The Clot Thickens: Unusual Presentation of a Left Atrial Thrombus
Stephen F. Lau, MD,1 James S. Hood, MD,2 Dorinna D. Mendoza, MD,3 Carolyn Yi Li, MD,4 Maria Ansari, MD,5 Jamal S. Rana, MD, PhD3,6
1Department of Internal Medicine, Kaiser Permanente Oakland Medical Center, Oakland, CA; 2Department of Cardiothoracic Surgery, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 3Department of Cardiology, Kaiser Permanente Oakland Medical Center, Oakland, CA; 4Department of Pathology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 5Department of Cardiology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 6Department of Medicine, University of California, San Francisco, San Francisco, CA
Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality. Transesophageal echocardiography is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity of up to 100% and 99%, respectively. Cardiac magnetic resonance imaging has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi. This is an unusual case of a large, free-floating atrial thrombus with a cystic appearance that was surgically removed. The echocardiographic appearance of the cystic atrial mass led to the consideration of another potential etiology for a cardiac mass, namely, atrial myxoma. Histopathologic analyses of the mass led to the final diagnosis of an atrial thrombus.
[Rev Cardiovasc Med. 2015;16(1):81-83 doi: 10.3909/ricm0745]
© 2015 MedReviews®, LLC
The Clot Thickens: Unusual Presentation of a Left Atrial Thrombus
Stephen F. Lau, MD,1 James S. Hood, MD,2 Dorinna D. Mendoza, MD,3 Carolyn Yi Li, MD,4 Maria Ansari, MD,5 Jamal S. Rana, MD, PhD3,6
1Department of Internal Medicine, Kaiser Permanente Oakland Medical Center, Oakland, CA; 2Department of Cardiothoracic Surgery, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 3Department of Cardiology, Kaiser Permanente Oakland Medical Center, Oakland, CA; 4Department of Pathology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 5Department of Cardiology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 6Department of Medicine, University of California, San Francisco, San Francisco, CA
Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality. Transesophageal echocardiography is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity of up to 100% and 99%, respectively. Cardiac magnetic resonance imaging has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi. This is an unusual case of a large, free-floating atrial thrombus with a cystic appearance that was surgically removed. The echocardiographic appearance of the cystic atrial mass led to the consideration of another potential etiology for a cardiac mass, namely, atrial myxoma. Histopathologic analyses of the mass led to the final diagnosis of an atrial thrombus.
[Rev Cardiovasc Med. 2015;16(1):81-83 doi: 10.3909/ricm0745]
© 2015 MedReviews®, LLC
The Clot Thickens: Unusual Presentation of a Left Atrial Thrombus
Stephen F. Lau, MD,1 James S. Hood, MD,2 Dorinna D. Mendoza, MD,3 Carolyn Yi Li, MD,4 Maria Ansari, MD,5 Jamal S. Rana, MD, PhD3,6
1Department of Internal Medicine, Kaiser Permanente Oakland Medical Center, Oakland, CA; 2Department of Cardiothoracic Surgery, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 3Department of Cardiology, Kaiser Permanente Oakland Medical Center, Oakland, CA; 4Department of Pathology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 5Department of Cardiology, Kaiser Permanente San Francisco Medical Center, San Francisco, CA; 6Department of Medicine, University of California, San Francisco, San Francisco, CA
Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality. Transesophageal echocardiography is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity of up to 100% and 99%, respectively. Cardiac magnetic resonance imaging has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi. This is an unusual case of a large, free-floating atrial thrombus with a cystic appearance that was surgically removed. The echocardiographic appearance of the cystic atrial mass led to the consideration of another potential etiology for a cardiac mass, namely, atrial myxoma. Histopathologic analyses of the mass led to the final diagnosis of an atrial thrombus.
[Rev Cardiovasc Med. 2015;16(1):81-83 doi: 10.3909/ricm0745]
© 2015 MedReviews®, LLC
KEY WORDS
Atrial thrombus • Atrial myxoma • Transesophageal echocardiography • Cardiac magnetic resonance imaging • Histopathology
KEY WORDS
Atrial thrombus • Atrial myxoma • Transesophageal echocardiography • Cardiac magnetic resonance imaging • Histopathology
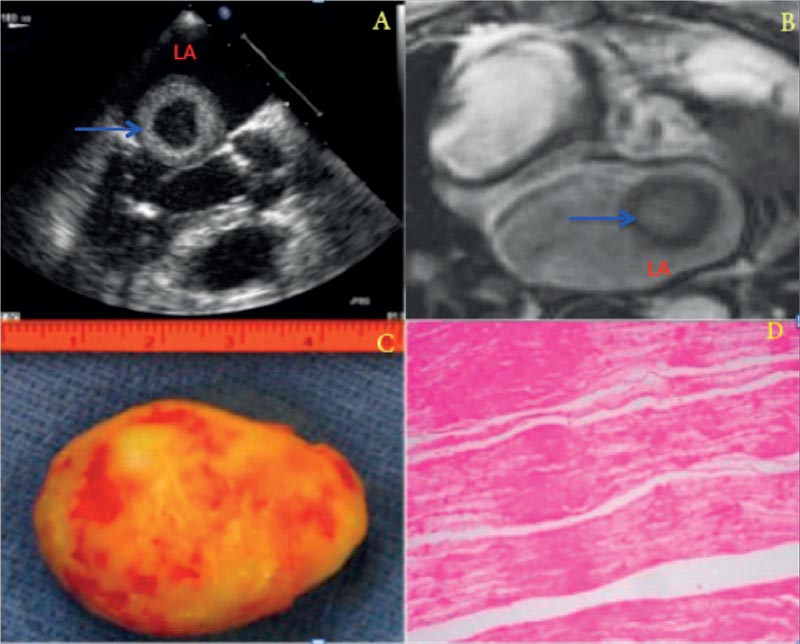
Figure 1. (A) Transesophageal echocardiogram showing the large cystic mass (blue arrow) in the left atrium (LA). (B) Cardiac magnetic resonance image (T2-weighted image) showing a free-floating mass with a central core (blue arrow) in the left atrium (LA). (C) Macroscopic gross appearance of the cardiac mass (4.5 3 4.0 3 3.5 cm, approximately 20 g). (D) Microscopic appearance showing organized thrombi with fibrin and exceedingly rare histiocytes.
Steady-state free-precession images showed a severely dilated left atrium (38 cm2) containing a 3.6 cm × 3.3 cm × 3.4 cm spherical highly mobile free-floating mass with a central core.
Main Points
• Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality; the left atrial appendage is most commonly associated with atrial thrombus formation, particularly in the setting of atrial fibrillation.
• The sensitivity of transthoracic echocardiography for the visualization of left atrial thrombi has been studied to range from 40% to 60%, and is limited. Transesophageal echocardiography is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity of up to 100% and 99%, respectively.
• Although echocardiography has been well studied as a sensitive tool for the detection of atrial myxomas, its use in discriminating between cardiac tumors and other cardiac masses, including atrial thrombi, is limited.
• Cardiac magnetic resonance imaging has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi.
• Histopathologic confirmation may still be required when typical imaging characteristics are not present.
Main Points
• Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality; the left atrial appendage is most commonly associated with atrial thrombus formation, particularly in the setting of atrial fibrillation.
• The sensitivity of transthoracic echocardiography for the visualization of left atrial thrombi has been studied to range from 40% to 60%, and is limited. Transesophageal echocardiography is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity of up to 100% and 99%, respectively.
• Although echocardiography has been well studied as a sensitive tool for the detection of atrial myxomas, its use in discriminating between cardiac tumors and other cardiac masses, including atrial thrombi, is limited.
• Cardiac magnetic resonance imaging has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi.
• Histopathologic confirmation may still be required when typical imaging characteristics are not present.
An 80-year-old woman with history of longstanding persistent atrial fibrillation presented to the emergency department (ED) with a 2-day history of weakness. Two weeks prior, the patient presented to the ED with acute right lower extremity pain and was found to have a large occlusive thrombus in the distal common femoral artery extending into the superficial femoral artery. The International Normalized Ratio (INR) was supratherapeutic at 4.7 at that time. Subsequently, the patient underwent successful emergent endarterectomy. No cardiac imaging was performed during that hospital admission.
During this admission, her blood pressure was 90/50 mm Hg, her pulse was 90 beats/min, and her respiratory rate was 16 breaths/ min. The lungs were clear to auscultation bilaterally. A soft, extra heart sound was heard after diastole, most prominent over the cardiac apex. Laboratory studies were significant for a leukocyte count of 24,000/uL, and urinalysis revealed large leukocyte ester-ase with a leukocyte count of 150/ high-power field. Her INR was 1.8 despite having been administered warfarin. The 12-lead electrocardiogram revealed atrial fibrillation and a right bundle branch block. The chest radiograph showed no acute cardiopulmonary findings. Intravenous antibiotics and several liters of isotonic fluids were administered for sepsis with a suspected urinary source of infection. On hospital day 1, she developed respiratory distress. Her respiratory rate was 26 breaths/min with diffuse crackles auscultated over the lung bases. A repeat chest radiograph revealed diffuse interstitial edema.
Transthoracic echocardiography (TTE) during this admission revealed a large, mobile mass within the left atrium. Transesophageal echocardiography (TEE) confirmed a nonpedunculated, highly mobile mass with an echolucent core in the left atrium (Figure 1A). The mass abutted against the mitral valve during diastole. The mitral valve apparatus was intact without significant hemodynamic changes and there was only trace mitral regurgitation. There was also evidence of spontaneous echocardiographic contrast. No thrombus was noted in the left atrial appendage. The intraatrial septum was intact. Due to the patient's atrial fibrillation and tachypnea, a limited cardiac magnetic resonance imaging (MRI) study without gadolinium administration was performed. Steady-state free-precession images showed a severely dilated left atrium (38 cm2) containing a 3.6 cm × 3.3 cm × 3.4 cm spherical highly mobile free-floating mass with a central core (Figure 1B). On several planes, the mass appeared to float toward the mitral annulus, likely causing partial obstruction of mitral inflow. A coronary angiogram showed diffuse coronary artery disease but no evidence of neovascularization to the left atrial mass. The patient underwent removal of the mass via sternotomy and left atriotomy using cardiopulmonary bypass. A bypass graft was performed to the left anterior descending artery. A 4.5 × 4.0 × 3.5 cm free-floating encapsulated rubbery mass was delivered from the left atrium using a large spoon (Figure 1C). The remainder of the left atrium was inspected for additional masses or stalks and none were visualized. The patient's postoperative course was uneventful. Microscopic examination of the mass revealed organized thrombi with fibrin and exceedingly rare histiocytes (Figure 1D). Of note, the entire specimen was subjected to microscopic examination with a total of 29 slides, all with histologic features consistent with a left atrial thrombus.
Discussion
Left atrial thrombi are a significant cause of cardioembolic morbidity and mortality.1 The left atrial appendage is the site most commonly associated with atrial thrombus formation, particularly in the setting of atrial fibrillation. The sensitivity of TTE for the visualization of left atrial thrombi has been studied to range from 40% to 60%, and is limited.2 TEE is the preferred method for complete visualization of atrial thrombi, and has a sensitivity and specificity as high as 100% and 99%, respectively.3 This high specificity reflects the typical appearance of left atrial thrombi as echocardiographically dense masses, distinct from underlying endocardium and observed in more than one imaging plane.4
Atrial thrombi rarely present with a cystic appearance. Cystic cardiac masses offer a more limited differential diagnosis, including hydatid cysts, bronchogenic cysts, intracardiac varices, and atrial myxomas.5 Although echocardiography has been well studied as a sensitive tool for the detection of atrial myxomas, its use in discriminating between cardiac tumors and other cardiac masses, including atrial thrombi, is limited. Cardiac MRI has been shown to be useful in identifying tissue characteristics that may aid in differentiating between atrial myxoma and thrombi. Atrial myxomas may appear hypointense relative to myocardium on Tl-weighted cine images, and have an overall heterogeneous quality. Atrial thrombi may appear brighter than myocardium in contrast-enhanced images.6 Additionally, atrial myxomas are highly vascularized and identification of neovascularization on coronary angiography is suggestive of the diagnosis. However, neovascularization is only seen in one-third to one-half of cases, and the use of coronary angiography has largely been limited to preoperative identification of concomitant coronary artery disease.7,8
This is an unusual case of a large, free-floating atrial thrombus with a cystic appearance seen on both TTE and TEE. Although prior studies report high specificity of TEE for the detection of atrial thrombi, the echocardiographic appearance of the cystic atrial mass led to the consideration of other potential etiologies for a cardiac mass, namely, atrial myxoma. Cardiac MRI and coronary angiography may be useful in determining the etiology of cardiac masses; however, histopathologic confirmation may still be required when typical imaging characteristics are not present. ![]()
References
- Leung DY, Davidson PM, Cranney GB, Walsh WF. Thromboembolic risks of left atrial thrombus detected by transesophageal echocardiogram. Am J Cardiol. 1997;79:626-629.
- Otto CM. Textbook of Clinical Echocardiography. 4th ed. Philadelphia, PA: Saunders Elsevier; 2009.
- Manning WJ, Weintraub RM, Waksmonski CA, et al. Accuracy of transesophageal echocardiography for identifying left atrial thrombi. A prospective, intraoperative study. Ann Intern Med. 1995;123:817-822.
- Fatkin D, Kuchar DL, Thorburn CW, Feneley MP. Transesophageal echocardiography before and during direct current cardioversion of atrial fibrillation: evidence for “atrial stunning” as a mechanism of thromboembolic complications. J Am Coll Cardiol. 1994;23:307-316.
- Park J, Song JM, Shin E, et al. Cystic cardiac mass in the left atrium: hemorrhage in myxoma. Circulation. 2011;123:e368-e369.
- Rahmanian PB, Castillo JG, Sanz J, et al. Cardiac myxoma: preoperative diagnosis using a multimodal imaging approach and surgical outcome in a large contemporary series. Interact Cardiovasc Thorac Surg. 2007;6:479-483.
- Van Cleemput J, Daenen W, De Geest H. Coronary angiography in cardiac myxomas: findings in 19 consecutive cases and review of the literature. Cathet Cardiovasc Diagn. 1993;29:217-220.
- Janas R, Jutley RS, Fenton P, Sarkar P. Should we perform preoperative coronary angiography in all cases of atrial myxomas? Catheter Cardiovasc Interv. 2006;67:379-383.