Three-Dimensional Angle Assessment and Plaque Distribution Classification in Left Main Disease: Impact of Geometry on Outcome
Davide Capodanno, MD, PhD, Giuseppe Gargiulo, MD, Giovanni Longo, MD, Corrado Tamburino, MD, PhD
Ferrarotto Hospital, University of Catania, Catania, Italy
Bifurcation geometry and plaque distribution in a diseased left main artery (LM) have the potential to drive operators’ decisions regarding treatment strategies, techniques, and material selection. The three-dimensional (3D) geometry of the LM bifurcation typically results in specific patterns of plaque distribution. Plaque distribution may, in turn, significantly affect the procedural and long-term clinical and angiographic outcomes of LM percutaneous coronary intervention. Each LM bifurcation must be treated according to its unique anatomic and pathologic characteristics. Novel classification schemes of plaque distribution and 3D assessment may be valuable aids to obtaining a working picture of the bifurcation geometry.
[Rev Cardiovasc Med. 2015;16(2): 131-139 doi: 10.3909/ricm0763]
© 2015 MedReviews®, LLC
Three-Dimensional Angle Assessment and Plaque Distribution Classification in Left Main Disease: Impact of Geometry on Outcome
Davide Capodanno, MD, PhD, Giuseppe Gargiulo, MD, Giovanni Longo, MD, Corrado Tamburino, MD, PhD
Ferrarotto Hospital, University of Catania, Catania, Italy
Bifurcation geometry and plaque distribution in a diseased left main artery (LM) have the potential to drive operators’ decisions regarding treatment strategies, techniques, and material selection. The three-dimensional (3D) geometry of the LM bifurcation typically results in specific patterns of plaque distribution. Plaque distribution may, in turn, significantly affect the procedural and long-term clinical and angiographic outcomes of LM percutaneous coronary intervention. Each LM bifurcation must be treated according to its unique anatomic and pathologic characteristics. Novel classification schemes of plaque distribution and 3D assessment may be valuable aids to obtaining a working picture of the bifurcation geometry.
[Rev Cardiovasc Med. 2015;16(2): 131-139 doi: 10.3909/ricm0763]
© 2015 MedReviews®, LLC
Three-Dimensional Angle Assessment and Plaque Distribution Classification in Left Main Disease: Impact of Geometry on Outcome
Davide Capodanno, MD, PhD, Giuseppe Gargiulo, MD, Giovanni Longo, MD, Corrado Tamburino, MD, PhD
Ferrarotto Hospital, University of Catania, Catania, Italy
Bifurcation geometry and plaque distribution in a diseased left main artery (LM) have the potential to drive operators’ decisions regarding treatment strategies, techniques, and material selection. The three-dimensional (3D) geometry of the LM bifurcation typically results in specific patterns of plaque distribution. Plaque distribution may, in turn, significantly affect the procedural and long-term clinical and angiographic outcomes of LM percutaneous coronary intervention. Each LM bifurcation must be treated according to its unique anatomic and pathologic characteristics. Novel classification schemes of plaque distribution and 3D assessment may be valuable aids to obtaining a working picture of the bifurcation geometry.
[Rev Cardiovasc Med. 2015;16(2): 131-139 doi: 10.3909/ricm0763]
© 2015 MedReviews®, LLC
KEY WORDS
Left main bifurcation • Percutaneous coronary intervention • Angles
KEY WORDS
Left main bifurcation • Percutaneous coronary intervention • Angles
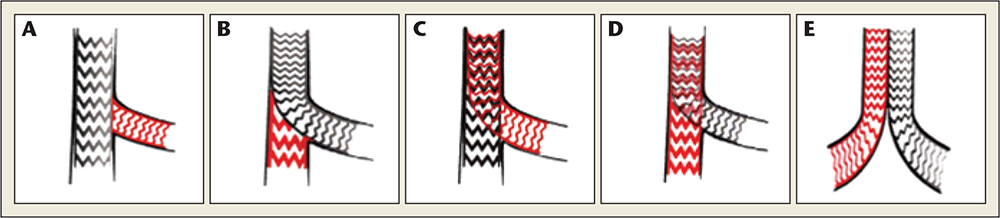
Figure 1. Two-stent techniques for new carina: (A) crush, minicrush, and variants; (B) crush, minicrush, and variants reverse techniques; (C) culotte; (D) reverse culotte; (E) simultaneous kissing stenting. Adapted from Tamburino C, Di Salvo ME.13
A consistent body of literature supports the role of the distal angle B as a predictor of procedural success and long-term clinical outcomes.
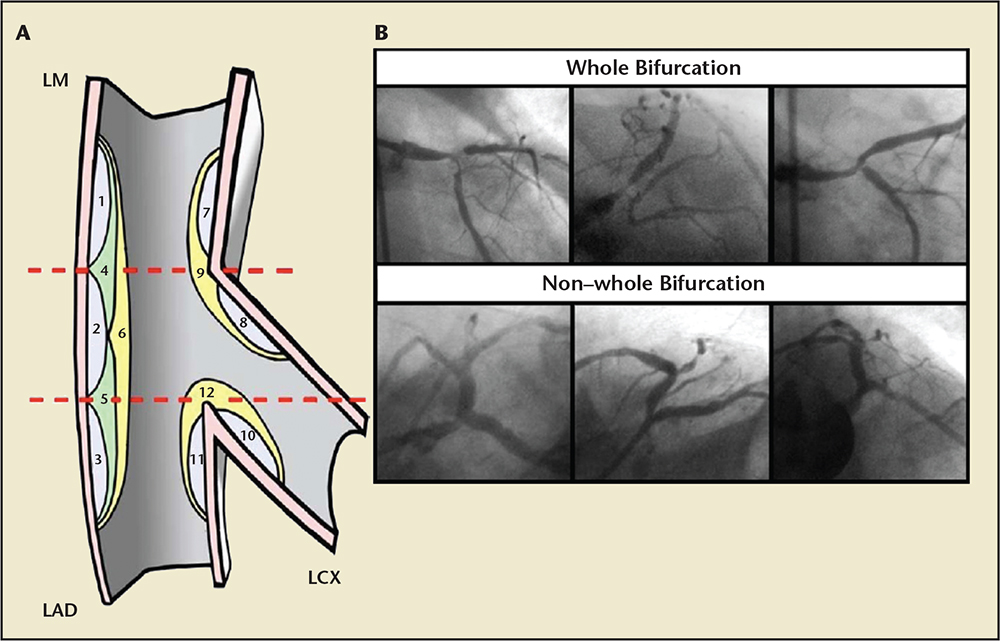
Figure 2. Possible plaque locations at LM bifurcation and distribution patterns. The whole bifurcation involvement is represented by plaque locations 6, 9, and 12 (A), and by the three angiograms at the top (B). The partial bifurcation involvement is represented by plaque locations 1-5, 7, 8, 10, and 11 (A), and by the three angiograms at the bottom (B). LAD, left anterior descending artery; LCX, left circumflex artery; LM, left main artery. Adapted from Tamburino C et al.27
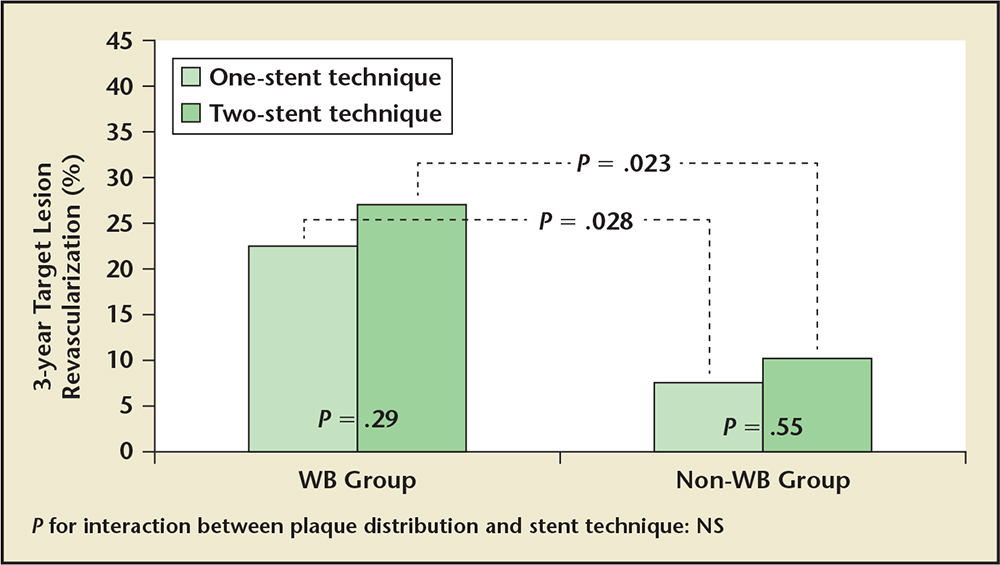
Figure 3. Impact of stent technique and plaque distribution in the study by Tamburino and colleagues.27 The impact of plaque distribution on the incidence of 3-year target lesion revascularization is independent from the stenting technique (P for interaction = NS). NS, nonsignificant; WB, whole bifurcation involvement; non-WB, partial bifurcation involvement.
… IVUS is a well-established tool to improve long-term clinical outcomes in patients undergoing PCI for bifurcation lesions…
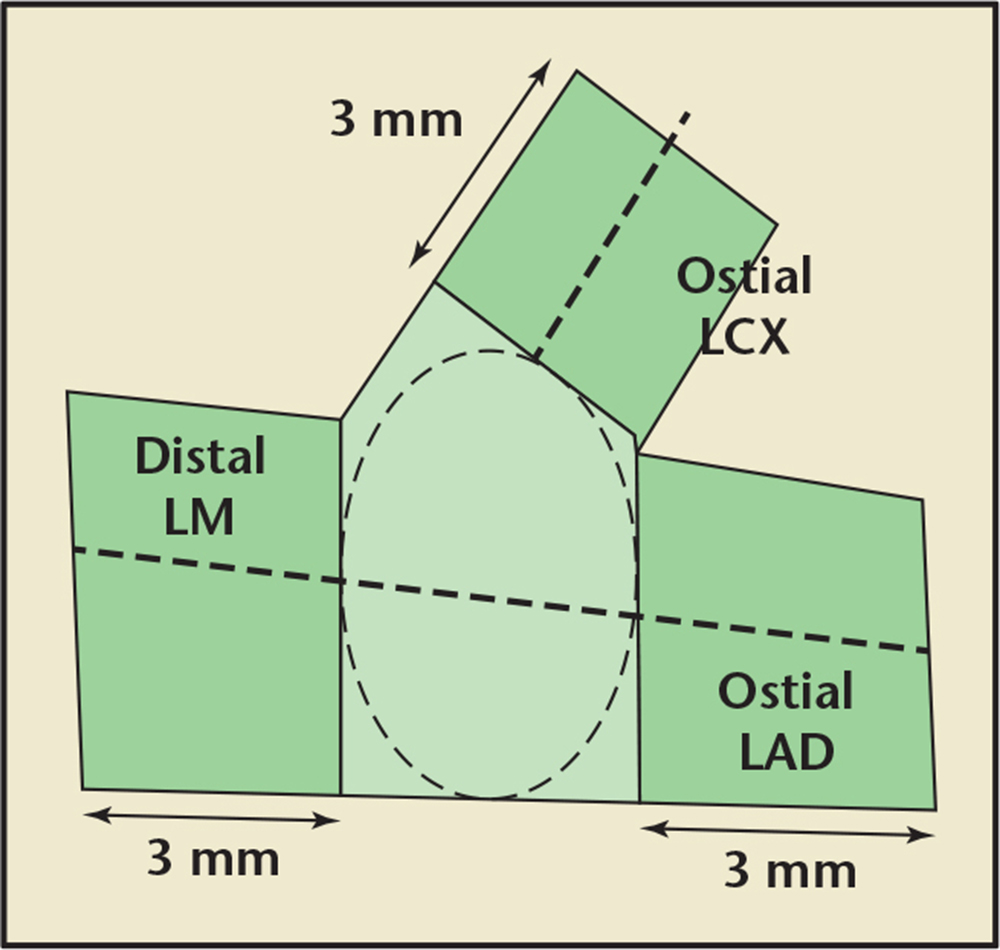
Figure 4. Polygon of confluence in the left main coronary artery. LAD, left anterior descending artery; LCX, left circumflex artery; LM, left main artery. Adapted from Ramcharitar S et al.37
… accurate preprocedural analysis of LM bifurcation and plaque distribution play a crucial role in the planning of PCI strategy.
… the spatial plaque burden and BA should be closely examined before crush stenting, and segments should not be left unstented over large plaques.
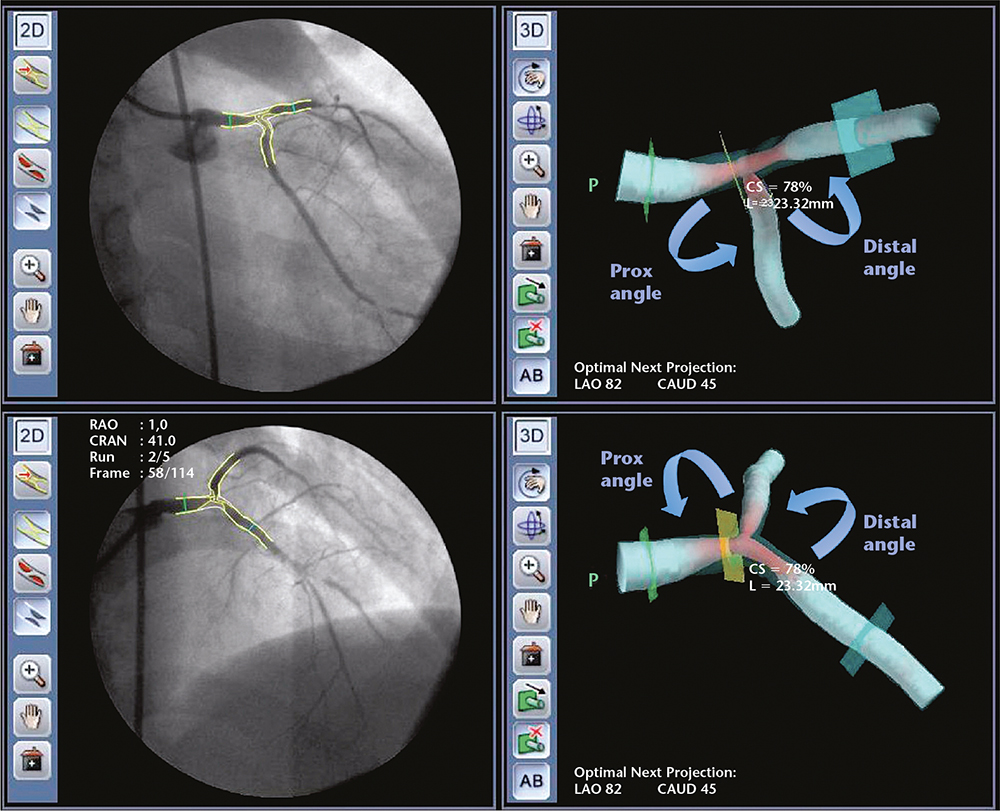
Figure 5. Angiographic images of distal severe left main stenosis involving the left anterior descending and left circumflex arteries with corresponding three-dimensional reconstructions from the integration of two single-plane angiographic images taken from different angles. CAUD, caudal; CRAN, cranial; LAO, left anterior oblique; Prox, proximal; RAO, right anterior oblique.
Main Points
• Bifurcation geometry is known to significantly affect the approach to left main coronary artery (LM) percutaneous coronary intervention (PCI).
• In patients undergoing PCI with drug-eluting stents for unprotected LM disease, distal LM location of disease significantly predict major adverse cardiovascular events and target vessel revascularization.
• The use of intravascular ultrasound is strongly recommended in patients with distal LM lesions, because it is a useful tool when planning the LM bifurcation PCI strategy and optimizes outcomes.
• Three-dimensional quantitative coronary analysis is of great interest and has the potential to overcome the limitations of two-dimensional assessment of the LM by accurately defining the extent, complexity, and length of the lesion, the degree of stenosis, and the reference vessel diameter, thereby allowing a thorough and appropriate assessment of PCI strategy.
Main Points
• Bifurcation geometry is known to significantly affect the approach to left main coronary artery (LM) percutaneous coronary intervention (PCI).
• In patients undergoing PCI with drug-eluting stents for unprotected LM disease, distal LM location of disease significantly predict major adverse cardiovascular events and target vessel revascularization.
• The use of intravascular ultrasound is strongly recommended in patients with distal LM lesions, because it is a useful tool when planning the LM bifurcation PCI strategy and optimizes outcomes.
• Three-dimensional quantitative coronary analysis is of great interest and has the potential to overcome the limitations of two-dimensional assessment of the LM by accurately defining the extent, complexity, and length of the lesion, the degree of stenosis, and the reference vessel diameter, thereby allowing a thorough and appropriate assessment of PCI strategy.
The left main coronary artery (LM) normally arises from the corresponding aortic sinus at a length of 1 to 25 mm, and then bifurcates into the left anterior descending (LAD) and the left circumflex (LCX) arteries. Beyond this classic presentation, a substantial unpredictability exists in the normal and pathologic presentation of the LM, including interindividual variations in take-off, course, length, diameter, and angle.1 The bifurcation geometry is known to significantly affect the approach to LM percutaneous coronary intervention (PCI).2,3 The distribution of plaque in a diseased LM is also recognized as a significant determinant of the operator's preferences on strategies, techniques, and material selection.2,3 This article reviews the growing evidence surrounding the presumptive link among LM bifurcation geometry, plaque distribution, and clinical outcomes of LM PCI. A literature review of focused PubMed searches, online databases, and reference lists of recent publications was performed, and included the following key words: left main, three-dimensional quantitative coronary analysis, bifurcation angles, coronary angioplasty, and percutaneous coronary intervention.
Left Main Bifurcation: Angles, Procedural Techniques, and Outcomes
The bifurcation angles (BAs) pose important and unique technical challenges to the operator. For example, in patients with LM disease located at the distal bifurcation, the angle between the LM and the LCX (proximal angle A) is known to impact the accessibility of the side branch.2,4 Conversely, the angle between the LAD and LCX (distal angle B) has been consistently associated with the likelihood of side branch occlusion during and after stenting of the main branch.2,4 The European Bifurcation Club has consistently advocated the importance of BA measurements for the prediction of procedural outcome.3
A consistent body of literature supports the role of the distal angle B as a predictor of procedural success and long-term clinical outcomes.5-9 In the SYNTAX score, a well-established and validated angiographic tool for stratifying the angiographic risk of patients referred to complex PCI, one additive lesion characteristic added to the bifurcation lesion classification is the presence of a ≤ 70° angle B.10,11 Although this feature may represent a less technical challenge in wiring and stenting, a ≤ 70° angle B is regarded as an adverse lesion characteristic due to the anticipated difficulty in covering the ostium of the side branch when a stent is implanted. When the stent is placed to cover the distal rim of the ostium, the proximal rim will remain uncovered. If the stent is placed to cover the proximal rim, it will protrude into the main vessel. Therefore, bifurcations with a wide angulation between the daughter vessels should be approached with single stent strategies whenever possible.12 This applies equally to the LM bifurcation, which is less likely to have a narrow distal B angle than non-LM bifurcations.1 When a second stent is needed to treat the side branch after stenting the main vessel (bailout stenting), the distal angle B typically influences the strategy of choice. In case of a near 90° distal angle B, T-stenting is generally preferred.13 When both branches are of near equal size and the angle is narrow, the culotte or internal crush techniques are feasible options. Finally, when the LCX is smaller than the LM and LAD and the angle is narrow, T and small protrusion (TAP) or internal crush techniques should be considered.13 When a planned two-stent strategy is elected, T-, modified T-, or TAP techniques are preferred for a 75°- to 90°-angled LCX.13 For Y-shaped bifurcations, the mini-crush (in cases with LAD/LCX diameter mismatch) or culotte (in cases with matched LAD/LCX diameters) techniques are usually selected (Figure 1).13
The Left Main Is a Different Animal: the Issue of Plaque Distribution
Despite the availability of drug-eluting stents and the clinical equipoise of PCI versus CABG in patients with low angiographic complexity,14 stenting on LM bifurcation remains challenging and provides suboptimal outcomes compared with nondistal LM stenting.2,3,15-18 A meta-analysis of 1278 patients undergoing PCI with drug-eluting stents for unprotected LM disease demonstrated that the distal LM location of disease significantly predicted major adverse cardiovascular events and target vessel revascularization, whereas death was predicted from the presence of high-risk features.19 Consequently, based on data from major randomized trials20-24 and some registries, PCI as a means of revascularization for ostial and/or shaft LM stenosis has been upgraded to a class Ha recommendation, whereas LM bifurcation PCI was assigned to a class lib recommendation, being considered at significant higher risk for adverse clinical outcomes compared with surgery.25,26 As previously noted, possible explanations include inherent anatomic and hemodynamic characteristics, along with technical issues. However, the lack of appreciation of the true extent and morphology and the distribution of the atherosclerotic plaque, embracing a broad pattern of localizations in the different segments of the bifurcation, may represent further crucial contributing factors.
In a previous study, Tamburino and colleagues27 investigated the independent association between a specific plaque distribution pattern within the LM bifurcation area and the long-term outcomes of LM PCI. A total of 329 patients undergoing LM bifurcation PCI were evaluated and their angiograms systematically reviewed. Two transversal planes, the first crossing the takeoff of LCX and the second crossing the point of bifurcation, were considered to define the bifurcation as the area included between 2 mm above and below the first and the second plane, respectively (Figure 2). Following this approach, three areas were identified: one above the first plane, one included between the first and second planes, and the third below the second plane (Figure 2). Within these three regions, several different plaque distribution patterns were identified. These were collapsed into two specific groups: the group in which the plaque was extensively located at all three bifurcation regions, defined as whole bifurcation involvement (WB), and the group encompassing all the other plaque distribution scenarios, defined as partial bifurcation involvement (non-WB) (Figure 2). Importantly, differently from the well-established Medina classification,28 the presence of the plaque at each side was attributed regardless of the stenosis degree, but the overall narrowing was > 50% in at least one point of the entire bifurcation area. Interestingly, the WB plaque distribution pattern was associated with higher risk of target lesion revascularization throughout 3 years of follow-up compared with the non-WB pattern (24.9% vs 8.3%; P < .001; adjusted hazard ratio: 2.84; 95% confidence interval, 1.43-5.64; P < .003), independently of other angiographic characteristics, including stenosis degree, vessels, lesions treated, and stent technique (Figure 3). Therefore, within the potential plaque distribution patterns, a specific high-risk LM bifurcation type was identified, in which a greater burden of plaque extensively occupying all the main components of the bifurcation might be responsible for hemodynamic alterations of flow patterns favoring neointimal hyperplasia after stent implantation. Further, a WB patterns might represent a specific anatomic condition hampering correct stent deployment, thus potentially favoring disease progression in a type of plaque that also might have an enhanced intrinsic tendency to progress.
The issue of the location and impact of plaque distribution in the LM bifurcation has been further explored using intravascular ultrasound (IVUS) imaging by Oviedo and colleagues,29 adding meaningfully to the current understanding of the actual spatial distribution of plaque atheroma at the LM bifurcation. In particular, both the LAD and LCX sides of the carina were confirmed to be free from disease, and the most common IVUS pattern involved continuous axial plaque from the distal LM into the proximal LAD and LCX. These results underscore the peculiarity of the LM bifurcation, where the blood flow is slow, and it changes direction with the cardiac cycle, resulting in a weak hemodynamic shear stress. Because atherosclerosis has a predilection for areas with low shear stress and turbulent blood flow, the involvement of the flow divider is generally minimal or absent.30,31 Notably, IVUS is a well-established tool to improve long-term clinical outcomes in patients undergoing PCI for bifurcation lesions,32 not only for post-stent assessment, but also to elucidate the LM anatomy, plaque distribution, and severity of disease.33 In patients with distal LM lesions, the use of IVUS is strongly recommended because it is a useful tool to plan the LM bifurcation PCI strategy and, in turn, to optimize the outcome of these complex procedures.33 Kang and colleagues34 demonstrated that lumen loss at the LCX ostium frequently occurred after crossover stenting from the distal LM to the LAD due to carina shift that was associated with a narrow angle between the LAD and LCX.34 Hence, the assessment of the LCX ostium by direct IVUS LCX pullback is recommended to evaluate accurately the mechanisms of lumen loss during stent implantation and choose the best revascularization strategy.3 However, IVUS requires additional steps and catheters for the procedure, in addition to expertise and major costs. Spoon and colleagues35 compared three-dimensional (3D) quantitative coronary analysis (QCA) reconstruction with IVUS for LM disease, demonstrating a fair agreement of the two techniques in LM measurements (minimal luminal diameter and minimal luminal area [MLA]), but failing in demonstrating an equally adequate concordance in the estimation of plaque burden; notably, this was a single, retrospective, small study conducted in only 55 patients.35
A crucial role of plaque distribution and morphology in the LM bifurcation has also been demonstrated by Yoshitaka Goto and associates,36 who analyzed 80 patients with multidetector row computed tomography underlining the potential for this technique to provide useful information that can predict the eventual side branch compromise during and after LM PCI.
Another concept typically applicable to the LM bifurcation addresses the polygon of confluence (POC), namely the confluent zone of the LAD and LCX arteries just proximal to the carina and the distal LM over the carina37 (Figure 4). The preprocedural MLA within the POC appears to be a surrogate for the overall severity and complexity of LM bifurcation disease. In a study by Kang and coworkers,38 the MLA and the post-stenting minimum stent area were mainly located within the POC, and the preprocedural MLA within the POC was associated with disease severity in the distal LM and in the LAD and LCX ostia. In addition, the preprocedural MLA within the POC significantly correlated with the risk of stent underexpansion and major adverse cardiovascular events at 3-year follow-up. Together, these data support the abovementioned recommendation that an accurate preprocedural analysis of LM bifurcation and plaque distribution play a crucial role in the planning of PCI strategy.
Characterizing the Bifurcation Angle: Shifting From Two-Dimensional to Three-Dimensional Assessment
Despite the remarkable progresses made in recent years in noninva-sive cardiovascular imaging with powerful instruments, such as multislice computed tomography and cardiac magnetic resonance imaging, coronary angiography remains the gold standard for the assessment of epicardial coronary arteries. The geometry of the coronary tree and the complex relationship among its branches can be efficiently reconstructed through the acquisition of two-dimensional (2D) angiograms from different views. However, the 2D QCA of a bifurcation segment suffers from important limitations including foreshortening and vessel overlap. These caveats may result in errors when assessing the actual length of the coronary artery branches, their dimension, and the presence and severity of luminal narrowing. In addition, 2D images hamper the ability to fully appreciate the vessel curvature and the take-off angles at the carina, which are key in the study of hemodynamic factors associated with atherosclerosis and for choosing the interventional approach to treat a bifurcation lesion. In the LM, the drawbacks of 2D QCA are magnified for several reasons, including its direct origin from the aorta, shortness, variable course, plaque distribution, the concealment of diffuse atherosclerosis due to arterial remodeling, the distinct lack of a reference segment, issues of catheter placement, and contrast streaming in the case of ostial disease. To further make LM angiographic evaluation unique and complex, the possibility of the LM to exhibit reverse tapering should be considered—that the LM ostium has a smaller caliper compared with its distal segment in the absence of atherosclerosis.39 Interestingly, in support of this hypothesis, initial experiences indicated significant discrepancies between angiographic estimates of stenosis severity and findings at autopsy,40 which was also confirmed in vivo through the use of IVUS41 and the analysis of experienced interventionalists, and showed poor agreement and high interobserver variability.33
Moreover, it should also be considered that to obtain the optimal views, interventionalists will interactively adjust the rotation angle (left anterior oblique/right anterior oblique) and the angulation angle (cranial/caudal) guided by the radiographic images. However, this approach could significantly increase contrast medium volume used and radiation exposure. Furthermore, due to variable anatomy and variable heart orientation in the thorax, the chosen angle can be quite different from the true optimal viewing angle.
Initial experience studying the expansion and deformity of the stents after crush stenting in a silicon tube 3D model of LM bifurcation—with a view to determine the impact of the 3D structure on the outcome of crush stenting—demonstrated that overlap of the LAD stent over (as opposed to under) the LCX stent was associated with close apposition of the stent to the vessel on the myocardial side, at the ostium of the LCX artery, where atherosclerotic plaques are likely to be present. This evidence led the author to conclude that the spatial plaque burden and BA should be closely examined before crush stenting, and segments should not be left unstented over large plaques.9
Recently, Onuma and colleagues42 and Girasis and colleagues43 validated the 3D reconstruction and QCA for bifurcation lesions; they reported accurate, precise, and reproducible measures of diameter, length, and BA. Importantly, the impact of BA on immediate post-procedural and long-term outcomes has been evaluated in non-LM bifurcations.5-7 Also the role of this technique in evaluating post-PCI results of bifurcation PCI has been proven.4,44,45 Therefore, 3D QCA is of great interest and has the potential to overcome the limitations of 2D assessment of the LM by accurately defining the extent, complexity, and length of the lesion, the degree of stenosis, and the reference vessel diameter, thereby allowing a thorough and appropriate assessment of the indication for PCI, and offering guidance in the material selection.46-49 The 3D-rendered images of the LM bifurcation can be freely rotated in space, allowing for a precise analysis of the vessels from different viewpoints, and for the assessment of the LM and its side branches, as well as the take-off angles (Figure 5).4,49 Dvir and associates50 demonstrated that 3D reconstructions significantly improved morphologic analysis of LM disease, particularly for ostial and bifurcation lesions.
In a 3D QCA study by Rubinshtein and coworkers,51 133 patients with no angiographically detected coronary artery disease and 70 patients with LM disease were analyzed; 3D QCA was first performed on patients with no coronary artery disease to characterize the normal LM anatomy. The proximal A and distal B BAs had mean values of 116° ± 22° and 74° ± 25°, respectively. Conversely, in patients with LM disease, the proximal and distal BAs were 107° ± 25° and 84° ± 24°, respectively. The magnitude of the distal angle was found to be associated with several clinical and anatomic factors, including the presence of distal LM disease. Therefore, this study supports the understanding that the distal angle B may be increased in patients with bifurcation LM disease. Indeed, whether this difference is the cause of the plaque location at the LM bifurcation, or rather the consequence, remains unclear.
In a study from Godino and associates,52 the correlation between BAs and procedural outcomes of PCI was further investigated. In 75 LM bifurcations, the baseline mean values of the proximal A and distal B angles were 131° ± 32° and 78° ± 28°, respectively. In LM bifurcations treated with two stents the distal angle B significantly decreased by a mean of 10° (P = .003) and the proximal angle A increased by 10° (P = .006). The greatest variation in the A and B angles was found following a two-stent techniques performed in T-shaped (≥ 70°) bifurcations. The crush technique was associated with the largest decrease of the distal angle B, particularly in nontrue bifurcations. These findings underscore that especially in LM bifurcations treated with two stents, the distal B angle became narrower mainly at the expense of the proximal angle A, which became wider.
The feasibility of assessing the LM BA with a 3D QCA algorithm has been further explored by Girasis and colleagues4 in 354 LM patients enrolled in the Synergy Between PCI With TAXUS and Cardiac Surgery (SYNTAX) trial.4 For the purposes of the analysis, the LCX was designated as the side branch and the LM bifurcation was defined as Y-shaped when the distal angle B was < 70°. The 3D QCA analysis was feasible in a relatively high (75.1%) proportion of patients. Suboptimal analyses were due to inadequate cineangiography or difficult anatomy, lacking a proper demarcation of the bifurcation. In patients with completely analyzable rendered images (N = 266), the distal and proximal BAs were inversely correlated and followed a normal distribution with a high grade of interindividual variability. The proximal angle A and the distal angle B had mean pre-PCI end-diastolic values of 106° ± 22° and 96° ± 24°, respectively, and pre-PCI end-systolic mean values of 114° ± 20° and 87° ± 23°, respectively. This finding underscores that cardiac motion significantly affects the LM BAs, including an increase of the proximal angle A and a decrease of the distal angle B. After PCI, the proximal angle A and distal angle B were found to slightly increase and decrease, respectively, consistently with the findings of Godino and colleagues.52 However, in analyses restricted to Y-shaped LM bifurcations, the opposite phenomenon was observed.
Interestingly, the authors analyzed the 12-month freedom from major adverse cardiac or cerebrovascular events (MACCE) after stratification by tertiles of the distal angle B. Theoretically, in LM bifurcations treated with the crush technique, a wide distal angle B may be associated with less optimal expansion and apposition of the side branch stent, especially at the site of the ostium. Conversely, a narrow distal angle B could negatively affect the outcome of the culotte technique due to the increased stent cell size necessary to span an oblique ostium. However, no differences in clinical outcomes were noted across different groups, regardless of whether diastolic or systolic values were analyzed or whether one or two stents were used. Given the small sample size and the retrospective nature of their study, the authors concluded that the potential long-term predictive value of BA assessment and its prospective applicability during PCI deserve further investigation. Recently, the same authors reported on the 5-year outcomes of the 266 patients eligible for the analysis and confirmed that stratification across pre-PCI diastolic distal BA tertiles (< 82°, 82°-106°, ≥ 107°) failed to show any difference in MACCE rates.45 Interestingly, patients with bifurcation disease and post-PCI systolic-diastolic range < 10° had significantly higher MACCE rates (50.8% vs 22.7%; P < .001), and a post-PCI systolic-diastolic range < 10° was an independent predictor of MACCE, demonstrating the crucial role of the unprotected LM post-PCI 3D reconstruction of the bifurcation geometry on the patient's prognosis. However, despite this latter study, which did not identify 3D-QCA pre-PCI as a significant predictor, based on its retrospective analysis, it cannot be excluded that a LM bifurcation PCI guided from the 3D analysis could lead to different results; thus, to date whether pre-PCI 3D QCA is able to significantly impact on prognosis remains still unclear, but there can be yet hypothesized a potential role of this imaging on guiding distal LM PCI and ameliorating outcomes. Further studies to address this issue are needed.
Conclusions
Compared with non-LM bifurcations, the LM bifurcation has peculiar anatomic characteristics, including a wider carina and a larger distal angle. The 3D geometry of the LM bifurcation typically results in specific patterns of plaque distribution. Plaque distribution may in turn significantly affect the procedural and long-term clinical and angiographic outcomes of LM PCI. Therefore, each LM bifurcation must be approached and treated according to its unique anatomic and pathologic characteristics. Novel classification schemes of plaque distribution and 3D assessment may be valuable aids to get a working picture of the bifurcation geometry. ![]()
The authors report no real or apparent conflicts of interest.
References
- Capodanno D, Di Salvo ME, Seminara D, et al. Epidemiology and clinical impact of different anatomical phenotypes of the left main coronary artery. Heart Vessels. 2011;26:138-144.
- Capodanno D, Calvi V, Tamburino C. A focused update on emerging prognostic determinants in distal left main percutaneous coronary intervention. Int J Cardiol. 2012;160:4-7.
- Stankovic G, Lefèvre T, Chieffo A, et al; European Bifurcation Club. Consensus from the 7th European Bifurcation Club meeting. EuroIntervention. 2013;9:36-45.
- Girasis C, Serruys PW, Onuma Y, et al. 3-Dimensional bifurcation angle analysis in patients with left main disease: a substudy of the SYNTAX trial (SYNergy Between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery). JACC Cardiovasc Interv. 2010;3:41-48.
- Collins N, Seidelin PH, Daly P, et al. Long-term outcomes after percutaneous coronary intervention of bifurcation narrowings. Am J Cardiol. 2008;102:404- 410.
- Dzavik V, Kharbanda R, Ivanov J, et al. Predictors of long-term outcome after crush stenting of coronary bifurcation lesions: importance of the bifurcation angle. Am Heart J. 2006;152:762-769.
- Adriaenssens T, Byrne RA, Dibra A, et al. Culotte stenting technique in coronary bifurcation disease: angiographic follow-up using dedicated quantitative coronary angiographic analysis and 12-month clinical outcomes. Eur Heart J. 2008;29:2868-2876.
- Ormiston JA, Currie E, Webster MW, et al. Drugeluting stents for coronary bifurcations: insights into the crush technique. Catheter Cardiovasc Interv. 2004;63:332-336.
- Murasato Y. Impact of three-dimensional characteristics of the left main coronary artery bifurcation on outcome of crush stenting. Catheter Cardiovasc Interv. 2007;69:248-256.
- Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-227.
- Capodanno D, Tamburino C. Integrating the Synergy between percutaneous coronary intervention with Taxus and Cardiac Surgery (SYNTAX) score into practice: use, pitfalls, and new directions. Am Heart J. 2011;161:462-470.
- Hildick-Smith D, Lassen JF, Albiero R, et al. Consensus from the 5th European Bifurcation Club meeting. EuroIntervention. 2010;6:34-38.
- Tamburino C, Di Salvo ME. Left Main Coronary Artery Disease: A Practical Guide for the Interventional Cardiologist. Milan, Italy: Springer-Verlag;2009.
- Capodanno D, Stone GW, Morice MC, et al. Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of randomized clinical data. J Am Coll Cardiol. 2011;58:1426-1432.
- Valgimigli M, Malagutti P, Rodriguez-Granillo GA, et al. Distal left main coronary disease is a major predictor of outcome in patients undergoing percutaneous intervention in the drug-eluting stent era: an integrated clinical and angiographic analysis based on the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) and Taxus-Stent Evaluated At Rotterdam Cardiology Hospital (TSEARCH) registries. J Am Coll Cardiol. 2006;47:1530- 1537.
- Baim DS, Mauri L, Cutlip DC. Drug-eluting stenting for unprotected left main coronary artery disease: are we ready to replace bypass surgery? J Am Coll Cardiol. 2006;47:878-881.
- Palmerini T, Sangiorgi D, Marzocchi A, et al. Ostial and midshaft lesions vs. bifurcation lesions in 1111 patients with unprotected left main coronary artery stenosis treated with drug-eluting stents: results of the survey from the Italian Society of Invasive Cardiology. Eur Heart J. 2009;30:2087-2094.
- Chieffo A, Park SJ, Valgimigli M, et al. Favorable longterm outcome after drug-eluting stent implantation in nonbifurcation lesions that involve unprotected left main coronary artery: a multicenter registry. Circulation. 2007;116:158-162.
- Biondi-Zoccai GG, Lotrionte M, Moretti C, et al. A collaborative systematic review and meta-analysis on 1278 patients undergoing percutaneous drug-eluting stenting for unprotected left main coronary artery disease. Am Heart J. 2008;155:274-283.
- Buszman PE, Kiesz SR, Bochenek A, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol. 2008;51:538-545.
- Serruys PW, Morice MC, Kappetein AP, et al; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360: 961-972.
- Morice MC, Serruys PW, Kappetein AP, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121:2645-2653.
- Park SJ, Kim YH, Park DW, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011;364:1718-1727.
- Boudriot E, Thiele H, Walther T, et al. Randomized comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol. 2011;57:538-545.
- Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31: 2501-2555.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-e122.
- Tamburino C, Capranzano P, Capodanno D, et al. Plaque distribution patterns in distal left main coronary artery to predict outcomes after stent implantation. JACC Cardiovasc Interv. 2010;3:624-631.
- Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions [in Spanish]. Rev Esp Cardiol. 2006;59:183.
- Oviedo C, Maehara A, Mintz GS, et al. Intravascular ultrasound classification of plaque distribution in left main coronary artery bifurcations: where is the plaque really located? Circ Cardiovasc Interv. 2010;3: 105-112.
- Kimura BJ, Russo RJ, Bhargava V, et al. Atheroma morphology and distribution in proximal left anterior descending coronary artery: in vivo observations. J Am Coll Cardiol. 1996;27:825-831.
- Nakazawa G, Yazdani SK, Finn AV, et al. Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55: 1679-1687.
- Kim JS, Hong MK, Ko YG, et al. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a Korean multicenter bifurcation registry. Am Heart J. 2011;161:180-187.
- Puri R, Kapadia SR, Nicholls SJ, et al. Optimizing outcomes during left main percutaneous coronary intervention with intravascular ultrasound and fractional flow reserve: the current state of evidence. JACC Cardiovasc Interv. 2012;5:697-707.
- Kang SJ, Mintz GS, Kim WJ, et al. Changes in left main bifurcation geometry after a single-stent crossover technique: an intravascular ultrasound study using direct imaging of both the left anterior descending and the left circumflex coronary arteries before and after intervention. Circ Cardiovasc Interv. 2011;4:355-361.
- Spoon DB, Rubinshtein R, Psaltis PJ, et al. Comparison between three-dimensional angiographic reconstruction and intravascular ultrasound: imaging of the left main coronary artery. Catheter Cardiovasc Interv. 2013;81:1156-1161.
- Yoshitaka Goto Y, Kawasaki T, Koga N, et al. Plaque distribution patterns in left main trunk bifurcations: prediction of branch vessel compromise by multidetector row computed topography after percutaneous coronary intervention.EuroIntervention. 2012;8: 708-716.
- Ramcharitar S, Onuma Y, Aben JP, et al. A novel dedicated quantitative coronary analysis methodology for bifurcation lesions. EuroIntervention. 2008;3:553-557.
- Kang SJ, Mintz GS, Kim WJ, et al. Effect of intravascular ultrasound findings on long-term repeat revascularization in patients undergoing drug-eluting stent implantation for severe unprotected left main bifurcation narrowing. Am J Cardiol. 2011;107: 367-373.