secondary study outcomes. Hospital readmission rates were statistically significant in the first 30 days between the arms (1 in the monitored arm vs 7 in the control arm; P = .03). The one readmission in the monitored arm was due to CHF. In the control arm, four of the seven readmissions were due to CHF. The other three readmissions were due to pneumonia, syncope, and hyperkalemia/acute kidney injury. There were no significant differences in readmission rates between both arms at 3 - or 6-month intervals. This was noted for both cardiac and noncardiac causes of readmission. Furthermore, all-cause mortality (Table 4) was equal between the two arms during the 6-month study period, with 7% in the monitored arm versus 14% in the control arm (P > .99).
Discussion
Telemedicine and telemonitoring technologies have been developed to include a wide range of possible patient-healthcare provider interactions. With advances in the field of information technology, more sophisticated systems continue to be developed. In the home setting, telemonitoring has been utilized for several chronic conditions (including diabetes, hypertension, chronic obstructive pulmonary disease, and cardiovascular disease).8 Among cardiovascular diseases, heart failure stands out as being suitable for the utilization of telemedicine technology. Patients with heart failure have a complicated disease and treatment course with frequent hospitalizations, as well as high disease-related morbidity and mortality rates.9
Studies conducted to examine the impact of telemonitoring on heart failure treatments have shown mixed results. An improvement in the overall survival of 17% to 47% over a 6- to 12-month follow-up and a decrease in the number and duration of hospitalizations after using telemonitoring techniques has been demonstrated in two large meta-analyses.10,11 The validity of these findings has been questioned, as many of the included trials utilized poor study designs (eg, lack of randomization, no control group, relatively small sample size, and vastly different telemonitoring techniques).
Two large randomized controlled trials failed to demonstrate a benefit in hospitalization or survival. In the Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) study,12 patients who were recently admitted to the hospital were randomized to either the telemonitoring (n = 826) or usual care (n = 827) group.12 The telemonitoring group was instructed to call a toll-free number and follow voice-prompted questions regarding symptoms and daily body weight. Certain responses triggered “variances,” which were brought to the attention of a supervising physician who could take appropriate action. A significant difference in hospital readmission or death between the two groups was not detected in the trial. This telemonitoring strategy (entering data via automated telephone prompts) may not be ideal, as the patients play a very passive role and typically do not receive immediate feedback on their clinical progress. In the Telemedical Interventional Monitoring in Heart Failure (TIM-HF) study13 stable patients with chronic heart failure were randomly assigned to either the telemonitoring (n = 354) or usual care (n = 356) groups. A difference in all-cause mortality was not identified. The TIM-HF study used devices with wireless Bluetooth capabilities and a personal data assistant that automatically transmitted data to a telemonitoring center. This method also lacks direct contact between the patient and provider. The TIM-HF study population (patients with stable heart failure) may not be the population that would derive the most benefit from telemonitoring.
Prior applications of telemonitoring were designed around the principle that regular monitoring of physiologic parameters will enable early identification of clinical changes and consequently allow for intervention before decompensation. The Health Connect system provides the added benefit of virtual appointments with healthcare providers. Virtual appointments allow review of telemonitoring data, assessment of symptoms, time for direct patient education, and monitoring of compliance with medications, diet, and office appointments. Most studies on the effects of telemonitoring report a high rate of patient satisfaction.8 An important benefit of telemonitoring appears to be related to patient empowerment. Patients gain insight and awareness into their disease when they are directly involved in the care process. Virtual appointments foster an environment that encourages patient empowerment by offering ideal opportunities for this type of interaction. The addition of virtual appointments truly transforms basic telemonitoring into telemedicine.
Despite the availability of evidence-based pharmacotherapies shown to improve survival and need for hospitalization, nonadherence to prescribed regimens remains a common problem in patients with heart failure. A recent study (N = 557) demonstrated a rate of nonadherence to prescribed treatments of 39% to 65%, depending on the medication.14 Nonadherence was associated with a significantly higher risk of all-cause mortality and cardiovascular hospitalization. The investigators estimated that 23% to 31% of hospital readmissions could have been prevented by improved adherence. It has been suggested that the level of adherence needs to be quite high (> 88%) in order to improve disease-free survival.15 Several factors appear to play a role in these high nonadherence rates. In one study (N = 954), patients with depressive symptoms and poor knowledge of their condition had significant difficulties with adherence.16 The telemedicine system employed in the current study allows clinicians to not only monitor and encourage medication adherence, but also provides an ideal opportunity for patient education, which is a root cause of nonadherence.
A major limitation with traditional telemonitoring is the lack of clinical context for the collected physiologic data. Virtual appointments provide this context and enable clinicians to better determine the most appropriate intervention. For example, a change in a previously stable vital sign may represent medication noncompliance, which may resolve with resumption of the missed medication. If necessary, medication doses can be adjusted or the patient can be referred for an early appointment with his or her cardiologist. Patients should be taken directly to the emergency department if the clinical condition becomes serious or life threatening.
Large, randomized controlled trials that are adequately powered to detect effects on survival and hospitalization are needed to confirm the clinical benefits of this telemedicine system. If the benefits are found to be real, the economic viability of telemedicine over usual care would need to be assessed prior to widespread implementation of this system.
The cost of the device used in our study for telemonitoring was estimated to be $450 per patient per month. It is reasonable to say that this cost can be significantly lower than the cost of rehospitalizations in patients with CHF. As the technology advances, the cost of telemonitoring will decrease accordingly, making it more affordable for the healthcare system.
Conclusions
The Health Connect telemedicine system appears to be acceptable and easy to use for both patients and healthcare providers. The integration of traditional telemonitoring technology with virtual provider appointments offers a powerful tool to improve outcomes in patients with CHF. Further research is required to confirm the clinical benefit and economic viability of the Health Connect system over standard medical therapy. ![]()
The authors report no real or apparent conflicts of interest.
References
- Lloyd-Jones D, Adams RJ, Brown TM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2010 update: a report from the American Heart Association.Circulation. 2010;121:e46-e215.
- Roger VL. Epidemiology of heart failure. Circ Res. 2013;113:646-659.
- Bradley EH, Curry L, Horwitz LI, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6:444-450.
- Gheorghiade M, Braunwald E. Hospitalizations for heart failure in the United States—a sign of hope. JAMA. 2011;306:1705-1706.
- Basoor A, Doshi NC, Cotant JF, et al. Decreased readmissions and improved quality of care with the use of an inexpensive checklist in heart failure. Congest Heart Fail. 2013;19:200-206.
- Ketterer MW, Draus C, McCord J, et al. Behavioral factors and hospital admissions/readmissions in patients with CHF. Psychosomatics. 2014;55:45-50.
- Smith AC. Effect of telemonitoring on re-admission in patients with congestive heart failure. Medsurg Nurs. 2013;22:39-44.
- Paré G, Janna M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc. 2007;14:269-277.
- Masoudi FA, Balillie CA, Wang Y, et al. The complexity and cost of drug regimens of older patients with heart failure in the United States, 1998-2001. Arch Intern Med. 2005;165:2069-2076.
- Klersy C, De Silvestri A, Gabutti G, et al. A metaanalysis of remote monitoring of heart failure patients. J Am Coll Cardiol. 2009;54:1683-1694.
- Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;(8):CD007228
- Chaudhry SI, Mattera JA, Curtis JP, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301-2309.
- Koehler F, Winkler S, Schieber M, et al; Telemedical Interventional Monitoring in Heart Failure Investigators. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation. 2011;123:1873-1880.
- Fitzgerald AA, Powers JD, Ho PM, et al. Impact of medication nonadherence in hospitalizations and mortality in heart failure. J Card Fail. 2011;17: 664-669.
- Wu JR, Moser DK, De Jong MJ, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. Am Heart J. 2009;157:285-291.
- Halpern MT, Khan ZM, Schmier JK, et al. Recommendations for evaluating compliance and persistence with hypertension therapy using retrospective data. Hypertension. 2006;47:1039-1048.